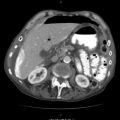
Fig. 82.1
Confirmation of a complex vascular injury that caused exsanguinations. Patient demised on arrival to the emergency department. ERT was not successful

Fig. 82.2
En bloc dissection showing a fatal GSW to the arch of the aorta
Fig. 82.3
Missed failed ETT tube exchange contributing to death in a multiple stab on a short obese neck trauma patient. See airway marked by the probe

Fig. 82.4
Stab/penetrating incised wounds with clean-cut sharp edges to the wounds

Fig. 82.5
Frank pus on and in the brain complicating skull fracture and penetrating head injury
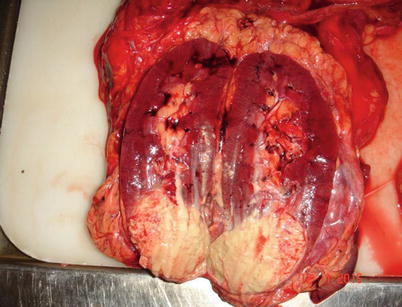
Fig. 82.6
Incidental finding of a renal tumour in a penetrating abdominal trauma not related to the demise of the patient
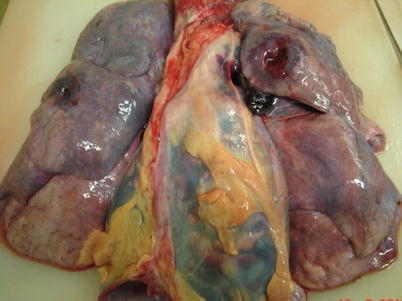
Fig. 82.7
Post-mortem confirmation of a transmediastinal GSW, en bloc dissection

Fig. 82.8
Tubes and lines left in situ for a patient that demised shortly after the procedure, this allows for confirmation of correct placement of these lines
82.2 How Forensic Science Has Developed Over the Years
The work of investigating criminal deaths by the police used to rely on very unscientific methods. No two investigators could reliably arrive at the same conclusion because of personal prejudice and bias in the process. In order to improve the quality of policing and give credible ethical support to the work they did, it was decided to use more credible and reproducible methods. A decision to add science to police work was noted to reduce or eliminate speculation, innuendo and partisanship and result in reproducible, factual information that could be presented to the courts.
It became clear to the police that they needed someone who had knowledge of the human body to aid in their investigations. They chose the medical doctor as someone with special knowledge in anatomy and pathology of the body. In Northern Italy the courts as early as the thirteenth century were appointing medical experts to advise them. By the sixteenth century, medical evidence was being given in courts. As a result of a rise in violent crimes and infanticide, the Bishop of Bamberg ordered the compilation and publication in 1507 of Constitutio Bambergensis Criminalis. In this publication, it was proposed that a medical doctor be involved and called in, in all violent deaths, to take notes on the position of wounds and their nature and to draw conclusions to be presented at court.
In 1516 Brandenberg followed suit with another publication. In 1533 the Constitutio Criminalis Carolina was ordered by the Emperor Charles V and had to be applied over Europe. In this publication more emphasis was put on forensic psychiatry, reporting on the mental state of a perpetrator before trial.
Medical practitioners were extensively involved in police investigations and were expected to give an opinion on a lot of things, even outside the scope of their specific training, as long as it was in the medical field. They pronounced on a wide range of things: medical issues, surgical issues, ballistics, toxicology, genetics etc.
Key definitions |
|---|
Forensics: for the purposes of the court, pertaining to the law |
Forensic medicine and pathology: The investigative element of medicine, for purposes of the law. It includes both forensic pathology and clinical forensic medicine |
The forensic pathologist is a medical doctor who has specialised in forensic pathology to work on the deceased as patients, and not the living, the end result being to establish a cause of death, get evidentiary material from or off them, etc., to name a few |
The clinical forensic doctor works with the living victims of trauma and alleged perpetrators or suspects in criminal or potential criminal cases, primarily to document injuries and get evidentiary material from or off them etc. |
The necropsy/autopsy/post-mortem examination is either academic or forensic. This is the medical process of performing an examination on the body of a deceased in order to establish amongst others: a cause of death, disease extent, evaluate effect of therapy, confirm identity where needed, etc. This is at the request of either the doctor in a clinical setting, the family for, e.g. cremation purposes or the police in the event of foul play |
The forensic necropsy/autopsy/post-mortem examination is done when there is foul play or it is suspected. The state police are involved |
The terms autopsy and post-mortem examination are used interchangeably, implying a thorough examination of the body externally and internally and to retain any specimens that may aid in coming to a conclusion regarding the cause of death |
Whenever a partial autopsy examination is performed, it should be stated clearly in the report and, if applicable, the reasons for it stated upfront |
For example, viewing autopsy, to denote the external examination only, was done. This is likely in the event of a natural death which was not sudden or unexpected, and while not forensic in nature, there was no one else available to sign the death notification form. Limited autopsy to denote that the examination was hampered by, for example, an infectious disease like tuberculosis in the one or more organs, but elsewhere in the body, the autopsy was carried out as per usual |
Incomplete autopsy would be one where the examination will be completed in the following day(s), pending someone critical to the case arriving, a medical information report coming or police investigation report supplied relating to the body |
High-risk limiting autopsy is one where just the necessary specimen(s) is taken to establish or confirm the suspected cause of death, where a communicable condition is suspected. If it is deemed necessary to, further examination may be done on receipt of the results |
The forensic scientist is generally not a medical doctor, but one trained to be a supportive team member in the police or medical side to assist with the medicolegal investigations |
82.3 Trauma and Clinical Forensic Medicine
Patient presentation to a health facility may be variable from an awake consenting adult to a moribund patient.
The living forensic victim of trauma has to consent to be seen by the doctor as in the usual patient-to-doctor relationship. Their full consent and participation are essential, and towards this there are trauma counselling centres with trauma counsellors, social workers and forensic nurses trained to empathise and reassure victims of accidental or criminal trauma before treatments and procedures. The nature of the trauma directs the examination and the treatment prescribed. The police are often initially or soon hereafter involved, and if there is to be a police case opened, the examination will help verify the incident, quantify the injuries and retrieve potential forensic evidence off the victim. Depending on the injuries, the victim will either be admitted to the hospital or discharged.
The forensic suspect trauma patient irrespective of the presentation will often be accompanied by police, in hand and or ankle cuffs, or shackled to the stretcher he/she is lying on. As the suspect is under police custody and a ward of the state, the request and consent for the examination will be rendered by the police. In addition to the medical examination, there may also be a need for collection of biological samples. Depending on the injuries, the suspect will be kept in the hospital or discharged under police custody.
The forensic suspect (with no obvious injuries but who needs to be examined for other legal reasons) is handed back to the police at the end of the medical assessment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree