Free Flaps
Radial Forearm Flap
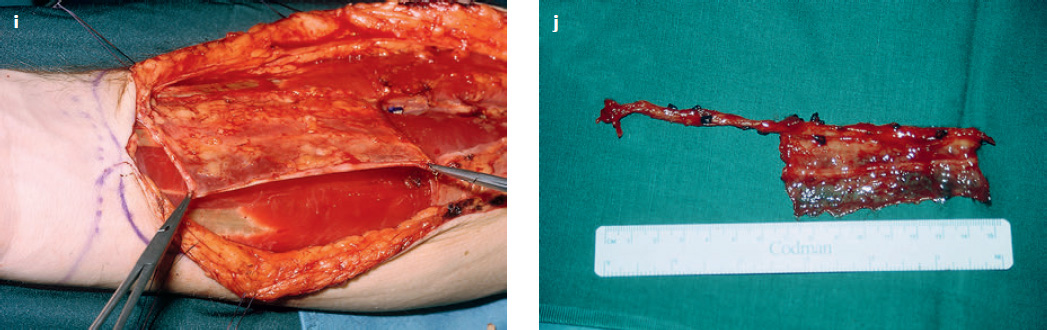
( Fig. 14.1 )
Flap type:
Fasciocutaneous (neurovascular) flap or pure fascial flap of the axial pattern type (see Figs. 1.3 and 1.4 ).
Flap components:
Skin, subcutaneous fat, and fascia (may include the sensory nerve).
Use:
Microvascular flap.
Vascular pedicle:
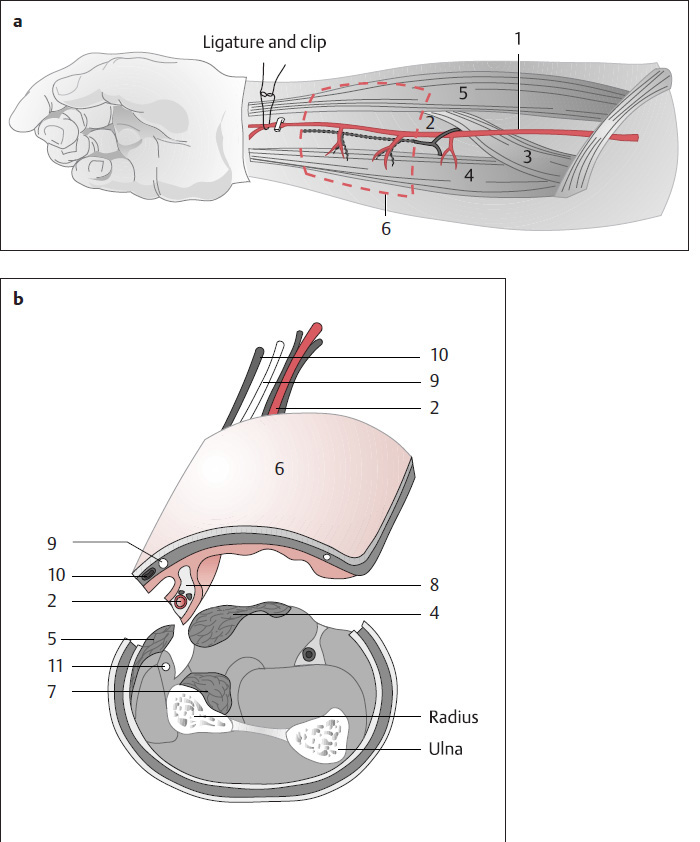
The flap is based on the radial artery, which is a continuation of the brachial artery. Its caliber is ~1 to 2 mm. The radial artery is accompanied in its distal portion by two venae comitantes ( Fig. 14.1a, b , 2), which unite at the elbow to form one vein ~2 mm in diameter. The flap is innervated by the lateral antebrachial cutaneous nerve ( Fig. 14.1b , 9), which runs parallel to the superficial cephalic vein.
Flap size:
Maximum 5 × 15 cm.
Position:
Supine.

Flap elevation:
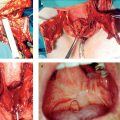
Before the operation, it is determined whether the hand will survive without radial arterial input. This is done by performing an Allen test or using Doppler ultrasound or angiography to check for adequate collateral flow via the ulnar artery. The flap size is marked on the skin ( Fig. 14.1c ), and an S-shaped incision is made from the elbow to the proximal margin of the flap, dividing the forearm fascia. Next, the muscle bellies of the flexor carpi radialis and brachioradialis are identified ( Fig. 14.1a , 4 and 5) and separated from their intermuscular septum. The radial artery and its two venae comitantes lie between these muscle bellies on the fascia of the flexor digitorum superficialis. Next, the perimeter of the flap is incised, dividing the fascia of the flexor digitorum superficialis at the ulnar border. The dissection of the flap and muscular fascia ( Fig. 14.1b , 8) proceeds from the ulnar to the radial side, avoiding injury to the peritendinous tissue. The flap should not be developed too far distally, to preserve the extensor retinaculum. Next the radial artery and its accompanying veins are ligated at the distal margin of the flap. The next step is to dissect the fasciocutaneous tissue from the radial side, as far as the abductor pollicis longus and brachioradialis muscles, preserving the superficial branch of the radial nerve. The vascular pedicle is raised with the fascia of the flexor digitorum superficialis in a distal to proximal direction, and finally the radial artery and venae comitantes (or one deep vein draining into the accompanying veins) are ligated ( Fig. 14.1d ). The donor site is closed by a combination of direct closure and split-skin grafting (Remmert 1995; Fig. 14.1e ).
Indications and advantages:
The radial forearm flap is very good for reconstructions of the oral cavity, tongue, pharynx, and neck, as well as for defects in the face ( Fig. 14.1f–h ) and ear region.
The vascular pedicle has a consistent length ( Fig. 14.1d ).
The flap is pliable.
There is no need to reposition the patient intraoperatively.
Tumor resection and reconstruction can be performed in one operation.
Two teams can work concurrently: one removes the tumor, while the other harvests the flap.
When a radial forearm flap is used for tongue reconstruction, for example, sensation is restored by anastomosing the lateral antebrachial cutaneous nerve to the lingual nerve. A radial forearm flap can be used for reconstructing the cheek ( Fig. 14.1f–h ). A facial forearm flap can be harvested for ear reconstruction ( Fig. 14.1i, j ).
Disadvantages and complications:
The donor forearm must be immobilized for 10 days.
Split-skin grafting of the defect may lead to wound-healing problems in the flexor tendon area, and cosmetic morbidity.
The flap may shrink by up to 25%.
Allen Test
The Allen test is used to determine whether the ulnar artery will adequately supply the hand following ligation of the radial artery. The patient is told to make a tight fist with the affected hand. Then the examiner simultaneously compresses the radial artery and ulnar artery, the patient slowly opens the hand, and pressure on the ulnar artery is released. In an abnormal test, the fingers do not show significant capillary fill (blush) within 5 seconds after ulnar artery release, and a radial forearm flap is contraindicated. A similar test is used intraoperatively. Following the usual dissection of the radial forearm flap and exposure of the axial vascular bundle, the radial artery is clipped at the distal margin of the flap. If oxygen saturation measured on the thumb does not fall below 97%, it is assumed that the ulnar artery is providing an adequate collateral supply, and the radial forearm flap can be raised (Remmert and Sommer 1993).
Groin Flap
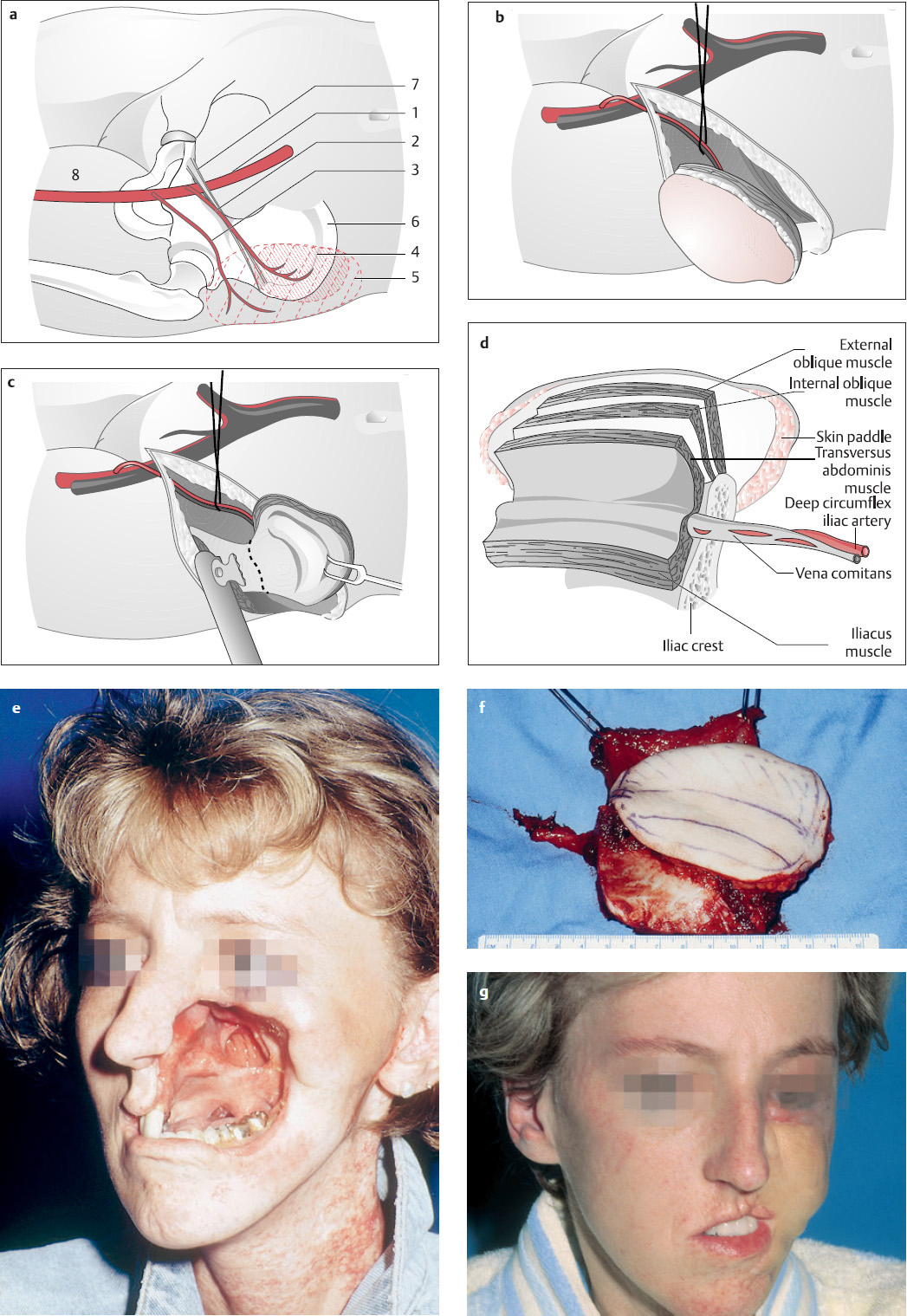
( Fig. 14.2 )
Flap type:
Osteomyocutaneous flap (composite or compound) of the axial pattern type.
Flap components:
Skin, subcutaneous, muscle (internal oblique), bone (ilium). The groin flap can be transferred as a bone graft only (iliac crest bone graft), as a bone graft with muscle, or as a bone graft with muscle and skin (osteomyocutaneous flap).
Use:
Microvascular transfer.
Vascular pedicle:
The osteomyocutaneous flap is supplied by the superficial and deep circumflex iliac arteries. The deep circumflex iliac artery is the more important of the two, arising from the external iliac artery posterior to the inguinal ligament ( Fig. 14.2a , 1). Its vascular pedicle has a length of 80 to 120 mm and a caliber of 3 mm, and chiefly supplies the ilium. In 75% of cases, there is an ascending branch with perforators, which supplies the internal oblique muscle, along with a 2.5 × 8-cm skin area over the iliac crest ( Fig. 14.2a , 4). The superficial circumflex iliac artery ( Fig. 14.2a , 3) arises from the femoral artery 30 mm below the inguinal ligament. Its vascular pedicle has a length of 5 to 20 mm and a caliber of 1.5 mm. The vessel mainly supplies a 12 × 23-cm skin area over the iliac crest ( Fig. 14.2a , 5). If only a small skin paddle is required, the deep circumflex iliac artery ( Fig. 14.2a , 2) is the only vessel that needs to be anastomosed at the recipient site. If a larger skin paddle is needed, the superficial circumflex iliac artery ( Fig. 14.2a , 3) should also be anastomosed (Remmert et al. 1998).
Position:
Supine.
Flap elevation:
First the inguinal ligament, femoral artery, and iliac crest are marked out on the skin ( Fig. 14.2a , 6 and 7). The skin paddle is outlined and its perimeter incised, dividing the skin and subcutaneous tissue down to the abdominal wall musculature. When the skin paddle is raised from the external oblique muscle, an area of muscle ~3 × 8 cm is left on the upper iliac crest. The muscle and skin in this area should not be divided, to preserve the perforator vessels to the skin paddle. After the external oblique muscle has been divided, leaving a flap ~2 to 4 cm wide on the iliac crest, an adjacent internal oblique muscle flap based on the iliac crest is cut to match the size of the defect. The underlying transversus abdominis muscle is divided in the same way as the external oblique muscle, leaving a strip of muscle ~2 to 4 cm wide on the iliac crest. This muscular cuff transmits the deep circumflex iliac artery ( Fig. 14.2a , 2) with its perforators. After the tensor fasciae latae and gluteus medius are separated from the lateral aspect of the ilium, the vascular pedicle is exposed by detaching all abdominal wall layers at the level of the anterior superior iliac spine. The deep circumflex iliac artery arises from the external iliac artery posterior to the inguinal ligament. The vascular pedicle is dissected free, proceeding in a medial to lateral direction as far as the anterior superior iliac spine. Finally, the iliacus muscle is released from the medial surface of the ilium, fully exposing both the medial and lateral aspects of the bone. A bone fragment of the necessary size and shape (determined from a pattern) is cut from the ilium, with an oscillating saw; the vascular pedicle is divided; and the osteomyocutaneous flap is transferred to the recipient site. The donor site is carefully closed in layers, to prevent hernia formation (Remmert et al. 1998).
Indications and advantages:
This flap is used for reconstructions of the mandible, maxilla, cheek, and occasionally the forehead ( Fig. 14.2e–g ).
There is consistent vascular anatomy.
Skin, muscle, and bone can all be reconstructed with one flap.
Bone from the iliac crest provides a good bed for dental implants.
Tumor resection and reconstruction can be performed in one operation.
There is no need to reposition the patient intraoperatively.
Disadvantages and complications:
There is a risk of hernia formation.
With a large skin paddle, both the deep and superficial circumflex iliac arteries must be anastomosed at the recipient site.
Primary closure of the donor site is not possible when a large skin paddle is taken.
Severe pain may occur.
The latissimus dorsi island (see Figs. 12.2 and 12.3 ) and the scapula and parascapula flap (see Fig. 14.4 ) can also be used as a free flap, using the microvascular anastomosing technique.
Transplants Anastomosed Using a Microvascular Technique
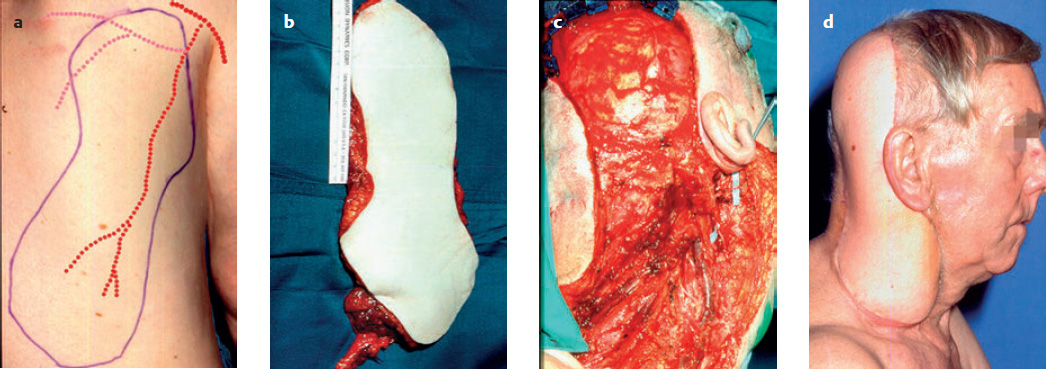
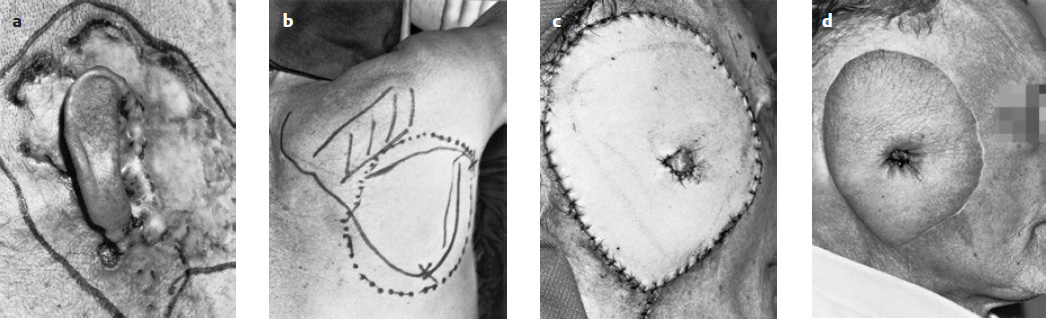
( Figs. 14.3 and 14.4 )
These are, for example, the free latissimus dorsi flap, the radial artery forearm flap (see Fig. 14.3 ), the parascapular flap ( Fig. 14.4 ), or the lateral upper arm flap.
Free transplants anastomosed on the superficial temporal artery and vein, the facial artery and vein, or other vessels are well suited to cover defects of the auricular region ( Fig. 14.4 ) and are now the techniques of first choice (Weerda 2001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree