49. Genioplasty
Ashkan Ghavami, Bahman Guyuron
RELEVANT ANATOMY
MUSCLES (Fig. 49-1)
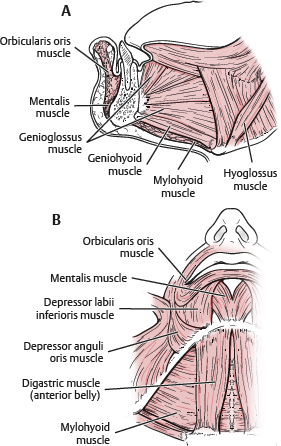
Fig. 49-1 Relevant muscular anatomy for genioplasty.
■ Mentalis
• Conelike, vertical fibers from incisive fossa to overlying skin
• Can cause wrinkling, and if hyperdynamic, may be visible under lower lip
• Midline void between fibers seen when chin dimple present
■ Orbicularis oris (lower fibers)
■ Depressor anguli oris
■ Quadratus (depressor) labii inferioris
■ Geniohyoid, genioglossus, mylohyoid, and anterior belly of digastric
• Attach to lingual (posterior) aspect of chin
BONY LANDMARKS
■ Mental foramen
■ Digastric fossa
■ Mental protuberance
■ Mental spines
■ Submandibular fossa
NERVE SUPPLY
■ Inferior alveolar nerve and mental nerve (terminating branch exiting mental foramen)
• Mental nerve: Located at base of first or second bicuspid
• Inferior alveolar nerve
► Risk of injury during genioplasty procedures
► Osteotomies should be 5-6 mm below mental foramen to prevent injury to nerve branches or tooth apices.
BLOOD SUPPLY
■ Labial branch (dominant supply) of facial artery
■ Inferior alveolar artery
SIGNIFICANT CEPHALOMETRIC POINTS (Fig. 49-2)
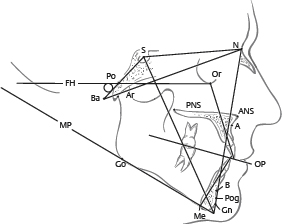
Fig. 49-2 Significant cephalometric points. (A, A-point; ANS, anterior nasal spine; Ar, articulaire; B, B-point; Ba, basion; FH, Frankfort horizontal plane; GN, gnathion; Go, gonion; Me, menton; MP, mandibular plane; N, nasion; OP, occlusal plane; Or, orbitale; PNS, posterior nasal spine; Po, porion; Pog, pogonion; PNS, posterior nasal plane; S, sella.)
■ Pogonion (Pog): Most projecting portion of mandible. Denotes chin excess or deficiency in relation to other structures (i.e., nasion and lip position)
■ Menton (Me): Lowest (most caudal) portion of chin
■ Subspinale (A): Columellar-labial junction
■ Supramentale (B): Deepest point between pogonion and incisor
■ Nasion (N): Nasofrontal junction
INDICATIONS AND CONTRAINDICATIONS
OSSEOUS GENIOPLASTY
■ Indications
• Horizontal asymmetries of any magnitude
• Excess deficiency or excess in both vertical and sagittal planes
► Moderate to severe microgenia
• Secondary cases after osseous or alloplastic genioplasty
• Adjunct to formal orthognathic surgery
► Alloplastic genioplasty is rarely, if ever, combined with formal orthognathic lower or upper jaw surgery.
■ Contraindications
• Inadequate bone stock (i.e., elderly patients, bone pathology)
• Abnormal dentition or significant dental pathology
• Patient preference to not have osteotomy
■ Contrary to common belief, can be a relatively simple and efficient procedure
■ More versatile procedure versus alloplastic augmentation
• Allows multidimensional chin correction, including reduction
ALLOPLASTIC AUGMENTATION
■ Indications
• Mild isolated sagittal deficiencies
• Need to increase only the labiomental fold depth
• Relative: Concomitant necklift/facelift
► Easily facilitates alloplastic augmentation as a concomitant procedure
■ Contraindication
• Excess horizontal deficiency
• Any vertical deficiency
• Mandibular asymmetry
• Secondary cases with bony erosion
• Malocclusion: Orthognathic surgery required
TIP: Generally, alloplastic augmentation should be used only in patients with mild to moderate chin deficiency in the sagittal plane and a shallow labiomental fold.1–4
■ Caveat: Aesthetic surgery patients seem to prefer alloplastic augmentation, and tend to shy away from osteotomies.
• Facelift/necklift procedures often include a submental incision that can easily be used for placing a chin implant.
• Popular media has shown a bias toward alloplastic augmentation and present any “cuts in the bone” as very “invasive.”
■ Malocclusion requires consideration of orthognathic surgery and a more extensive workup (cephalometric analysis, occlusion models) and possible collaboration with an oromaxillofacial surgeon.
■ Significant microgenia usually requires an osseous genioplasty, because a very large implant can appear awkward.
PREOPERATIVE EVALUATION
■ Medical comorbidities
• Diabetic and immunosuppressed patients: Not good candidates for alloplastic chin implantation
► Osteotomy site(s) may heal poorly.
• Age: Higher-age patients may have osteopenic bone—not good candidates for osseous genioplasty
■ Occlusion type (Fig. 49-3)
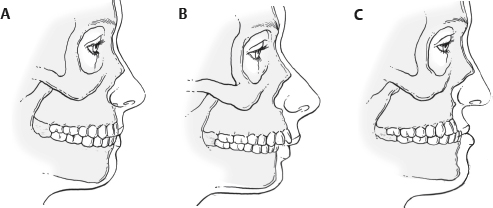
Fig. 49-3 Occlusion types. A, Angle class I. B, Angle class II. C, Angle class III.
• Normal occlusion (Angle class I)
► Mesiobuccal cusp of maxillary first molar occludes into the buccal groove of the mandibular first molar (Fig. 49-3, A).
• Angle class II malocclusion
► Mesiobuccal cusp of maxillary first molar occludes medial to the buccal groove (Fig. 49-3, B).
► Most common malocclusion in North American whites.
► Class II is often an indication for further evaluation and possibly orthognathic surgery with maxillary and mandibular osteotomies.
• Angle class III malocclusion
► Mesiobuccal cusp of the maxillary first molar occludes distal to the buccal groove of the mandibular first molar (Fig. 49-3, C).
TIP: Obtaining previous orthodontic history is important; because occlusion may have been corrected without addressing maxillary and mandibular disharmonies (deformity becomes masked).
■ Dentition
• Before 15 years of age, permanent dentition may not be fully erupted.
► Greater risk of injury during osteotomies
• Elderly patients may have retruded alveolar ridge (if edentulous), which contributes to chin pad ptosis.
► Presence of little bone stock
► May be better candidates for alloplastic augmentation
• Patients with poor dentition or infected dentition are very poor candidates for any form of genioplasty until fully treated.
LIFE-SIZE PHOTOGRAPHS2
■ Bilateral sagittal view, frontal views, and bilateral oblique (three-quarter) views
MIDFACE HEIGHT
■ Vertical maxillary excess: Especially important when accompanied by a deep labiomental fold
• Patient better served by formal orthognathic correction, with or without a genioplasty
NOSE-CHIN-LIP EVALUATION (Fig. 49-4)
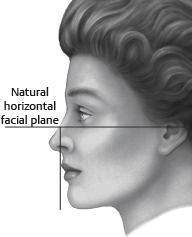
Fig. 49-4 Nose-chin-lip evaluation.
■ Nasofacial harmony is linked with chin dimensions and vice versa.
■ Chin projection should be 3 mm posterior to nose-lip-chin plane (NLCP).5
■ Nasal length: Two thirds of midfacial height and exactly equal to chin vertical length5
Symmetry of Lower Third of Face
■ Right-to-left asymmetries of the mandible and chin may require multiple osteotomy configurations to centralize chin or canting of the osteotomy line and differential plate bending.
■ Difficult to correct with alloplastic augmentation alone
SOFT TISSUE ANALYSIS
■ Soft tissue pad: Normally 9-11 mm thick
• Palpated at pogonion and off midline with patient in repose and then when smiling
• Soft tissue contribution can predict effects of augmentation.
■ Stomion: Junction between upper and lower lip in repose
■ Upper/lower lips: Lower lip eversion from deep bite, excess lip bulk, or excess overjet may deepen labiomental fold.4
■ Labiomental fold
• Indentation or crease between lower lip and lowest point of mandible (menton) best seen on sagittal view
• Fold aesthetics dependent on vertical proportion of mandible and facial length3
► Example: Deep fold may look good on longer faces.3
• Evaluate for height (when stomion-to-menton is divided into thirds, fold often falls at junction of upper and middle third).
► If fold is too low, augmentation may only address chin pad.4
• Depth
► Fold depth approximately 6 mm in men and 4 mm in women6
► If deep, horizontal vector, chin augmentation may result in an awkward exaggerated deep fold and an overprojected chin
► If shallow, may be further effaced by vertical augmentation
■ Riedel line: A line drawn vertically down facial plane on sagittal view, tangential to anterior upper and lower lip (Fig. 49-5)

Fig. 49-5 Riedel plane is a simple line that connects the most prominent portion of the upper and lower lip, which on a balanced face should touch the pogonion.
• Lower lip should be 2-3 mm posterior to upper lip projection.
• Pogonion should never project beyond this line and should be slightly posterior to it (or just touching it).
DYNAMIC AND STATIC CHIN PAD ANALYSIS4
■ A thin chin pad on smiling: Potential for increased pad effacement with increased bony prominence (i.e., native or from augmentation)
• Burr reduction or osteotomy setback may be required.
■ A thick pad may increase submental soft tissue fullness and worsen the cervicomental angle if bony setback performed
WITCH’S-CHIN DEFORMITY
■ Definition: Ptosis of soft tissue caudal to menton and an exaggerated submental crease
■ Correction requires soft tissue/muscle resection and/or repositioning.
■ Augmentation can exaggerate deformity.
TIP: Mentalis muscle fixation superiorly is critical to preventing any soft tissue descent. Secondary cases may require soft tissue fixation with a Mitek device (DePuy Synthes) to prevent ptosis recurrence.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




