Organ
Symptoms
Skin
Erythema, urticaria, angioedema, pruritus, burning, sensation, eczema
Mucous membrane
Eye symptoms: Conjunctival hyperemia and edema, pruritus, lacrination, blepharedema
Nasal symptoms: Rhinorrhea, nasal congestion, sneezing
Oral symptoms: Discomfort/swelling of the oral cavity, lips, or tongue
Respiratory organs
Discomfort/itch/tightness in the pharynglolarynx, hoarseness, dysphagia, coughing, wheezing, retractive breathing, feeling of chest tightness, dyspnear, cyanosis
Digestive organs
Nausea, vomiting, abdominal pain, diarrhea, hematochezia
Nerve
Headach, lowed vigor, urrest, impaired consciousness
Circulatory organs
Decreased blood pressure, tachycardia, bradycardia, arrythmia, coldness of limbs, pallo(peripheral circulatory failure)
Systemic
Anaphylaxis and anaohylactic shock
).
Anaphylaxis is defined as general symptoms affecting >2 target organs without hypotension, whereas anaphylactic shock is defined as anaphylaxis with hypotension and unconsciousness. Anaphylaxis and anaphylactic shock are life-threatening events for which early responses and treatments are needed.
28.2.2 Anaphylaxis [1, 2, 4–6]
Anaphylaxis is defined as a strong, life-threatening whole-body reaction caused by internal exposure to a specific antigen. The sources of these antigens include food, drug, insect venom, latex, and transfused blood and can cause IgE- or non-IgE-mediated reactions. Table 28.2 presents the grades of anaphylaxis according to the Japanese Society Academy of Allergy (Table 28.2
). In Japan, shock-related deaths are mainly attributable to drugs and insect venom. However, common anaphylaxis occurs most frequently in the context of FA. Hen’s egg, cow’s milk, wheat flour, shellfish, and soybeans are the main causative agents in Japan. However, peanut, tree nuts, fish and shellfish, hen’s egg, and cow’s milk are the main causative agents in Europe.
Organs | 1 (Mild) | 2 (Moderate) | 3 (Severe) |
|---|---|---|---|
Skin | Lovalized urticaria, exanthema, wheal pruitus, Swallen, eye lid or lip | Generalized urticaria exthanthema, wheal pruritus | (−) |
Swollen face | (−) | ||
Gastrointestinal tract | Pruritus of the throat or oral cavity | Throat pain | (−) |
Mild abdominal pain | Moderate abdominal pain | Cramps | |
Nausea, emesis, diarrhea | Recurrent emesis, diarrhea | Continuous emesis, loss of bowed control | |
Respiratory tract | Intermittent cough, nasal congestion, sneezing rhinorrhea | Recurrent cough | Persistent cough hoarseness, “barking” cough |
Chest tightness, wheezing detectable via auscultation | Audible wheezing, dyspnea, cyanosis, saturation < 92%, awallowing or speaking difficulties, throat tightness, respiratory arrest | ||
Cardiovascular | (−) | Pale face, mild hypotension, tachycardia (increase >15 beats/min) | Hypotension, dysrthythmia, severe bradycardia, cardiac arrest |
Neurological | Change in activity level, tiredness | Light-headedness, feeling of “pending doom”, sommunolence, headache | Confusion, loss of consciousness, incontinence |
28.2.3 Epidemiology
A 2012 large-scale Japanese investigation reported the following FA prevalence rates: infants (<1-year-old), 5–10%; 1–6-year-old children, approximately 5%; and 6–12-year-old children, 1.5–3%. In other words, infants were most likely to exhibit FA, and the prevalence tended to decrease with aging. In Japan, hen’s egg, cow’s milk, and wheat flour are the main causes of FA. In older children, shellfish, fruits, and buckwheat have been identified as causative agents [1, 2, 5, 7].
In contrast, the prevalence of FA among adults has seldom been investigated in Japan. Recently, however, reports of adult FA cases have increased. In addition, self-reports of FA have been investigated on websites. The overall prevalence was 1.9–10%, and shellfish was the most frequent causative agent. Additional larger-scale investigations are needed in the future [8]. In Western countries, the following FA prevalence rates have been reported: children, 1.4–5.5% [9–11]; adults, 0.8–3.2%; and all age groups, 1.4–3.6% [12, 13]. The prevalence rates detected during the double-blind placebo-controlled food challenge (DBPCFC) [9–14] were lower than those determined using other types of diagnosis [11]. In adult patients with FA, inadequate attention to a genuine food allergy sometimes would be risk factors for anaphylaxis/anaphylaxis shock [15].
28.3 Atopic Dermatitis and Food Allergy in Infants
28.3.1 Clinical Features of Food Allergy
28.3.1.1 Neonatal and Infantile Gastrointestinal Allergy [1, 2]
GI tract allergy is a type of FA. However, the symptoms of vomiting, bloody stool, and diarrhea are caused by IgE-independent mechanisms. Cow’s milk was the most prevalent cause.
Many affected patients will naturally outgrow this disease.
28.3.1.2 Infantile Atopic Dermatitis Associated with Food Allergy [1, 2, 16–19]
The onset of this type of FA is most commonly observed in infants and is preceded by AD. Avoidance of the causative food generally leads to improvements in skin symptoms [19]. Additionally, FA symptoms tend to decrease naturally with age [16–18, 20]. Hen’s egg, cow’s milk, and soybean are the main causative agents of FA-related AD in Japan [1, 2]. Comorbid FA and AD occur at a high frequency. Generally, AD is considered the first step in the “allergic march” [1–3] and is followed by asthma, allergic rhinitis (AR), and FA in approximately 50% of cases. Furthermore, up to 80% of children with AD will reportedly develop AR or asthma later in childhood [1, 2, 16, 20].
Tupker et al. suggested [21] that inhalation of house dust mites (i.e., respiratory route) could induce dermatitis episodes in patients with AD. The authors concluded that a causal relationship might link bronchial and skin reactions.
We have experienced the same situation in clinical practice.
Allergic (Atopic) March and Food Allergy
In infants, various allergic diseases, including FA, AD, asthma, and AR, occur sequentially as part of the natural progression known as the “allergic (atopic) march.” AD precedes FA, and other allergic diseases will develop over a period of several years [1, 2, 16, 22, 23]. Recently, dysfunction in filaggrin, a skin barrier component protein, has been reported as a cause of onset for various allergic diseases (i.e., “allergic (atopic) march”) [24, 25]. Recently dysfunction of thymic stromal lymphopoietin (TSLP) in epidermal barrier on atopic march progression has also been reported [26].
Filaggrin Function and Food Allergy [27–30]
Filaggrin plays an important role as a skin barrier component. Filaggrin loss-of-function (FLG-LOF) mutations have been identified as a risk factor for allergic sensitization, atopic eczema, AR, and asthma. These mutations also lead to epidermal barrier dysfunction and increased trans-epidermal water losses (TEWLs). Increased TEWL can lead to clinical AD in patients at a high risk of atopy.
A combination of FLG-LOF mutation and allergic sensitization in childhood increases the risk of eczema. Recently, an association between FLG-LOF and food allergy has been investigated in many studies. FLG-LOF mutations have been reported to associate with FA in older children through mechanisms involving eczema and food allergen sensitization (FAS). Specifically, FLG-LOF leads to eczema, which in turn leads to early childhood FAS; this latter condition increases the risk of FA in later life.
Immediate-Type Food Allergy [1, 2, 4, 5]
These symptoms occur immediately (i.e., within 2 h). Infant FA without AD may develop, as the foods that commonly cause AD, including hen’s egg, cow’s milk, and wheat flour, often cause the preceding FA; furthermore, buckwheat, peanuts, fish, shellfish, and fruit become involved with age. Generally, it is difficult to outgrow this condition.
Adult Food Allergy
Adult patients with FA often exhibit immediate-type disease, are less likely to have a history of infant FA, and seldom exhibit continuous symptoms since childhood [1.2]. These patients generally consult the Department of Allergology/Dermatology for the first time after a sudden onset of skin and mucus membrane symptoms after a meal or may be referred from the emergency department (ED) immediately after treatment for anaphylaxis/anaphylactic shock. Wheat flour, shellfish, fresh fruits and vegetables, and, occasionally, Anisakis [31] are the main causes of allergic symptoms; however, the etiology is often unknown because patients only consult the hospital for a single event. These patients exhibit not only FA but also a comorbid allergic disease. Patients with a particular type of FA, such as food-dependent exercise-induced anaphylaxis (FDEIA), secondary pollen fruit syndrome after pollinosis, latex fruit syndrome (LFS), and other occupational FA, which involve airway and cutaneous sensitization to low concentrations of biological antigens, often consult the hospital.
A family history of various allergic diseases is an important risk factor for young adult with current AD and multiple atopic diseases. In addition, severe seasonal reactions are observed in patients with rhinoconjunctivitis and asthma [32–34]. During 3 months, elimination of causative foods, cheese, yogurt, and chocolate improves more or less some of AD symptoms [35].
28.3.2 Particular Food Allergy
28.3.2.1 Pollen-Food Syndrome, Oral Allergic Syndrome
Pollen-food syndrome (PFS) is a type I IgE-dependent FA that is generally localized to the oral mucosal membrane. The main causative agent is fresh vegetables or fruit. Patients with PFS often have complicating pollinosis; accordingly, PFS is also called pollen-associated syndrome [36, 37].
Patients with birch pollinosis in Hokkaido manifest a type I FA reaction after eating fruits from the rose family, which exhibit cross-reactivity with birch pollen antigen. Mild oral symptoms are common, although life-threatening anaphylaxis may occur, especially during the pollination season. Approximately one third of patients with PFS have concomitant AD. Therefore, asymptomatic individuals with AD may experience an exacerbation of AD even after eating cooked antigens [38, 39]. In Japan, rose family fruits are the most common cause of PFS [40].
28.3.2.2 Food-Dependent Exercise-Induced Anaphylaxis
FDEIA is induced in response to a combination of intake of a particular food and exercise; either alone will not induce anaphylaxis. IgE-mediated anaphylactic symptoms are induced within 2 h after eating the causative food and performing exercise. FDEIA is not common; it occurs in some adolescent and young adult patients in response to exercise and the intake of mainly wheat flour and shellfish, or occasionally fruit. More intense exercise and/or a larger quantity of causative food correlate with more severe symptoms [41–44]. Moreover, the use of nonsteroidal anti-inflammatory drugs (NSAIDs) exacerbates the severity of anaphylaxis [45, 46]. In Japan, many researchers have reported on FDEIA but not FDEIA-related AD [47]. Measurement-specific IgE antibodies to ω − 5 gliadin are useful for the diagnosis of wheat-dependent exercise-induced anaphylaxis [48, 49].
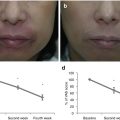
28.3.2.3 Accidental Hydrolyzed Wheat-Dependent Exercise Anaphylaxis
In Japan, the presence of hydrolyzed wheat protein in facial soap and consequent induction of wheat allergy responses, including wheat-dependent exercise-induced anaphylaxis (WDEIA), has become a social issue. People who used the affected soaps experience wheat anaphylaxis caused by transdermal or transmucosal sensitization to the hydrolyzed wheat proteins. Some reports suggest that surfactants might aggravate skin permeability. This case suggested that we should understand the risk of skin sensitization to non-dietary food antigens [50–54]. Oatmeal for skin product for AD has occurred anaphylaxis accidentally, too [55].
28.3.2.4 Latex Fruit Syndrome (LFS)
Approximately 30–50% of patients with latex allergy will exhibit concomitant type I FA symptoms after the intake of fresh and/or processed fruits with cross-reactivity to latex, such as chestnuts, bananas, and kiwifruit. Anaphylaxis, asthma attack, urticaria, and oral allergy syndrome may be induced. This allergic reaction is known as LFS. Medical workers with individual atopic reactions, patients with spina bifida who undergo recurrent procedures involving latex, and workers who use latex gloves occupationally are at a high risk of LFS [56–58]. Although patients with AD are considered high-risk, a recent report suggests that these patients are less likely to be sensitized to latex and consequently develop LFS [59]. On the other hand, a case report described a patient with AD and concomitant FDEIA who quickly became sensitized to latex and developed a delayed-type latex allergy [60]. Medical advice regarding the use of latex leads to improved AD symptoms in affected patients. Generally, AD patients could potentially develop various allergic symptoms. LFS is a frequent type of FA and an important risk factor for occupational allergy [61].
28.3.2.5 Occupational Food Allergy
Some patients with “bakery asthma” develop secondary WDEIA and/or wheat flour FA, similar to workers who develop an occupational latex allergy. Workers with atopic factors are at a high risk of developing allergic disease following sensitization to even low concentrations of occupational food antigens [62]. In particular, AD may cause patients to change their occupation [63]. We must understand the social and individual burdens of AD and consider the quality of life related to health.
28.4 Diagnosis [1, 2, 64–68]
- 1.
Medical interview: suspicious types of food, intake, induced symptoms, exercise, NSAIDs, recurrent symptoms, individual life habits and circumstances, occupation, environment are checked.
- 2.
Differential diagnoses (e.g., contact dermatitis, collagen disease) must be eliminated.
- 3.
Skin test (in vivo): The skin prick test, which is safe and accurate, is recommended for both infants and adults. For patients with AD, an atopy patch test for food allergens is available. Medical treatment must be stopped for several days before the skin prick test. A prick-by-prick test, which directly pricks patients with food juices, is used for OAS patients. Even if the SPT is negative, allergic symptoms are occasionally induced.
- 4.
Serum specific IgE antibody (in vitro): This diagnostic test is commonly used for both infants and adults to quantitatively measure FA-specific IgE. A positive result indicates sensitization to a specific food allergen, although this does not always correspond to actual allergic symptoms. For some food allergens, specific IgE levels correlate with clinical symptoms.
- 5.
Basophil histamine release test (in vitro): This specific diagnostic test measures the concentration of histamine released from peripheral eosinophil blood cells and reflects strong reactions to specific food allergens in vivo. As for SPT, medical treatment must be stopped before HRT. HRT should not be performed more than 1 month after an episode of anaphylaxis.
- 6.
Elimination test: Suspected foods are eliminated for approximately 2 weeks to determine the effect on allergic symptoms (e.g., improvement). Nursing mothers of affected infants should also eliminate the suspected foods.
- 7.
Get Clinical Tree app for offline access
Oral food challenge test: This is the most reliable diagnostic test for FA. However, some risk factors induce severe allergic symptoms, including anaphylaxis; therefore, we must ensure official notification and attain standard procedures for the challenge test.
- (a)
Safety: This test must be conducted under the guidance of professional medical doctors and nurses who are prepared to provide emergency care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)