Gold Weight Insertion for Upper Eyelid Reanimation
Larissa Habib
Brian P. Marr
DEFINITION
Upper eyelid loading with a gold weight is the treatment for paralytic lagophthalmos causing exposure keratopathy. This is due most commonly to facial nerve damage following trauma, infection, ischemic event, or tumor.
Pure gold is used for its density and to minimize allergic reaction.
The weights range from 0.8 to 1.6 g.
ANATOMY
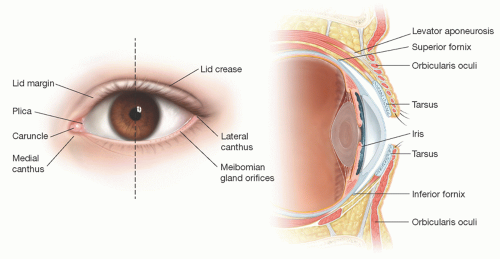
The upper and lower eyelid meet at the medial and lateral canthus with the lateral canthus sitting 2 to 4 mm higher than the medial (FIG 1).
The palpebral fissure is approximately 28 to 30 mm in length and 9 to 10 mm in height.
The eyelid anatomy can be divided into anterior and posterior lamellae.
The anterior lamella consists of the skin and the orbicularis oculi muscle.
The eyelid skin is the thinnest in the body (less than 1 mm). The epidermis receives its nourishment from a deeper connective tissue layer as it lacks blood vessels and lymphatics. There is a sparse amount of fat in the preseptal and preorbital skin and is absent in the pretarsal skin.
The orbicularis oculi is loosely adherent to the skin and divided into orbital and palpebral portions. The palpebral portion is further divided into pretarsal and preseptal and functions in blinking and voluntary winking. The orbital portion is for forced closure.
The posterior lamella consists of the tarsus and the conjunctiva.
The tarsus is composed of dense fibrous tissue. It is approximately 1 mm thick and provides the structural support of the eyelid. The upper eyelid tarsus extends from the punctum to the lateral canthus and is 30 mm long and 7 to 10 mm high, with the highest portion being centrally. The lower tarsus ranges from 3.5 to 5 mm in height. The ciliary border contains meibomian gland orifices that provide the lipid layer of the tear film. The medial and lateral ends are attached to the orbital rim by the medial and lateral palpebral ligaments.
The conjunctiva is a nonkeratinized, stratified squamous epithelium that lines the inside of the eyelids and provides coverage to the sclera.
Upper eyelid retractors
The levator palpebrae superioris arises at the orbital apex and courses anteriorly for 40 mm ending in the aponeurosis 10 mm behind the septum. At this junction, it changes direction to vertical and then inserts inferiorly onto the lower third of the tarsal plate. In addition, some fibers pass anteriorly to the eyelid crease.
Mueller muscle originates from the undersurface of the levator at the muscular aponeurotic junction and then travels between the levator and the conjunctiva to insert on the superior border of the tarsus. It is innervated by the sympathetic nervous system.
The lower eyelid retractors are fascial extensions of the inferior rectus muscle originating as the capsulopalpebral fascia. The lower lid retractors insert at the inferior border of the tarsal plate. A small portion of the lower eyelid retractors joins with Tenon capsule at the inferior fornix and courses anteriorly to form the lower lid crease.
Blood supply to the eyelids is derived from branches of both the internal and external carotid arteries.
Medially, two palpebral branches (superior and inferior marginal arteries) arise from the ophthalmic to supply the upper and lower lid. These arteries then travel horizontally as the marginal arcades, which lie on the tarsal plate (4 mm from the upper margin and 2 mm from the lower margin).
Laterally, the lacrimal artery provides branches to both the upper and lower lid, which then travel horizontally to anastomose with the marginal arcades.
The external carotid contributes through branches of the facial, superficial temporal, and infraorbital arteries.
PATIENT HISTORY AND PHYSICAL FINDINGS
Facial paralysis can occur from many causes including tumor, postsurgical, infection, trauma, idiopathic Bell palsy, and cerebral vascular accidents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree