44
Graft-Versus-Host Disease
Acute GVHD
• Most often arises 4–6 weeks after HSCT with traditional regimens.
• Typically presents as a morbilliform exanthem, often with perifollicular accentuation.
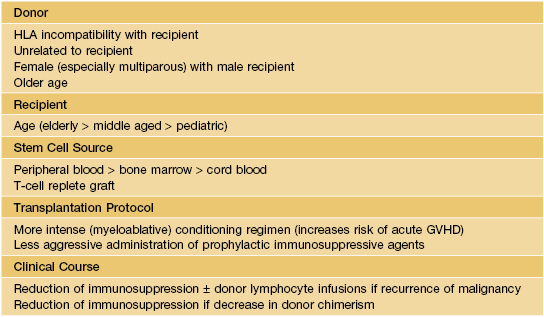
• Clinical staging is based on the proportion of the cutaneous surface involved: Stage 1, <25%; Stage 2, 25–50%; and Stage 3, >50%. Stage 4 represents erythroderma with bullae/epidermal detachment resembling toxic epidermal necrolysis (Fig. 44.1).


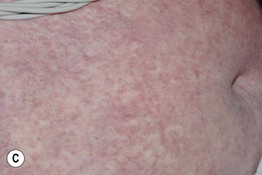

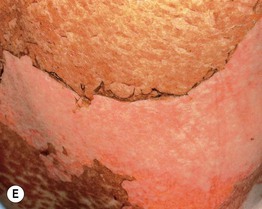
Fig. 44.1 Clinical spectrum of acute cutaneous graft-versus-host disease. A Stage 1 – discrete and coalescing small pink papules on the upper chest and neck of a woman 6 weeks following allogeneic bone marrow transplant. B, C Stage 2 – pink macules and papules of the palms that are becoming confluent 14 weeks post allogeneic bone marrow transplant and pink-violet macules and minimally elevated papules on the abdomen in a liver transplant recipient. D Stage 3 – diffuse erythema with desquamation, but without bullae formation. E Stage 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree