15
Hand Infections and Injection Injuries
 Hand Infections
Hand Infections
Hand infections are classified as superficial, deep, acute, subacute, or chronic. Ascertaining the cause of the infection, anatomical location, and length of duration of symptoms is essential to the proper diagnosis and the treatment of hand infections.
Hand infections range from superficial cellulitis to osteomyelitis. Cellulitis is a superficial inflammation of the dermal/epidermal components of the skin secondary to bacterial contamination. Deep to the dermis, infection in the subcutaneous tissue manifests as an abscess. Continual deep infectious penetration will affect the fascia or the synovial sheaths of the flexor and extensor tendons, particularly in the hand and forearm. These deeper infections warrant rapid evaluation and treatment to prevent necrotizing inflammation within the deep tissue planes and erosive extension into the hand and forearm.
Physical Examination
Patients with hand infections should receive a complete evaluation that begins with a physical examination. Key components include
• Inspection and palpation to determine location and to assess the depth of the infection
 Remove all jewelry (watches, rings, etc.) to prevent secondary vascular constriction from a tourniquet effect when edema develops
Remove all jewelry (watches, rings, etc.) to prevent secondary vascular constriction from a tourniquet effect when edema develops
• Assessment of neurovascular status
• Passive ROM assessment of all joints
• Obtain radiographs of the involved hand/digit – three views
Management
The antimicrobial treatments for common hand infections are described in Table 15–1. The antimicrobial therapies delineated in Table 15–1 represent empiric recommendations until definitive culture results are available for specific therapy.
Types of Hand Infections
Acute Paronychia
Acute paronychia is an infection that involves the eponychial, paronychial fold, or the nail matrix. This process usually begins under the skin of the lateral nail fold causing erythema and edema (paronychia). Persistent disease may cause extension into the eponychium (eponychia) or under the nail sulcus to the contralateral fold (runaround infection or horseshoe infection).
Etiology
• Poor fingernail hygiene
• Minor trauma
• Nail biting
• Finger sucking
• Manicures
• Artificial nails
• Hangnails
Treatment
An early infection without evidence of fluctuance can be treated conservatively:
• Warm soaks three times a day with a 1:1 solution of 3% hydrogen peroxide and normal saline
• Oral antibiotics for one week; consider anaerobic coverage (clindamycin 450 mg PO q.i.d.) for associated nail biting or finger-sucking etiologies (human bite)
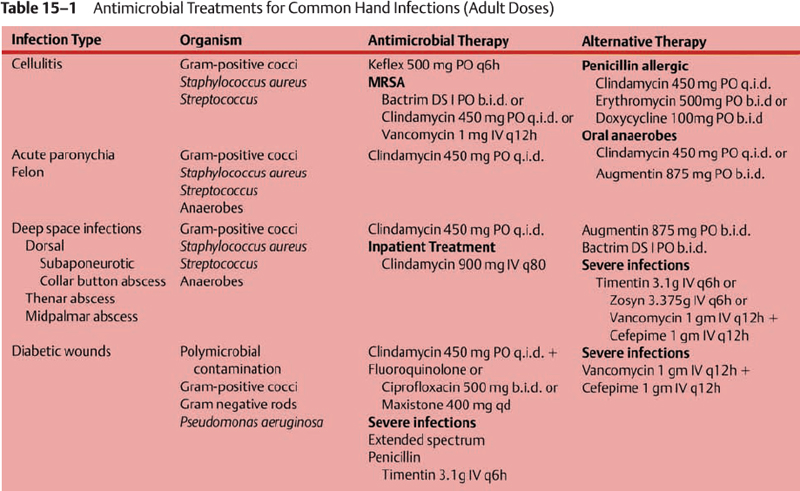
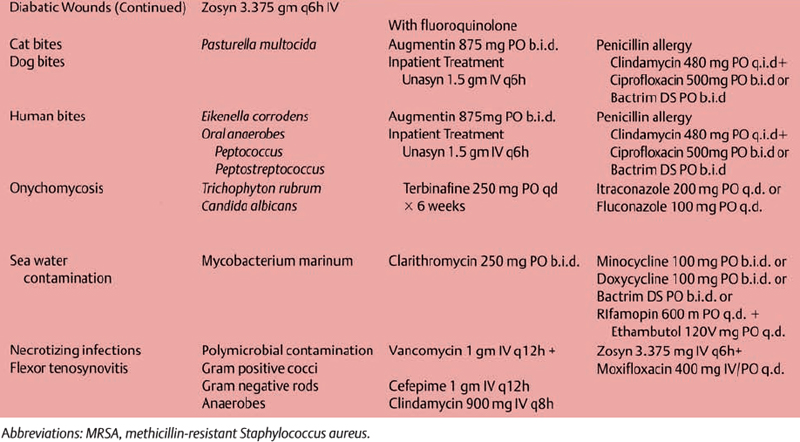
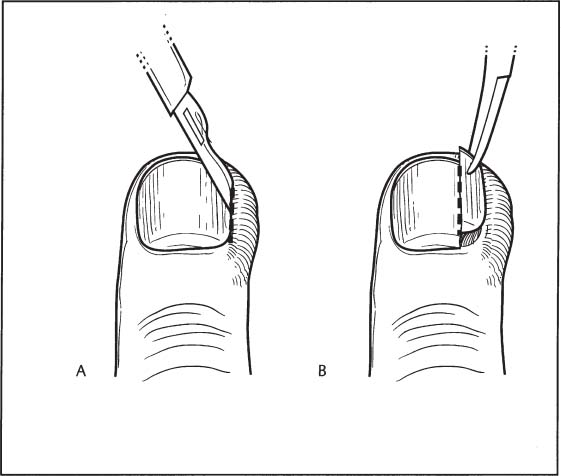
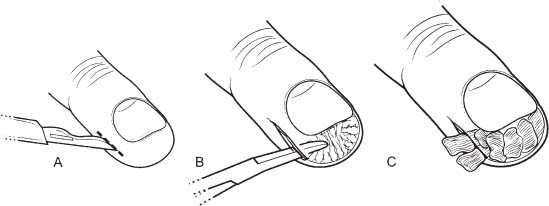
Figure 15–1 (A) Incision and drainage of paronychial infection. (B) Partial nail excision.
• Elevation
• Short-term follow-up
A paronychia that has developed purulence requires drainage:
• Perform a digital block (see Chapter 13, Fig. 13–1)
• Use the no-nail excision technique (Fig. 15–1A)
 Elevate the nail fold using small elevator from the perionychial/eponychial junction to the proximal nail edge.
Elevate the nail fold using small elevator from the perionychial/eponychial junction to the proximal nail edge.
 Excise the distal third of the nail to evacuate purulent material and if needed for additional exposure
Excise the distal third of the nail to evacuate purulent material and if needed for additional exposure
• Incision technique (Fig. 15–1B)
 Begin with a longitudinal incision along the lateral nail fold with a 15-blade beveled away from the nail
Begin with a longitudinal incision along the lateral nail fold with a 15-blade beveled away from the nail
 Repeat bilaterally if both sides are involved
Repeat bilaterally if both sides are involved
 Drain purulent material at the base of the nail by elevating the eponychial fold
Drain purulent material at the base of the nail by elevating the eponychial fold
 Excise a longitudinal strip of the nail adjacent to the fold with an edge of the eponychium for drainage
Excise a longitudinal strip of the nail adjacent to the fold with an edge of the eponychium for drainage
 Extensive eponychial and subungual infections require removal of the nail plate and stenting of the fold with Iodoform garze.
Extensive eponychial and subungual infections require removal of the nail plate and stenting of the fold with Iodoform garze.
Postoperative Care
• Warm soaks three times a day with a 1:1 solution of 3% hydrogen peroxide and normal saline
• Oral antibiotics for one week
• Elevation
• Short-term followup
• Avoid nail biting and trimming nails too closely
Chronic Paronychia
Chronic paronychia is defined as an infection that involves the eponychial, paronychial fold, or the nail matrix lasting longer than 6 weeks. Fungi are most commonly associated with these infections. Candida albicans is the primary infectious organism. However, atypical mycobacteria are implicated in hand infections of persons chronically exposed to water. Generally, these infections are found in swimmers, dishwashers, and housekeepers who have prolonged exposure to moist environments and repeated exposure to chemical irritants.
Treatment
• Topical miconazole b.i.d. or Terbinafin
• Oral ketoconazole 200 mg PO q.d. or fluconazole 100 mg PO q.d. for 4 weeks
• Consider biopsy to rule out squamous cell carcinoma for recalcitrant disease
• Marsupialization
 Perform a digital block
Perform a digital block
 Apply finger tourniquet
Apply finger tourniquet
 Using a 15-blade scalpel incise along the proximal and distal edge of the eponychium in a crescent fashion
Using a 15-blade scalpel incise along the proximal and distal edge of the eponychium in a crescent fashion
 Excise the eponychial skin and infected tissue leaving the germinal matrix intact
Excise the eponychial skin and infected tissue leaving the germinal matrix intact
 Irrigate the exteriorized germinal matrix, then pack the region with iodoform gauze
Irrigate the exteriorized germinal matrix, then pack the region with iodoform gauze
 Remove the nail plate if grossly deformed
Remove the nail plate if grossly deformed
• Change the dressing every day until complete epithelialization has occurred
Felon
The volar pad of the distal phalanx is divided into 15 to 20 fibrous fascial compartments by vertical fibrous septa extending from the dermis to the distal phalanx. Infections in this area are compartmentalized, causing the formation of small abscesses. S. aureus, Streptococci, and anaerobes cause most felons. Evaluation should rule out the presence a foreign body, which occasionally can be detected radiographically. Persistent disease will result in extension to the distal phalanx and possibly the tendon sheath of the flexor digitorum superficialis (FDS), causing osteomyelitis or flexor tenosynovitis, respectively.
Treatment
The volar pad septae must be completely obtiterated, while minimizing damage to the neurovascular bundle:
• Perform a digital block
• Apply a finger tourniquet
• Mark the nondominant side of the finger for the incision. This is usually the ulnar side of the index, long finger, or ring finger. For the thumb and little finger, release via an incision on the radial side of the digit.
• Incisions
• Obtain culture
• Spread through septa-disrupting compartment
 High lateral incision (
High lateral incision ( Fish mouth incision
Fish mouth incision Palmar longitudinal incision
Palmar longitudinal incision