32. Hair Transplantation
Michelle Coriddi, Jeffrey E. Janis, Alfonso Barrera
There are many patients that can benefit from hair transplantation, not only men (male pattern baldness) but also females with androgenic alopecia and iatrogenic alopecia, i.e., postrhytidectomy hair loss.
Additionally, there are many examples of reconstructive situations that may benefit from hair transplantation, including eyebrows, eyelashes, moustache and beard, after burns, and after accidents or tumor removal.
With the latest technology in hair transplantation we have today, we cannot make new hair, but rather we can only redistribute the patient’s own hair roots. Suitable candidates have a favorable ratio of supply and density of the donor area as it compares to the size of the area that needs to be transplanted (the “supply and demand” factor).
DEFINITION OF PROBLEM
■ Alopecia: Hair loss resulting from a diminution of visible hair1,2
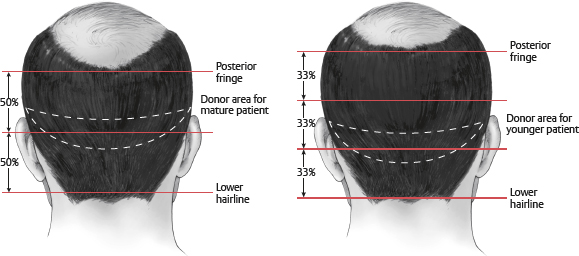
■ Three phases of hair growth: Anagen, catagen, and telogen (Fig. 32-1)
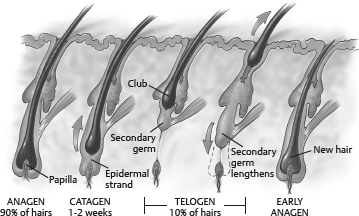
Fig. 32-1 Three phases of hair growth.
• Anagen: Active growth
• Catagen: Degradation phase
• Telogen: Resting phase
■ Thinning and baldness develop when anagen phase shortens and telogen phase is prolonged.2
GOALS OF TREATMENT2
PROVIDE A NATURAL LOOK
■ Hair growing in a natural and consistent direction with a natural appearance
• In adult males a natural and mature hairline, with some degree of frontotemporal recession, and the absence of this recession on the female patient
■ Absence of detectable scarring
INDICATIONS1,2
■ Androgenic alopecia in males and females
■ Secondary scarring alopecia (postsurgical, burns, radiotherapy-induced, traumatic injuries, postfungal infection scarring)
■ Congenital hair loss
CONTRAINDICATIONS
■ Chronic lupus erythematosus, lichen planopilaris, frontal fibrosing alopecia, classic pseudopelade of Brocq, folliculitis decalvans, central centrifugal cicatricial alopecia
PREOPERATIVE EVALUATION
NORWOOD CLASSIFICATION SYSTEM FOR MALE PATTERN BALDNESS3,4 (Fig. 32-2)
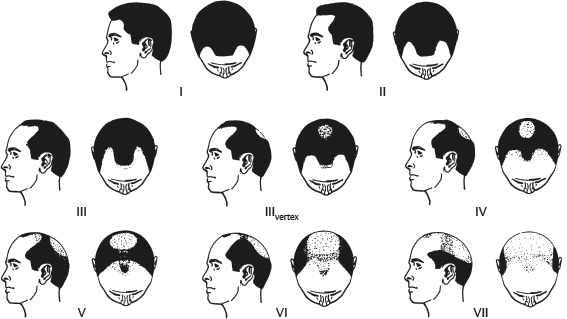
Fig. 32-2 Norwood classification of male alopecia.
■ Type I: Minimal or no hairline recession at the frontotemporal areas
■ Type II: Symmetrical triangular frontotemporal recessions extend posteriorly no more than 2 cm anterior to the coronal plane drawn between the external auditory canals
■ Type III: Symmetrical triangular frontotemporal recessions extend posteriorly more than 2 cm
■ Type III vertex: Primarily vertex hair loss; may be accompanied by frontotemporal recession that conforms to type III guidelines
■ Type IV: Sparse or absent vertex hair with more severe frontotemporal recession; areas separated by a band of moderately dense hair that extends across the top of the head
■ Type V: Same as type IV, but more severe hair loss; band of hair narrower and more sparse
■ Type VI: Absent band, and two areas interconnect
■ Type VII: Most severe form; only a narrow horseshoe-shaped band of fine, sparse hair
■ Type a variants: Applies to 3% of cases in which baldness starts at the anterior hairline without a peninsula of hair and advances in a posterior direction
LUDWIG CLASSIFICATION SYSTEM FOR FEMALE PATTERN BALDNESS5 (Fig. 32-3)
Fig. 32-3 Ludwig classification of female alopecia.
■ Grade I: Mild hair loss
■ Grade II: Moderate hair loss
■ Grade III: Severe hair loss
OTHER CONSIDERATIONS
• Normal hair density: 140-220 hairs/cm2
• Need only 70-110 hairs/cm2 for normal-appearing density
SENIOR AUTHOR TIP: This can usually be accomplished in two sessions (sometimes three, depending on the thickness and type of hair).
• When we do 2500 grafts, each graft having one, two, three, or four hairs per graft, this equates to somewhere about 5000-6000 hairs in a single session, so double that in two sessions or about 10,000-12,000 hairs in two sessions (see Fig. 32-5).1,2
■ Donor site dominance
• Concept that hair will retain growth characteristics of donor site
• Best donor sites are occipital and temporal
■ Straight versus curly hair1
• Natural results are easier to obtain using curly hair in a single session.
■ Hair color1
• Dark hair on light skin tone may require more sessions to mask the contrast and create the optimal appearance of hair fullness.
■ Age1
• For patients <23 years of age, a trial of medical treatment (e.g., minoxidil [Rogaine] or finasteride [Propecia]) is recommended because of incipient baldness.
PREOPERATIVE CARE1,2
■ Patients need to stop medications that may cause excessive bleeding (NSAIDs, acetyl salicylic acid).
■ Patients are assessed for allergies.
INFORMED CONSENT1
■ Patients must have realistic expectations and understand that the procedure redistributes existing hair; therefore hair density is limited.
■ Currently no method to create new hair exists.
■ The final result will not be seen until 1 year after transplantation.
■ Several sessions may be necessary.
EQUIPMENT1
■ Basic surgical equipment
■ No. 10 Bard-Parker blades
■ No. 11 feather blades
■ No. 22.5 and 15-degree Sharpoint blades
■ 3-0 polypropylene
■ Mantis microscope (10×)
■ Magnifying loupes (3.5×)
■ Background lighting for graft dissection
■ Chilled Petri dishes for graft preservation
■ Aftercare: Adaptic, Polysporin ointment, Kerlix, 3-inch Ace bandage
TECHNIQUE1
ANESTHESIA
■ Intravenous sedation with midazolam and fentanyl
■ Supraorbital, supratrochlear, occipital nerve blocks
■ Field blocking of the recipient site and the caudal margin of the donor area
■ Tumescence infiltration: To minimize bleeding, produces temporary thickness to facilitate easier implantation of the FUs, completes anesthesia.
• Solution of 120 ml normal saline solution, 20 ml 2% lidocaine, 1 ml epinephrine 1:1000, 40 mg triamcinolone (Kenalog) injected intradermally and subcutaneously, not subgaleally into of the recipient scalp 5-10 minutes before micrografting