Free Flap for Hemi-Tongue Reconstruction
Carrie K. Chu
Peirong Yu
DEFINITION
The tongue is a highly functional organ responsible for speech, deglutition, taste, and airway protection.
Glossectomy defects following oncologic resection represent the most common indication for oral cavity reconstruction.
Glossectomy defects can be partial, subtotal, or total. In general, defects that exceed one-third of the tongue or include significant floor of mouth resection usually require free flap reconstruction. Small defects may be closed primarily or skin grafted.
Goals of partial glossectomy reconstruction include provision of soft tissue coverage, restoration of intelligible speech, restoration of oral intake, maintenance of patent airway, and separation of the oral cavity from the structures of the neck when required. Re-establishment of sensation is a secondary but important goal.
ANATOMY
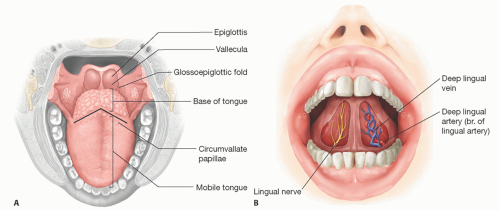
The tongue is composed of two anatomic components. The anterior two-thirds within the oral cavity is the oral (or mobile) tongue, whereas the posterior third within the oropharynx is the base of the tongue. The boundaries of the base of the tongue include the circumvallate papillae anteriorly, the glossoepiglottic folds laterally, and the vallecula and the lingual aspect of the epiglottis posteriorly (FIG 1A).
General sensation to the anterior two-thirds of the tongue is supplied via the lingual nerve (CN V3). The chorda tympani (CN VII), which accompany the lingual nerve, are responsible for taste.
Taste and sensation for the posterior one-third tongue derive from the glossopharyngeal nerve (CN IX).
Motor innervation of the intrinsic and extrinsic tongue musculature is via the hypoglossal nerve (CN XII), with the exception of the vagus nerve (CN X) for the palatoglossus muscle. The floor of the mouth, the ventral sulcus, and the lateral gutter facilitate the excursion of tongue muscle for its intelligent functions. The tip of the tongue easily touches the palate for precise pronunciation (FIG 1B).
The lingual arteries, branches of the external carotid artery, provide vascular supply to the tongue. A secondary blood supply arises from the tonsillar branch of the facial artery and the ascending pharyngeal artery. Venous drainage is via the lingual veins into the internal jugular vein.
PATHOGENESIS
Oral cavity and oropharyngeal cancers, including squamous cell carcinoma and minor salivary gland carcinomas, are the main indications for hemiglossectomy.
Risk factors for oral cavity and oropharyngeal cancers include tobacco and/or alcohol use, human papillomavirus
infection, elderly age, male sex, inhaled environmental or occupational exposures, and poor oral/dental hygiene.
Oral tongue cancers are typically treated with up-front surgical resection, whereas base of tongue cancers are frequently managed with neoadjuvant radiation followed by surgery as indicated.
Glossectomy potentially compromises tongue function including speech, deglutition, and taste. The base of the tongue is more important for swallowing function, whereas the oral tongue is more important for speech and food manipulation. Restoration of these functions while preserving airway patency represents the main objective of hemiglossectomy reconstruction.
PATIENT HISTORY AND PHYSICAL FINDINGS
Symptomatology review should be performed including pain, swallow dysfunction, oral intake status, speech alteration, otalgia, paraesthesias, altered tongue mobility, and airway obstruction.
History of neoadjuvant therapies should be noted. In cases of recurrence, records concerning prior surgical history, including neck dissection, should be reviewed in detail.
The surgeon should be aware of factors that may compromise recipient vessel availability including radiation and prior cervical lymphadenectomy.
Medical comorbidities and substance abuse history are both highly prevalent in this patient population.
Occupation, hobbies, physical activity level, and hand dominance should be queried to select an optimal donor site.
Head and neck examination should include the following elements:
Neck range of motion
Palpation of the facial artery
Quality of neck skin
Interincisal opening distance
Dental hygiene and presence of caries
Cranial nerve function (V, VII, XII)
IMAGING
Computed tomography studies with contrast are reviewed for primary tumor dimensions including extension past midline, adjacent structures, and neck vessel patency.
SURGICAL MANAGEMENT
Partial glossectomy defects smaller than one-third of the native tongue without a floor of mouth defect can typically be reconstructed with primary closure or skin grafting.
The latter may exhibit partial graft loss but ultimately will serve as a biologic dressing that allows for eventual mucosalization.
Hemiglossectomy defects benefit from free flap reconstruction using a thin, pliable flap to avoid restricting functional tongue mobility.
These goals are distinguished from those associated with subtotal or total glossectomy, where the objective is to render a bulky flap reconstruction that provides adequate palatal contact to avoid aspiration and enhance speech intelligibility.
Consideration should also be given to sensory reinnervation.
Resection of the floor of the mouth combined with neck dissection creates a communication between the oral cavity and the neck along the lingual cortex of the mandible.
These defects, even if they involve less than one-third of the tongue, are best reconstructed with a flap to minimize the risk of infection and fistula formation, which can potentially delay crucial adjuvant therapy.
The pectoralis major muscle or myocutaneous flap is a pedicled option for hemiglossectomy reconstruction. Its bulk, potential tethering and downward retraction are disadvantages for hemiglossectomy reconstruction. The functional outcomes are usually compromised.
Therefore, it is usually reserved for salvage after a failed free flap reconstruction or for use in high-risk cases deemed unsuitable for free flap reconstruction.
Preoperative Planning
The potential functional impairment should be thoroughly discussed with the patient and family because these deficits will not only significantly affect their quality of life but their profession as well.
Referral for dental extractions in preparation for flap inset and adjuvant radiation may be appropriate if significant caries or nonviable teeth are identified.
The availability of blood products based on preoperative type and cross should be confirmed.
Potential donor-site assessment should be carried out including soft tissue thickness and quality of the upper extremity and thighs.
Hand dominance should be documented.
The radial and ulnar aspects of the forearm should be assessed for hair growth. A less hairy skin flap is preferred.
Flap choices
In patients with very thin thighs, the anterolateral thigh flap is the first choice due to its minimal donor-site morbidity with the exception of young female patients.
Otherwise, the ulnar artery perforator flap is the first choice followed by the radial forearm flap as the ulnar artery flap creates a less conspicuous donor-site scar.
The most common flaps for hemiglossectomy reconstruction are described in this chapter, but consideration may be given to numerous alternative donor-site options that would provide thin, pliable tissue to meet the goals of reconstruction.
These include, but are not limited to, lateral arm, profunda artery perforator, anteromedial thigh, and medial sural artery perforator flaps.
Preoperative nutritional status should be evaluated.
Some patients may have lost significant weight due to pain and inability to consume oral diet.
A percutaneous gastrostomy feeding tube may be necessary to provide adequate nutritional support before surgery.
Antibiotic prophylaxis is administered before incision. For defects involving the aerodigestive track, 3 g of ampicillin/sulbactam is our antibiotic of choice, which is redosed every 6 hours.
Positioning
The patient is placed in supine position, typically with the operating table reversed by 180 degrees.
Placement of an underbody warmer avoids physical interference with multiple surgical sites.
The dominant arm is tucked, while the contralateral potential donor arm is prepped circumferentially toward the axilla.
The arm is secured to the chest drapes to provide room for the extirpative team.
It is then placed on an arm board for flap harvesting.
The thighs are also prepared for potential thigh flap or as a skin graft donor site.
The lower abdomen/groin may be prepared as a full-thickness skin graft donor site to cover forearm flap donorsite defect.
A two-team approach is possible when harvesting a thighbased flap.
With a forearm flap, flap elevation may require delay until the extirpative team completes the resection and neck dissection.
TECHNIQUES
▪ Recipient Site Preparation
While waiting for margins, the defect is assessed, and recipient vessels are dissected out.
A Dobhoff feeding tube is inserted into the stomach intraoperatively if percutaneous gastrostomy is not indicated.
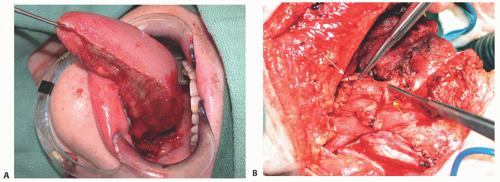
The length of the surgical defect is measured from the tip of the remaining tongue to the posterior limit, which can be in the base of the tongue or immediately above the epiglottis (TECH FIG 1A). In the latter case, there will also be a defect in the lateral pharyngeal wall.
The viability of the remnant tongue should be assessed as well. However, any debridement should be conservative and limited to tissue that is definitively nonviable. Marginal areas may benefit from time for recovery and demarcation postoperatively.
The width of the defect includes the tongue as well as the floor of the mouth. A flap width of 6 to 8 cm is usually required to adequately recreate the lateral sulcus and provide enough surface area coverage.
A neck dissection is commonly performed along with a glossectomy.
Extra soft tissue is included in the flap design to obliterate any submandibular or upper neck dead space.
The transected end of the lingual nerve should be explored for potential sensory reinnervation (TECH FIG 1B).
The lingual nerve is the optimal recipient for sensory reinnervation of the neotongue compared to other options such as the inferior alveolar nerve and the greater auricular nerve.
It is usually 2 mm in diameter and can be found along the lingual cortex and anterior to the angle of the mandible.
The lingual artery is often exposed and divided during glossectomy. With a diameter between 2 and 2.5 mm in most cases, the lingual artery represents an ideal recipient target.
The facial artery is often divided as well during a neck dissection and can be used as a recipient artery. Its diameter is similar to that of lingual artery.
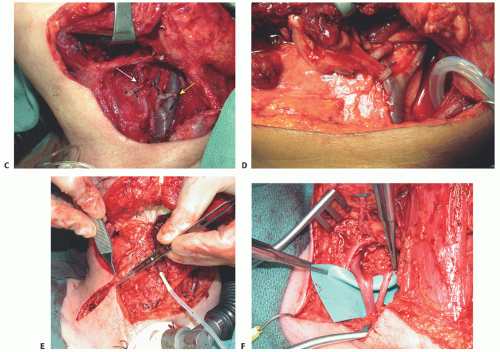
The artery is dissected back to its origin from the external carotid artery and brought under the posterior belly of the digastric muscle (TECH FIG 1C), which can be divided if it facilitates improved vessel access.
The curved portion of the artery is removed to allow for unimpeded inflow, leaving only a 1-cm stump on the external carotid artery.
Sometimes, the lingual and facial arteries share a common trunk, which may be more suitable as a recipient vessel as the vessels may become small after the bifurcation. The superior thyroid artery is usually much smaller in Western populations and is usually undisturbed during ablative surgery, thus less desirable as a recipient vessel.
The author’s preferred recipient vein is a branch of or the common facial vein stump on the internal jugular vein depending on the flap vein size. A vein coupler or flow coupler is used for end-to-end anastomosis (TECH FIG 1D).
If no facial vein branches are available, an end-to-side anastomosis on the internal jugular vein itself is a viable option.
If the internal jugular vein is also unavailable, the external jugular vein, if it remains in good condition, is the next choice.
The transverse cervical vessels are usually available even in the vessel-depleted neck1 and can be easily reached with a radial forearm flap or anterolateral thigh flap without the need for vein grafting (TECH FIG 1E,F).
Finally, the internal mammary vessels and the use of a cephalic vein turn-up can serve as the last resort.
▪ Flap Harvest
Radial Forearm Free Flap
A flap with a width of 6 to 8 cm and length of 10 to 12 cm is usually required for a true hemiglossectomy defect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree