Cleft surgeons seek to provide the best results in the fewest surgeries. Gingivoperiosteoplasty (GPP) is one option to achieve this goal. Although it may normalize early form and function and obviate secondary alveolar bone grafting, it has been associated with iatrogenic dentofacial restriction requiring more extensive treatment later. GPP technique associated with nasoalveolar molding (NAM) uses passive presurgical molding with strict patient-selection criteria. Data on the benefits of NAM-GPP are favorable but long-term outcome studies are required before its final role in cleft care is determined. This article describes the history, technique, perioperative care, and preliminary outcomes of NAM-GPP.
Key points
- •
Gingivoperiosteoplasty (GPP) replaces alveolar cleft soft tissue with a gingivoperiosteal tunnel that facilitates bone healing without the need for bone grafting.
- •
Skoog’s descriptions of “boneless bone grafting” popularized the technique in cleft care.
- •
The reported negative impact of the Latham device on dentofacial growth has led to the development of nasoalveolar molding (NAM), a passive, noninvasive, molding process.
- •
NAM-GPP prerequisites include appropriate cleft anatomy to allow alveolar bony approximation.
- •
GPP seals the cleft nasally, orally, and labially by mucoperiosteal flaps.
- •
GPP advocates report the elimination of secondary alveolar bone grafting at mixed dentition as a benefit.
- •
Critics voice concerns over iatrogenic facial growth restriction and malocclusion.
- •
Data available on NAM-GPP (with appropriate patient selection and technique) are favorable but long-term outcome studies are required.
Gingivoperiosteoplasty (GPP) removes the soft tissue barrier within an alveolar cleft and replaces it with a gingivoperiosteal tunnel that facilitates bone healing through guided tissue regeneration (GTR) without the need for bone grafting and its associated donor site morbidity. The importance of the periosteum in bony healing has been well documented by several investigators ; however, Ollier is most often credited with first emphasizing the osteogenic potential of the periosteum. This is especially true for patients at a younger age. Dahlin and colleagues were first to demonstrate union of critical bony defects by creating a Teflon tunnel to guide bone regeneration while impairing soft tissue in-growth and fibrous nonunion. Although the osteogenic properties of mucoperiosteum in healing a cleft palate were initially recognized by Langenbeck in the 1800s, it was not until Tord Skoog’s descriptions of primary GPP or “boneless bone grafting” in the 1960s that the technique became popularized in cleft care. Successful GTR following a GPP depends on the integrity of the guiding tunnel to restrict fibrous in-growth, the presence of viable periosteum in the created flaps, and the age of the patient.
Historical perspective
Skoog described the creation of local mucoperiosteal flaps with oxidized regenerated cellulose. Though not every patient grew bone initially, with repeated periosteal flaps, all patients eventually formed a bony bridge. Without presurgical molding, this method required extensive, often repeated, subperiosteal maxillary dissection to close the alveolar cleft, with an associated negative impact on facial growth. In the 1970s and 1980s, Ritsilä and colleagues, and Rintala and Ranta, reported the outcomes of free tibial periosteal grafts. During a 6-year period, they treated 67 patients with Skoog’s maxillary periosteal flap technique and 23 with free periosteal grafts. Although bony formation was noted in 64% of patients treated with the Skoog technique and 85% of those treated with the tibial periosteum graft technique, secondary bone grafts were required in 72% and 73% of each group, respectively. There was a lateral cross-bite in all patients. A similar finding with the Skoog technique was reported by Renkielska and colleagues. They found 50% of patients had Goslon scores of 4 or 5 with need for orthognathic surgery and the technique fell out of favor.
The popularization of presurgical orthopedics ushered in the next phase in GPP care. Millard’s presurgical orthopedics, periosteoplasty, and lip adhesion (POPLA) approach involved presurgical orthopedics with the “Latham device” followed by lip adhesion and GPP at 3 to 4 months of age. Active mechanical presurgical approximation of the alveolar edges allowed for less subperiosteal dissection, but critics of the POPLA approach note a 40% to 42% maxillary vertical growth disturbance of the maxilla and 100% of patients with cross-bites that were often difficult to correct orthodontically.
Historical perspective
Skoog described the creation of local mucoperiosteal flaps with oxidized regenerated cellulose. Though not every patient grew bone initially, with repeated periosteal flaps, all patients eventually formed a bony bridge. Without presurgical molding, this method required extensive, often repeated, subperiosteal maxillary dissection to close the alveolar cleft, with an associated negative impact on facial growth. In the 1970s and 1980s, Ritsilä and colleagues, and Rintala and Ranta, reported the outcomes of free tibial periosteal grafts. During a 6-year period, they treated 67 patients with Skoog’s maxillary periosteal flap technique and 23 with free periosteal grafts. Although bony formation was noted in 64% of patients treated with the Skoog technique and 85% of those treated with the tibial periosteum graft technique, secondary bone grafts were required in 72% and 73% of each group, respectively. There was a lateral cross-bite in all patients. A similar finding with the Skoog technique was reported by Renkielska and colleagues. They found 50% of patients had Goslon scores of 4 or 5 with need for orthognathic surgery and the technique fell out of favor.
The popularization of presurgical orthopedics ushered in the next phase in GPP care. Millard’s presurgical orthopedics, periosteoplasty, and lip adhesion (POPLA) approach involved presurgical orthopedics with the “Latham device” followed by lip adhesion and GPP at 3 to 4 months of age. Active mechanical presurgical approximation of the alveolar edges allowed for less subperiosteal dissection, but critics of the POPLA approach note a 40% to 42% maxillary vertical growth disturbance of the maxilla and 100% of patients with cross-bites that were often difficult to correct orthodontically.
NAM-GPP
The potential negative impact of the active direct force of the Latham device on dentofacial growth led to the development of a more passive molding process, nasoalveolar molding (NAM), as described by Grayson and colleagues. NAM is described as guiding early alveolar growth as opposed to directly molding it. NAM-GPP differs from POPLA in the method of presurgical alveolar molding and surgical technique as well as in more rigorous selection criteria by which patients are deemed appropriate candidates for a GPP. This is partly because its advocates think NAM is a more accurate means of molding the leading edges of the alveolar cleft into a close parallel relationship to optimize flap design and osteogenesis.
Patient selection and evaluation
Prerequisites for a GPP are: (1) an informed consenting family, (2) appropriate cleft anatomy to allow alveolar bony approximation, (3) an optimally molded alveolar cleft and intact mucosa, and (4) no dental eruption. Once these criteria are met, the GPP can be scheduled at the time of the primary lip repair.
Before undergoing a GPP, the infant with a cleft must be evaluated by the practitioner administering the NAM, as well as the surgeon who will be performing the GPP. Before initiating NAM, the guardians of the infant should be introduced to the concept of a GPP, the risks and benefits reported in earlier GPP techniques, and the current data on NAM-GPP.
Variations in cleft anatomy may exclude some patients from NAM-GPP. For example, patients with isolated clefts of the primary palate are usually not good candidates for NAM-GPP. Due to the bony fusion of the secondary palate, the alveolar segments of the primary palate are more resistant to parallel presurgical molding and, in many cases, cannot be adequately aligned for a successful GPP. Another group of patients who are not candidates for a NAM-GPP are the “mesenchymal deficient” infants, with such wide unilateral clefts that the alveolar arch form would be excessively constricted should the segments be presurgically approximated. Finally, in bilateral complete clefts, it is not always possible to align both sides of the premaxilla with the lateral alveolar segments to allow for bilateral GPP. In these cases, the one aligned alveolar cleft can undergo a GPP to convert the arch form to a lesser and greater segment instead of a three-piece upper jaw. Although the contralateral cleft will need to be secondarily grafted, the premaxilla will be stabilized by the GPP to facilitate incisor mastication during early childhood.
Preoperative management
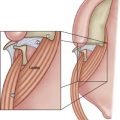
During the preoperative management (NAM) process, the preoperative assessment of alveolar ridge alignment and parallel alveolar molding is subjective. Alveolar segment alignment is assessed based on the underlying bone, not on the visible gingival mucosa ( Fig. 1 ). In some cases, the gingival tissue can be hypertrophied in the area of the cleft, mimicking close approximation, while the underlying bone gap is wide. In other cases, the alveolar cleft is compressed, but the bony arch forms are not in alignment, with the premaxilla wedged anterior to collapsed lesser segments or the lesser segment posterior to the greater ( Fig. 2 ). If a GPP is performed in these situations, the mucoperiosteal tunnel between the exposed bone edges will be “kinked,” creating a soft tissue barrier instead of GTR.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree