Fig. 8.1
A tourniquet may be used on the finger for bloodless digit and nail procedures
Solution 5
Biopsies and procedures on the lip can be made blood-free when lip is secured with a chalazion clamp (Fig. 8.2).

Fig. 8.2
Use a chalazion clamp for procedures on the lip to create a bloodless field
Fig. 8.3
Stabilize the ala by inserting cotton tip applicators inside the nasal vestibule to buttress the surgical site and reduce brisk bleeding by compressing vessels. Dental roll gauze can also be used but may obstruct airflow
Solution 7
For procedures on the ear or eyelid, tumescence of the area with anesthesia will aid in hemostasis by compressing smaller vessels.
Solution 8
Be mindful of the path of larger caliber vessels so as to avoid their transection. Vessels susceptible to injury during skin surgery include the superficial temporal artery, labial arteries, angular artery, and dorsal nasal artery.
Solution 9
Be aware of the depth of vessels, and use this to your advantage when undermining. For example, the plane on the scalp beneath the galea is avascular and is the preferred level of undermining when operating in this region (Fig. 8.4).

Fig. 8.4
Blunt undermining with scissors in the avascular subgaleal plane on the scalp
Accidents Happen When
Vigorous blood flow obscures the surgical field. Non-deliberate, jerky motions to stop bleeding can result in a stick.
Solution 1
Have gauze ready. Immediately blot the area with continuous pressure. Upon release, assess the rate and volume of blood flow.
Solution 2
For less brisk bleeding, apply pressure with gauze for 5 seconds, then quickly release and work. Re-blot as needed.
Solution 3
Put the corner of a gauze at the wound edge to absorb blood by capillary action. This method accepts a short-term free-flow of blood.
Accidents Happen When
The chosen method of hemostasis is incongruent to the amount of bleeding. For example, using a topical hemostatic agent in a field that is bleeding briskly will not be successful.
Solution
Light bleeding can be stopped with topical hemostatic agents. Moderate bleeding, characterized by rapid pooling of blood in the field, should be addressed with electrosurgery. Actively spurting vessels require suture ligation. Grip the bleeding vessel with hemostats or forceps to stop it from bleeding, then throw a figure-of-eight suture.
Accidents Happen When
Electrosurgery is used excessively, causing adverse cosmetic outcomes due to excess tissue destruction.
Solution
Only use electrosurgery when it is necessary to control bleeding. Distinguish between use of electrosurgery for adjunctive surgical destruction (i.e., at the base of an excised cancer) versus merely for hemostasis.
Accidents Happen When
Caustic hemostatic agents such as aluminum chloride are used near the eye. These agents can be corrosive and damage the eye.
Solution
Periocular hemostasis should be performed with manual pressure or electrosurgery. If aluminum chloride must be used, the cotton tip should be wet but not dripping. This is often achieved by blotting the freshly wet applicator tip on the dry paper of the Mayo stand cover.
Accidents Happen When
The containers of topical hemostatic liquids are left on the surgical tray or counter uncapped (Fig. 8.5). Blood can splash into the stock bottle. There is also temptation to double-dip a contaminated cotton tipped applicator.
Fig. 8.5
Uncapped aluminum chloride stock bottle on unstable Mayo stand is at risk for contamination and spilling
Solution 1
Always recap stock bottles immediately after use.
Solution 2
Do not place a stock bottle on the surgical tray.

Fig. 8.6
Assistant hands the surgeon a wet cotton tip applicator
Accidents Happen When
A cotton tip applicator, soaked with hemostatic agent, is applied to unsplayed skin. Slack wounds shelter capillaries in the dermal papillae resulting in persistent bleeding.
Solution
Splay the skin to maximize contact of the agent with the dermal capillaries.
Accidents Happen When
A suboptimal electrosurgical device is used to gain hemostasis.
Solution
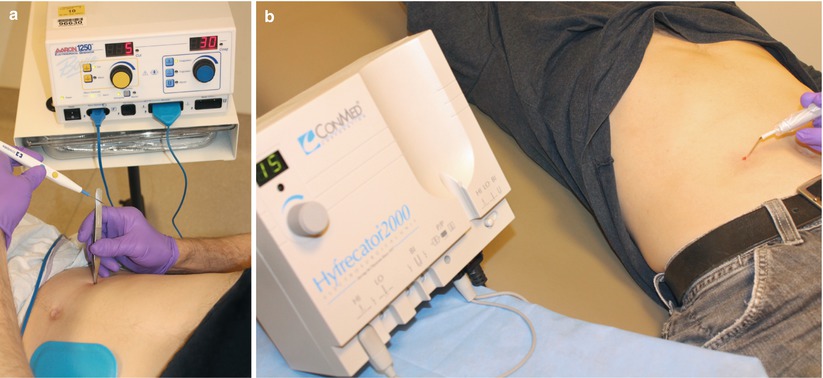
Fig. 8.7
Common electrosurgical devices. (a) Bovie (a biterminal device) used with indirect electrocoagulation via forceps. (b) Hyfrecator directly applied to skin. A dispersive plate placed on this patient (as in a) would also allow for indirect electrosurgery with forceps
Accidents Happen When
Failing to identify patients with implantable electronic devices (IED). Electrosurgical devices cause inappropriate functioning of IEDs (e.g., pacemakers, defibrillators) due to: (1) Use of high amperage; (2) Use of an electrosurgical device too close to the IED; or (3) Use of a device for long bursts (e.g., more than 5 seconds).
Solution 1
Preoperatively identify IEDs via standardized patient intake forms.
Solution 2
Heat electrocautery is the only true method to avoid electromagnetic interference (EI) with IEDs (Fig. 8.8). This modality does not use an electric current and poses no risk of EI.
Fig. 8.8
Activated heat electrocautery device (single-use)
Solution 3
If heat electrocautery is not available and a topical hemostatic agent would not create effective hemostasis then an electrosurgical device with a bipolar electrode tip should be used (Fig. 8.9).
Fig. 8.9
Bipolar electrode forceps. The current concentrates across the electrode tips and minimizes the risk of EI. A dispersive plate is required for use
Solution 4
Many outpatient offices have monoterminal, monopolar electrosurgical units (e.g., Hyfrecator) (Fig. 8.10). Limit Hyfrecator current flows to short bursts of 5 seconds or less, and place the settings on the lowest power possible to attain hemostasis. Finally, the surgical site should not be within 15 cm of the IED.
Fig. 8.10
Hyfrecator









