Introduction
The gracilis flap was described in 1972 by Orticochea, as a pedicled myocutaneous flap, and the first cases included a penile reconstruction and one of calcaneal soft tissue coverage. It was one of the first myocutaneous flaps described in humans, and in 1976, Harii published a series of gracilis free flaps for soft tissue cover and, in a separate paper, a functional free gracilis for facial reanimation. Since then the flap has become one of the most widely used of all flaps due to its versatile nature, reliable pedicle, and good donor site. It is commonly utilized for soft tissue coverage, as a functional flap, and for contour deformities such as in breast reconstruction. It may be transferred as a pedicled flap, a free flap, or a perforator flap. The flap may include all of the muscle, a longitudinal segment, or a vertical segment. It may be muscle only or combined with skin (myocutaneous) and can be innervated to act as a functioning muscle. It has become one of the essential tools of the reconstructive surgeon.
Flap Anatomy (see Fig. 49.1 and Figs 13.1 , 13.2 , 13.19 )
The muscle takes origin from the symphysis pubis and pubic arch and inserts distally into the medial surface of the proximal tibia. It is a large strap-shaped muscle and is the most superficially located of the adductors. The muscle belly is relatively broad at its origin and tapers toward the insertion. The muscle belly length is approximately 30 cm. The distal tendon of the gracilis is round in shape but becomes a flattened sheet as it inserts into the tibia. At its distal end the muscle lies between sartorius anteriorly and semitendinosus posteriorly. The function of the muscle is to adduct, flex, and medially rotate the hip and to flex the knee.
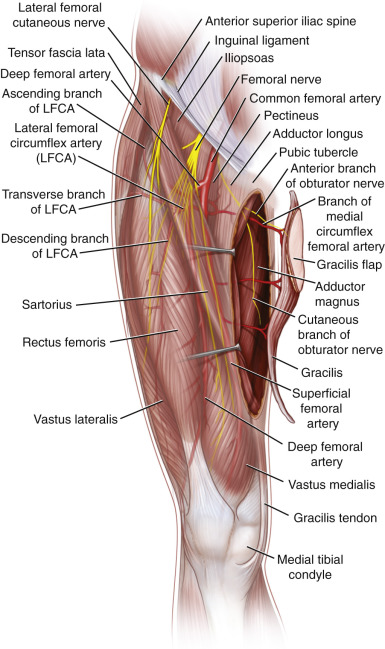
Arterial Anatomy (see Figs 49.1 , 13.1 , 13.2 )
The gracilis muscle has a type 2 vascular supply, as described by Mathes and Nahai, with one dominant and several minor vascular pedicles. The muscle is most commonly raised on the dominant pedicle only, and the entire muscle may be harvested this way. Although its pedicle is relatively consistent, some variations have been described in anatomic studies, including split and duplicate dominant pedicles.
Dominant Pedicle
Dominant:
branch of the medial femoral circumflex artery or direct branch from the profunda femoral artery
Length: 7 cm (range 6–8 cm)
Diameter: 2 mm (range 1.5–3 mm)
The main vascular supply enters the gracilis approximately 10 cm inferior to the pubic tubercle in the adult. The course of the pedicle runs deep between adductor magnus and longus and arises from either the descending branch of the medial circumflex femoral or directly from the profunda femoris artery ( Fig. 49.2 ). A large branch arises from the pedicle on the deep surface of the adductor longus and goes on to supply that muscle. Harvest of both gracilis and adductor longus on the common vascular pedicle has been described.
Minor Pedicles
Minor pedicles enter the muscle distal to the main pedicle and normally arise from the superficial femoral artery. Secondary pedicles may also arise from the descending genicular artery in less than 10% of cases. There are commonly two minor pedicles but there may be up to six. It is not common to base a flap on these minor pedicles although this technique has been described.
Perforator Vessels
Perforators are most common in the proximal third of the muscle in association with the dominant pedicle. Fasciocutaneous vessels arising from the fascia between gracilis and adductor longus may be present, but musculocutaneous perforators arising from the anterior part of the muscle are more common. Perforators from the minor pedicles may also be present but are not as reliable as those associated with the dominant vessel. Perforator diameters of 0.5–1 mm may be found arising from the proximal aspect of the muscle at the level of the major pedicle, making a gracilis perforator flap feasible.
Venous Anatomy
Primary:
venae comitantes (two) of the dominant gracilis branch
Length: 7 cm (range 5–8 cm)
Diameter: 2 mm (range 1.5–2.5 mm)
Usually two venae comitantes are found accompanying the artery. They drain into the profunda femoris vein and may converge to form a common vein a short distance before entering the profunda. The long saphenous does not make a significant contribution to drainage but may be used as a landmark as the gracilis muscle is commonly the first muscle to be found posterior to the vein.
Nerve Supply (see Fig. 49.1 and Fig 13.1 , Fig 13.2 , Fig 13.19 )
Motor:
The motor supply is from the anterior branch of the obturator nerve. This nerve arises from the obturator foramen and branches into anterior and posterior divisions beneath pectineus. The anterior division then travels between adductor longus and brevis (which it supplies) before entering the gracilis close to the location of the dominant pedicle. The nerve has a more oblique course proximally than the vascular pedicle, which lies perpendicular to the muscle and enters on its deep surface ( Figs 49.3 , 49.4 ). The nerve is at least 7–8 cm in length but up to 13 cm may be obtained by dissection back as far as the obturator foramen.
Sensory:
Sensory nerve supply to the skin of the proximal medial thigh is also from the anterior division of the obturator nerve, which runs along the deep surface of the adductor longus muscle ( Fig 13.1 , Fig 13.2 , Fig 13.19 ).
Flap Components
- •
Muscle-only flap
- •
Functional muscle flap (with motor nerve)
- •
Segmental functional muscle flap (proximal segment including motor nerve)
- •
Segmental muscle based on minor pedicle (non-functional)
- •
Myocutaneous flap (various skin paddles have been described)
- •
Perforator fasciocutaneous flap
- •
Combined gracilis and adductor longus muscle flaps (may be used as functional transfer)
Advantages
- •
Consistent anatomy of dominant pedicle.
- •
Relatively easy dissection.
- •
Large muscle belly useful for coverage of large wounds.
- •
Skin paddle may be designed over proximal muscle and can be useful for flap monitoring or for contour deficits such as in breast reconstruction.
- •
Single motor nerve consistent and located near main pedicle makes flap ideal for functional transfer. Whole muscle or small segmental transfers possible.
- •
Location makes two-team approach possible when the recipient site is in the head and neck, upper extremity, or even the contralateral lower extremity.
- •
Donor site well hidden on inner thigh.
- •
Expendable muscle with no functional loss when utilized.
Disadvantages
- •
Shape of muscle may not be as good as latissimus dorsi for coverage of large wounds.
- •
Skin paddle may not be reliable distally, due to paucity of perforators. Including the fascia between the gracilis and the adductor longus helps ensure better perfusion to the skin
Preoperative Preparation
The patient is usually positioned supine and a sandbag may be placed under the contralateral hip. The hips are abducted and knees flexed into a frog leg position. The flap is harvested without the use of a tourniquet due to the proximal extent of the dissection. Hair removal is sometimes required prior to marking, and perforating vessels may be located using Doppler or CT angiogram if a perforator flap is planned.
Flap Design and Markings
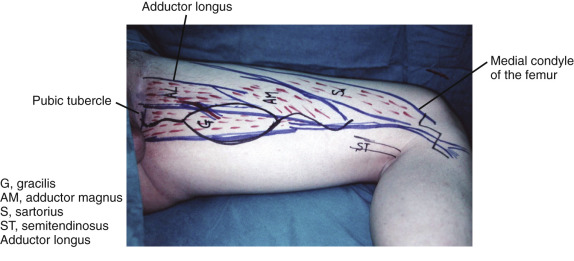
Bony landmarks of importance are the pubic tubercle and the medial condyle of the femur and/or tibia. A line can be drawn connecting these structures, and the incision line for a muscle-only flap lies parallel and 2–3 cm posterior to this line ( Fig. 49.5 ). The length of the incision for muscle-only harvest depends on the quantity of muscle required but clearly, the critical area of access overlies the dominant pedicle (around 10 cm) distal to the pubis. The entire muscle may be harvested through a relatively short proximal incision for pedicle dissection and a separate distal incision to divide the tendinous insertion. Care should be taken to avoid the groin crease in the incision, as this may become a painful scar.
If a skin paddle is required, it is designed over the proximal third of the muscle for greatest reliability. The skin paddle may be transverse, longitudinal, or fleur-de-lis in shape, and dimensions of up to 35 × 19 cm are theoretically possible.
Flap Dimensions
Muscle Dimensions
Length of muscle belly: 30 cm (range 27–34 cm) in adults. Approximately two-thirds of medial thigh length in children
Width: max 5–8 cm proximally (3–4 cm in children)
Thickness: 3 cm (range 2–4 cm). Distal tendon length 15 cm in adults
Skin Island Dimensions
Longitudinally orientated skin paddles may be up to 30 cm in length and 8–10 cm wide. It has been recommended to ensure harvest of all fascia surrounding the gracilis in order to maximize the viability of the skin paddle, which can be precarious, particularly distally. Transverse skin paddles of 25 × 10 cm may be harvested and a combination of longitudinal and transverse paddles is possible, although attention should be paid to feasibility of donor site closure when planning such large flaps ( Fig. 49.5 ).
Anesthetic Considerations
A general anesthetic is usually required for harvest of the gracilis flap, but if the recipient site is also in the lower limbs, the procedure may be performed under regional anesthesia. This may be of particular advantage if the patient is not fit for general anesthesia. Free flap reconstruction for the elderly has become increasingly accepted. The shorter procedure time associated with a two-team approach may be beneficial in this situation.
Technique of Flap Harvest
Muscle-Only Flap
With the patient supine and under general anesthetic, the lower limb is prepared and draped from the anterior superior iliac spine to below the knee. The hip is abducted and flexed and the knee flexed and a sandbag placed under the contralateral hip. With the hip abducted, the adductor longus becomes taught, and this may be easily palpated at its origin from the pubis with the gracilis origin lying just posterior. The medial femoral condyle is then palpated and a line drawn between the two. A second line, marking the incision is then drawn 2–3 cm parallel and posterior to the first line. The incision is started in the proximal third of the thigh and extended distally beyond the region of entry of the dominant pedicle (located approximately 10 cm inferior to the pubic tubercle).
The gracilis muscle is then identified as the most superficially located adductor. It lies posterior to the long saphenous vein. Care should be taken at this point to correctly identify the muscle and avoid inadvertent dissection of any of its neighbors. It may be readily distinguished from the adductor longus (lying anterior) and magnus (posterior) by flexing and extending the knee as the gracilis is the only muscle of the three to cross the knee joint. The sartorius muscle should not be confused with the gracilis proximally as it is located distant to the site of dissection.
With the muscle belly isolated, careful dissection around the muscle reveals the dominant and secondary pedicles. The dominant pedicle is easily identified as it is the largest, most proximal and is associated with the entry point of the motor nerve. Once all pedicles are identified the secondary pedicles may be ligated and divided.
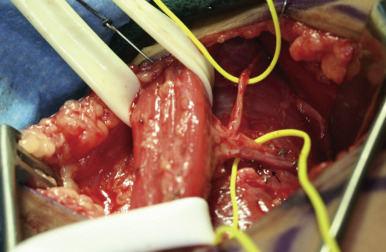
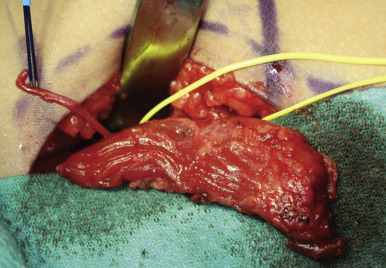
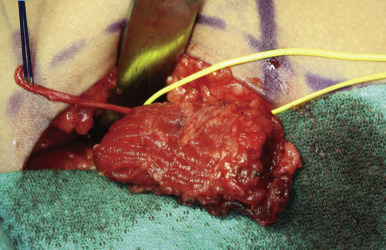
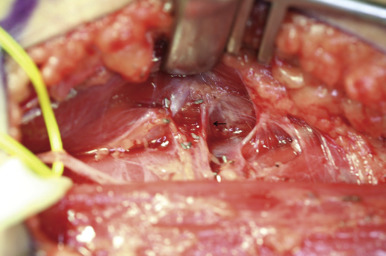
Dissection of the main pedicle commences in a distal to proximal direction. Retraction to elevate the adductor longus is required as the pedicle passes between this muscle and the adductor magnus. Branches of the main pedicle passing upward to the adductor longus should be ligated and divided ( Fig. 49.6 ). The pedicle is then dissected to its origin from the profunda femoris. At this point the artery and its accompanying venae comitans should be separated in preparation for division if the flap is to be used as a free flap.
If the flap is intended to be for functional reconstruction, the motor nerve should be identified at the time of identification of the dominant pedicle. This is then preserved and dissected proximally following its oblique course as far as is required.
Finally, the muscle itself is divided to isolate the flap on its pedicle. The proximal origin of the muscle is easily accessed through the same incision as the pedicle dissection. If the distal tendon is required for a functional transfer a separate incision can be made at the knee to isolate the tendon. The gracilis tendon lies between the insertion of sartorius anteriorly and semitendinosus posteriorly and the tendon is round in cross-section. The flattened distal portion of the insertion may be taken and can include some periosteum over the tibia if extra length is required.
Segmental Functional Gracilis Flap for Facial Reanimation
In cases of facial reanimation, the entire muscle belly of the gracilis is too large and its use results in an unacceptably bulky appearance of the cheek. In these cases we perform a segmental gracilis transfer, and flaps as small as 8 g in weight can be safely harvested in children ( Fig. 49.7 ). The dissection proceeds as described above through a limited proximal thigh incision. After identification and dissection of the neurovascular pedicle, the portion of muscle to be harvested is marked. We measure the length of muscle required at the recipient site and then add 1 cm of length on either side to allow for anchoring sutures. This required length is then marked on the gracilis, while it lies in situ in the thigh and before division of any of the muscle belly. The neurovascular pedicle is placed in the middle of the marked muscle segment. The desired portion of muscle is then dissected from the main portion of the muscle belly to include the neurovascular pedicle. The posterior third of the muscle segment is most often discarded to reduce bulk as the pedicle enters at the junction of anterior and middle thirds on the deep surface. The bulk may be reduced further by excision of an additional strip of muscle from the anterior border.

Cavadas et al. in 2004 showed that it may be possible to harvest small portions of the gracilis based on secondary pedicles only.
The Gracilis Skin Paddle Variations and the TUG Flap
The transverse upper gracilis (TUG) musculocutaneous flap was first described by Yousif et al. in 1992. The skin paddle is orientated transversely over the proximal third of the muscle and extends from the site of the femoral vessels anteriorly to the midline of the thigh posteriorly. Its proximal location is designed to include the most consistent perforators that are associated with the dominant pedicle. Skin paddles of 25 × 10 cm have been used, with the main limiting factor being donor site closure. The flap has gained popularity although is still seen as a secondary choice to lower abdominal free flaps for breast reconstruction. It is a reasonable choice in the patient for whom a DIEP/TRAM flap is not possible and who requires a small volume reconstruction ( Case 49.7 ). Criticisms of the flap for breast reconstruction include the small volume obtained, and some surgeons routinely use two flaps for a single breast reconstruction in order to overcome this problem.
Longitudinally oriented skin paddles and fleur-de-lis patterns have been described, which rely on the integrity of perforators from the secondary pedicles. The functional free gracilis for brachial plexus reconstruction as described by Doi routinely includes a longitudinally oriented skin paddle for monitoring, and the authors stress the importance of inclusion of harvesting all surrounding fascia with the muscle to maximize reliability of the skin paddle.
Gracilis Perforator Flaps
Hallock first described the gracilis perforator flap in 2003 and since then, other authors have studied the vascular anatomy of the flap allowing further extension of the skin paddle. In the original description perforators were identified by Doppler ultrasound at the start of the case and a skin paddle of 12 × 16 cm was designed around these vessels. The territory was located posterior to the site of the femoral vessels and distal to the groin crease. Peek et al. later defined the skin paddle in cadaveric studies as 18 × 15 cm but showed that by inclusion of intramuscular anastomosis between the dominant and secondary pedicles this territory may be extended, theoretically up to 27 cm distally.
There is minimal functional deficit following gracilis harvest and some authors argue that use of a perforator flap sparing the whole muscle is unnecessary.
Special Instruments
No special instruments are required for standard flap elevation, but some authors have performed endoscopic harvest of the flap in an attempt to minimize donor site morbidity.
Donor Site Closure and Management
After careful hemostasis if there was no significant amount of fascia harvested, the fascia is closed loosely to avoid muscle herniation and the skin closed in two layers with subcuticular absorbable sutures. If desired a compression bandage may then also be applied. There is no restriction in terms of postoperative mobilization. A drain may be used if required although it is often not necessary in children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






