Forehead Skin Flaps
J. S. P. WILSON
N. M. BREACH
EDITORIAL COMMENT
Historically, the forehead flap is one of the first axial flaps described, and it achieved enormous importance in head and neck reconstruction. Its major drawback is the secondary defect, which consequently led to the exploration and use of other flaps. Nevertheless, because of the reliability of its vascular supply, the excellent color match (particularly for resurfacing the cheeks and upper lips), and its proximity to the face, it should be given serious consideration by reconstructive surgeons.
The forehead flap provides the largest area of donor skin with matching color and texture to facial skin (Fig. 106.1). It is one of the safest cutaneous flaps available in reconstructive surgery (1, 2).
INDICATIONS
A forehead flap is long enough to reach any part of the ipsilateral face and will provide cover to the carotid artery in the upper neck. It also can be used to reconstruct the cervical esophagus, provided that it is passed under the malar region and that the body of the mandible is removed. The elderly patient is not confined to bed with a limitation of neck movements with the use of a forehead flap.
Skin taken from other regions for facial reconstruction does not provide a good color and texture match and does not supply the deep support necessary, as in the reconstruction of a nose. The difference in color and texture is difficult to disguise.
ANATOMY
A knowledge of the arterial pattern of this flap and its variations is essential to enable the full use of the forehead skin in reconstructive surgery (3). The lateral forehead is supplied by the zygomatic and anterior branches of the superficial temporal artery. The main artery arises as a terminal branch of the external carotid artery. It comes to lie in a superficial plane just anterior to the tragus of the ear (4). Proximal to this, it lies deep in the parotid gland, which prevents its further mobilization.
The superficial temporal artery ascends superficial to the zygomatic arch and soon divides into the anterior superficial temporal branch (ASTB), which passes upward and medially into an ascending posterior superficial branch that passes vertically to supply the scalp.
Cadaver studies revealed that in 80% of cases the zygomatic branch arises from the trunk of the superficial temporal artery, and in the remaining 20% of cases, it arises from the anterior branch (Fig. 106.2) (5, 6). It also has been found that the point of origin of the zygomatic artery was 60% above the zygomatic process, 32% over the zygomatic process, and 2% below the level of the zygomatic process (7). Failure to include a large zygomatic branch may be the reason for reported cases of failure. The ASTB sends perforating branches through the frontalis muscle that is included in the flap to supply the skin. The flap should therefore be regarded as a musculocutaneous flap.
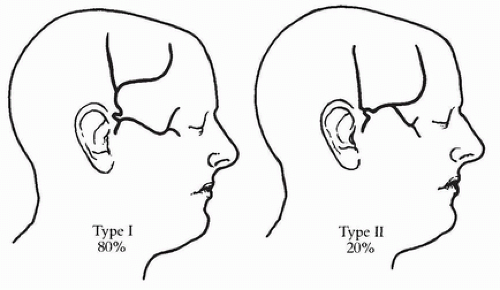 FIGURE 106.2 Variations in terminal branching of the superficial temporal artery (6). |
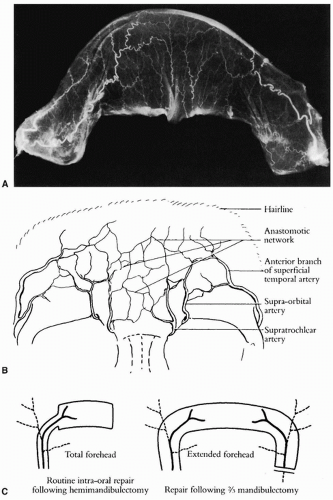
Centrally, the forehead is supplied bilaterally by the supratrochlear artery, which becomes superficial 1 cm medial to the inner canthus, and the supraorbital artery, which is palpable at the junction of the lateral two thirds of the rounded supraorbital ridge with the sharp medial one third. Both vessels are branches of the ophthalmic artery and then pass vertically upward to the scalp.
Micropaque injections of the superficial temporal artery (STA) in cadaver specimens show the rich anastomotic plexus between these vessels (Fig. 106.3). The blood supply to the forehead is therefore basically four interconnecting vascular territories or angiotomes.
FLAP DESIGN AND DIMENSIONS
If Micropaque is injected into one ASTB, the dye flows across the forehead into the supraorbital and supratrochlear angiotome and hence to the contralateral STA, in which the flow is reversed (Fig. 106.3A). This allows the creation of an extended flap passing from one malar bone to the contralateral malar bone (Fig. 106.3C). The flap is 25 cm long in an average adult and can be carried safely on a pedicle no wider than 2 cm at its base. It is obvious that this pedicle, based just anterior to the tragus containing the STA, is highly mobile (8) (Fig. 106.3C). This flap, provided that the STA and its small accompanying veins are intact, is perfectly safe in clinical practice (Fig. 106.4).
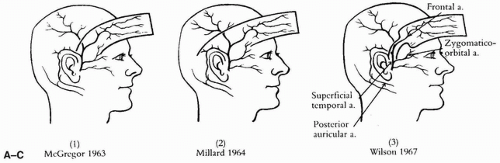
The course of the STA must be identified and marked on the forehead. The pedicle of the flap must be of sufficient length to transpose the flap without tension. The maximum mobility of the flap is achieved by using a narrow 2-cm pedicle, including the STA. If the STA has been previously sacrificed, a broad-based McGregor flap will be required, which should be delayed (9). If there is any doubt as to the viability of the flap, a flap that includes the postauricular vessel or a posteriorly based flap can be used, but this reduces flap mobility (10, 11) (Fig. 106.5).
Intraoral Reconstruction (12)
The flap should be of a correct size to repair an intraoral defect. Too much tissue provides excessive bulk that impedes swallowing, and too little leads to secondary deformities and oral disability. There are three basic shapes. The butterfly can repair defects of the posterior tongue to allow mobility, the other wing closing the defect in the cheek. The distal extension provides cover and seal, being supported by the cut end of the mandible. The narrow flap repairs central and alveolar defects. The repair following total glossectomy should be in the form of a shield (Fig. 106.6).
Neck Reconstruction
The dependability of the vascular supply of the forehead flap is such that it can be used to cover an exposed carotid artery in the neck (13). The extended forehead flap can be cut long enough to reconstruct the cervical esophagus safely, provided that the resection of the tumor had required sacrifice of the hemimandible (Fig. 106.7).
OPERATIVE TECHNIQUE
The STA lies superficial to the epicranial aponeurosis and thus is easily identified when the flap is raised on its narrow pedicle. As the flap is raised, care must be taken not to lift the periosteum from the frontal bone, and coagulation diathermy should be minimal. If either of these points is not observed, delayed healing of the applied skin graft will result.
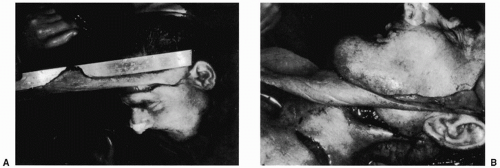 FIGURE 106.4 A,B: Clinical example of extended forehead flap showing that it can reach to the cervical region. (From Narayanan, ref. 17, with permission.) |