Gluteal Thigh Flap for Perineal Reconstruction
David Gerth
Christopher J. Salgado
DEFINITION
Gluteal thigh flap is an axial fasciocutaneous flap based on the inferior gluteal artery.
Usually raised as a pedicled flap, but free flap technique has been reported
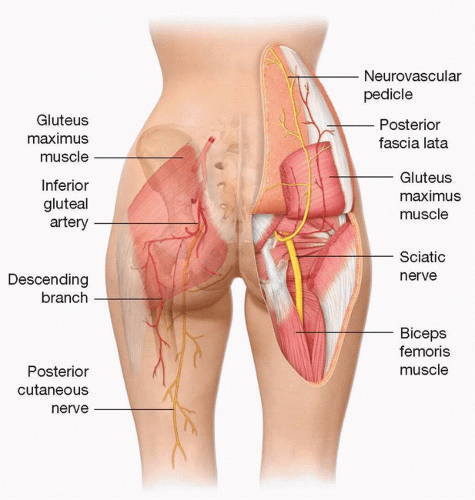
ANATOMY (FIG 1)
Blood supply: Descending branch of inferior gluteal artery1
Terminal branch of the internal iliac artery.
Course: exits the pelvis through the infrapiriform aperture
Supplies the lower aspect of the gluteus maximus muscle and overlying skin through musculocutaneous perforators2
These perforators combine with branches of the circumflex femoral arteries and obturator artery to create the cruciate anastomosis.
This anastomosis allows the posterior thigh to be adequately perfused even in the case of an absent inferior gluteal artery.
Recent study has shown that cutaneous branches supplying the distal gluteal and proximal posterior thigh can be more regularly identified.
108 of 118 specimens had cutaneous branches derived from the descending branch of the inferior gluteal artery. Ten cases derived from medial or lateral circumflex femoral artery or from the profunda femoris.3
Pedicle is usually spared during radical pelvic ablations.
Pedicle is usually outside the area affected by pelvic radiation.4
Venous drainage
Redundant
Deep system
Venae comitantes of inferior gluteal artery
Venae comitantes of deep femoral perforators
Superficial venous system
Due to substantial drainage, venous congestion rarely occurs.5
Innervation: posterior femoral cutaneous nerves (S1-S3)
Many fascicles exit the sciatic foramen along with the inferior gluteal artery.
Fascicles converge to form a common trunk with the descending branch of the inferior gluteal artery.4
PATIENT HISTORY AND PHYSICAL FINDINGS
IMAGING
No preoperative imaging is necessary.
Viability of the flap can be assessed intraoperatively via quantitative fluoroangiography (FIG 2).
SURGICAL MANAGEMENT
Goal of surgery
The process of perineal repair is especially difficult due to the necessity to preserve the anogenital triangle as well as to provide adequate skin coverage and tissue replacement.
Successful repair consists of appropriate reconstruction with vascularized tissue along with proper anogenital repair without leakage of feces or urine.
Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree