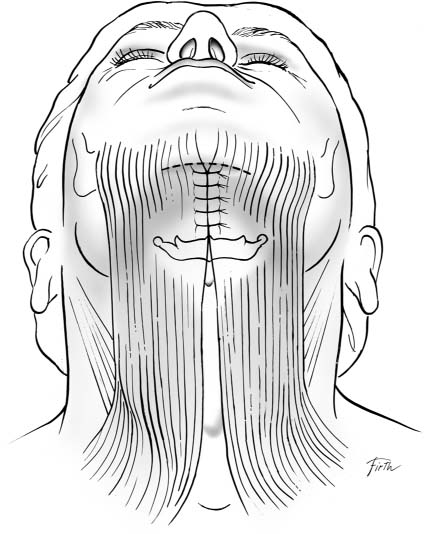
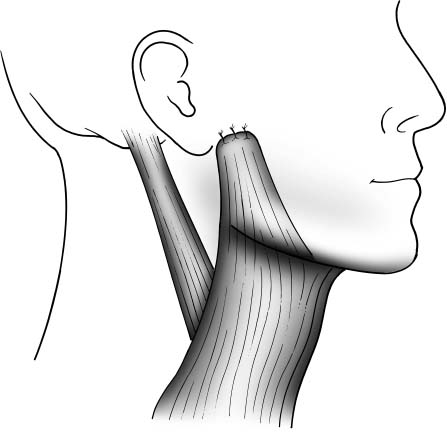
6 Rejuvenation of the aging neck is approached with varying techniques designed to correct undesired contours of the neck and cervicomental angle (CMA). Common problems in the aging neck include fullness or heaviness of contour, tissue laxity involving skin and subcutaneous soft tissue, and platysmal banding. These features may occur individually or in various combinations with one another, requiring accurate diagnosis of the underlying cause of the changes seen in the aging neck to determine an appropriate plan for treating them. Treatment of the aging neck may be done as a stand-alone procedure or in conjunction with facial rhytidoplasty, further increasing the number of variables to be considered in designing the proper procedure for an individual patient. Deformities of the neck are often effectively treated with modification of the platysma muscle and associated fibro-muscular tissue via plication and imbrication techniques. Many specific methods for this are described in the literature, and most may be useful for correcting some of the major types of deformity of the neck encountered by the facial plastic surgeon. Undermining of the skin of the neck and redraping it in a more favorable position are in many cases also necessary to completely correct an undesirable appearance of the neck. This chapter addresses the major techniques of muscle plication and imbrication described in the literature for treatment of the aging neck, and discusses the advantages of each, as well as the clinical situations for which they are best suited. Interest in treating the platysma muscle as an integral part of rejuvenation of the neck dates to the 1920s, when Bourguet1 advocated the surgical division of prominent platysmal muscle edges through a submental incision. In the 1930s Bourguet also pointed out that tightening of the skin of the neck provides only temporary improvement of paramedian platysmal bands.2 Fomon et al, in 1961, clearly expressed the opinion that techniques involving skin tightening alone for rejuvenation of the face and neck are inadequate for long-term correction, and instead proposed the creation of platysmal flaps for the correction of wrinkles in the neck.3 Despite these earlier recommendations, it was not until the work of Skoog, in the early 1970s, that interest took hold in directly advancing the platysma muscle and the contiguous fibromuscular tissue of the lower face, later to be called the superficial musculoaponeurotic system (SMAS), as a routine part of contour correction in the aging face and neck.4 Subsequently, a wide variety of techniques were described for managing the platysma muscle in the aging neck, most involving some component of undermining of skin and plication or imbrication of the platysma, and in many cases involving various strategies for division of the platysma with repositioning of the muscle.5–20 These techniques fall broadly into the four categories of wide skin undermining with minimal modification of the platysma and skin advancement, medial fixation of the platysma without division of the muscle, lateral fixation of the platysma without division of the muscle, and several combinations of techniques involving division of the platysma with its repositioning and fixation. Each of these general methodologies has enjoyed advocacy over time, and all offer advantages for certain types of aging-related problems of the neck. All techniques for imbrication and plication of the platysma require access to the subcutaneous tissues for subsequent modification and repositioning. A variety of incisions are described, with variable degrees of undermining of skin depending on the extent of access required. With regard to treatment of the neck alone, incisions in the submental crease and lower periauricular region are sufficient to access the platysma and submandibular glands, and are well camouflaged. In many cases, rhytidectomy is performed simultaneously, usually requiring more extensive periauricular incisions that incorporate the segment needed strictly for rejuvenation of the neck. In earlier works, large incisions in the lower neck, often with W-plasty or Zplasty closure, are discussed and advocated.5–7 Bourguet in 1936 advocated multiple small incisions directly overlying platysmal bands, with subsequent division of the bands and closure of the incisions.2 A similar concept was advocated by Saylan in 2002.8 Most surgeons do not currently use these techniques because of the undesirability of the visible scars they create on the neck. Effective contouring of the neck, widely accepted after the work of Skoog, is accomplished by modifying the underlying supportive tissue, primarily the platysma muscle.4 Skin incisions and flap elevation are designed primarily to allow adequate access for recontouring of the supportive subcutaneous tissue. Skin is then trimmed and redraped to conform to the improved contours. This is virtually always possible through well-camouflaged periauricular and submental incisions. The extent of undermining of skin required for treating the aging neck is most often determined by the amount of access needed to perform the desired modifications of the platysma, subcutaneous and submental fat, and submandibular glands. In some cases additional undermining is necessary to prevent puckering or irregularity of the skin after the modification of underlying structures. Short-flap procedures, with skin elevation limited to a distance of 4 or 5 cm distal to the periauricular incision, allow adequate access to the lateral border of the platysma for effective repositioning, and can be combined with limited elevation of submental skin to access medial platysmal bands. Long-flap procedures, extending the skin elevation broadly from the periauricular area to the anterior neck between the sternocleidomastoid (SCM) muscles on either side, allow much greater access for the modification of underlying structures, and in the author’s experience often make it easier to redrape skin without puckering. The broad-based blood supply to the subdermal plexus of the neck allows the surgeon to safely perform wide undermining in most patients. Care should be taken, however, due to the increased risk of skin flap compromise, in active smokers and in patients with known significant peripheral vascular disease. Regardless of the undermining technique selected, simple repositioning of the skin of the neck, with closure under tension, fails to yield satisfactory or lasting results. This problem was noted in the 1930s by Bourguet2 and addressed again by Fomon3 et al in the 1960s, and ultimately, after Skoog’s4 work in the 1970s, techniques addressing the skin alone were widely abandoned. The recent resurgence of interest in minimally invasive techniques has unfortunately led to renewed advocacy of techniques involving only the undermining and advancement of skin, which have the same problems as noted over the past half century of yielding an unnatural, stretched appearance and of poor duration of improvement in the contour of the neck, and are not to be recommended. Once incisional access is obtained and the necessary undermining of skin has been accomplished, correction of the underlying soft-tissue deformities of the neck may commence. An array of methods for repositioning and fixating the platysma muscle and associated soft tissue are described in the literature, including plication (the folding of tissue upon itself, with fixation), imbrication (the mobilization of tissue edges and approximation of the overlapped edges, with fixation), and the formal creation of muscle flaps with their subsequent repositioning. Each of these techniques offers the surgeon differing options for treating specific defects, and varies in ease of performance, safety, and expected recovery time. Perhaps the simplest technique used to treat laxity in the neck caused by descent of the medial platysma muscle is midline plication or imbrication of the separated edges of the muscle. Described as early as the 1960s by Adamson et al.,5 the technique requires first elevating an adequate sub-mental skin flap. Although Adamson and colleagues’ procedure involves a large transverse incision in the neck, subsequent authors have described such midline reconstruction of the platysma through a much smaller incision in the submental crease.9,10 The submental skin flap is widely elevated to access the entirety of the medial platysma, and the elevation is continued inferiorly to the level of the thyroid cartilage. Submental fatty fullness may be corrected by suction lipoplasty before the skin flap is elevated or by direct lipectomy after elevation of the flap. Often a mass of fibrofatty tissue is present between the medial edges of the platysma, and this is excised. The platysma is cleansed of any other adherent fatty tissue. If there are prominent medial bands they are excised sharply under direct visualization, and meticulous hemostasis is obtained. Plication of the medial edges of the platysma muscles is then accomplished with interrupted permanent sutures with inverted knots. The lowest suture is placed variably between the level of the thyroid cartilage and the level of the hyoid bone, with sufficient tension to create the desired submental contour. As the sutures are placed, any additional excess of platysma muscle may be excised with facelift scissors to insure a smooth midline contour of the platysma after closure. Once the muscle contouring is complete and meticulous hemostasis is obtained, the skin is redraped and the incision is closed. Although attractive in its simplicity, midline submental platysmaplasty is limited in effectiveness to use for relatively subtle defects of the anterior neck. There is no mechanism in this procedure for support of the lateral border of the platysma, although this can be accomplished in conjunction with the midline platysmaplasty via a periauricular incision with the elevation of lateral skin on the neck. Redundant skin may also be difficult to manage with a purely midline correction, and most methods described for the medial excision of substantial excess skin involve unsightly incisions in the anterior neck (Fig. 6.1).5–7 Fig. 6.1 Submental midline platysmaplasty. When correction of the contour of the neck primarily requires tightening of the platysma and overlying skin without the need to address platysmal banding, suture suspension of the lateral platysma may be appropriate. This general technique encompasses a group of methods that fix the lateral border to the platysma in a more superior and posterior position to effect tightening of the muscle across the CMA. There is no direct fixation of the medial edges of the platysma to one another or to other structures, and this technique, when used alone, therefore relies on existing attachments and decussation of the medial platysma to support the midline portion of the submental neck. The approach in lateral suspension of the platysma is via a periauricular incision. When a necklift is all that is necessary, a relatively short incision may be used, beginning just in front of the auricular lobule and coursing around the bottom of the ear and into the postauricular crease for a distance of several centimeters. This allows elevation of a sufficient skin flap to access the lateral edge of the platysma for repositioning and fixation. In patients in whom a facelift is performed in conjunction with correction of the contour of the neck, the greater length of the incision for the periauricular facelift makes it easier to mobilize the platysma. Once access to the platysma is obtained, several options are available for repositioning of the platysma, depending on the desired vector of correction. Many authors describe the use of plication techniques11 in this area, whereas others advocate development of a subplatysmal flap with subsequent repositioning and fixation of the muscle.4 The general concept of lateral elevation and fixation of the platysma has remained popular over several decades despite debate about the relative merits of plication, excision of muscle, undermining, and flap development. Baker,12 in 1973, described tightening the platysma by tacking its free lateral edge directly to the fascia of the SCM muscle. This was done in conjunction with his preferred facelift technique using suture plication of the SMAS, and required minimal undermining of the platysma. Skoog,4 during the same period as Baker’s description, described a more extensive platysmal undermining with fixation of the muscle to the perimastoid fascia, and there subsequently emerged many advocates of anchoring the platysmal edge, with or without undermining of the muscle, to the perimastoid fascia, SCM muscle, or both. Recently, renewed interest in minimal-incision techniques has sparked surgeons’ interest in lateral suspension of the platysma as a stand-alone procedure for correcting deformities of the aging neck. Labbe and associates13 proposed a cervical lift involving fixation of the border of the platysma to the preauricular fascia, arguing that the more vertical vector of pull that results from this provides better correction of both the CMA and the mandibular border than do more posterior fixation points such as the perimastoid fascia. In their technique, a multibite pursestring suture is anchored in the lateral border of the platysma, which is then elevated by direct traction and plicated to the preauricular fascia just anterior to the incisura (Fig. 6.2). Fig. 6.2 Lateral suspension suture (after Labbe).
Imbrication, Plication, and Wide Undermining Techniques
Submental Midline Platysmaplasty
Suspension Suture of the Lateral Platysma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








