Fig. 33.1
Long-term clinical consequences of a ruptured implant as a result of a patient’s negligence showing bilateral breast deformity
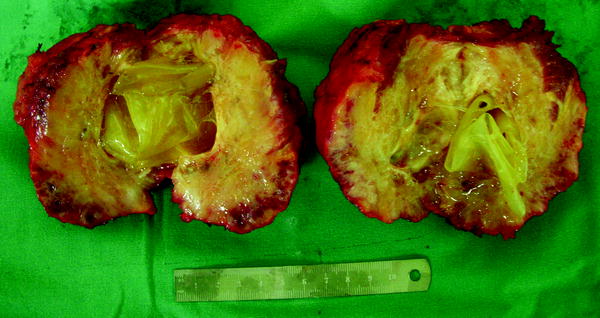
Fig. 33.2
Silicone bilaterally infiltrating breast tissue (explanted from the patient in the Fig. 33.1)

Fig. 33.3
Bilateral rupture 4 years after immediate breast reconstruction with form-stable anatomic breast implants
Ultrasonography has a low sensitivity to detect silicone implant rupture. According to Caskey et al. [15], 41 % of women with implant rupture have no detectable changes on ultrasonography. The most reliable sign of extracapsular rupture is a group of focal nodules with a generalized increase in echogenicity of the breast tissue and loss of normal parenchymal interface resulting from dispersion of the ultrasound beam [16]. The nodules are silicone granulomas. Many of them are located in the axillae.
MRI is the most accurate technique in the evaluation of implant integrity. Its sensitivity for rupture is between 80 and 90 %, and its specificity is between 90 and 97 % (Figs. 33.4 and 33.5). The use of contrast agents in MRI studies for assessment of breast implant integrity is not recommended. Silicone leakage progressing to herniation of silicone within the fibrous capsule, migration from the intracapsular space into the surrounding tissue, or progression of extracapsular silicone can be observed by MRI. There is no increase in autoantibody levels and no increase in reported breast hardness. Normally women do not have visible breast changes and do not have significant clinical symptoms. Thus, MRI is the gold standard to detect and follow-up breast implant ruptures, and the linguine sign is often present with extracapsular ruptures [17, 18]. Mammography is of little value in the assessment of implant integrity, although it may be useful for the assessment of the surrounding breast tissue. Several cases of silicone implant rupture from compression during a mammogram have been reported. They most probably occurred in women who had intracapsular ruptures previous to the mammogram.
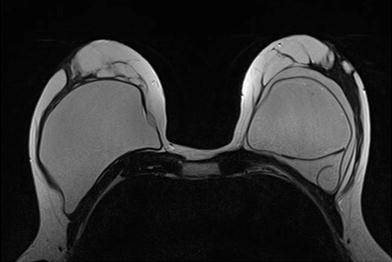
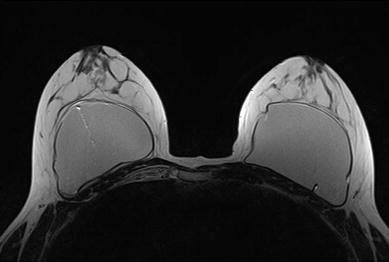
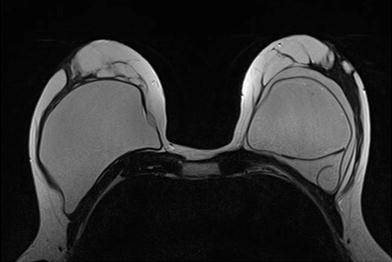
Fig. 33.4
Magnetic resonance image showing intracapsular rupture in a second-generation implant in the left breast (linguine sign)
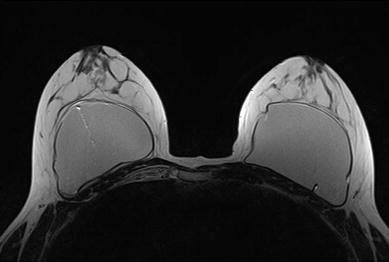
Fig. 33.5
Magnetic resonance image showing intracapsular rupture in a third-generation implant in the right breast
33.4 Treatment
Explantation is the gold standard treatment used for silicone implant rupture, with the removal of as much silicone as possible, but it is not the only possibility. Hölmich et al. [9] studied 64 patients with at least one rupture on MRI. There was progress of silicone in 11 % of them as a conversion from intracapsular into extracapsular ruptures. There was no increase in the levels of autoantibodies during the study. Because of the small risk of spread of silicone, women with implant rupture could be followed clinically, if not (preferentially) operated on. Residual silicone inside the breast of a breast cancer patient is a risk because a mass in the breast could add difficulties in differential diagnosis with recurrence. Some authors suggest a relationship between implant rupture and fibromyalgia, but this remains an unsolved question. There is no evidence that silicone breast implant rupture can cause long-term serious diseases, such as breast cancer or connective tissue diseases [4, 11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








