Floor of Mouth Reconstruction
George N. Kamel
J. Alejandro Conejero
Evan S. Garfein
ANATOMY
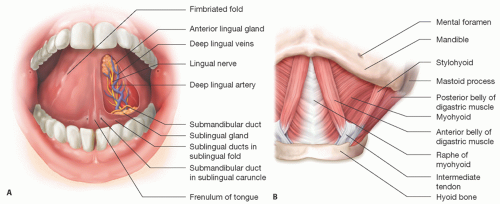
The floor of mouth is a U-shaped mucosal structure covered by squamous mucosa that is bordered by the alveolar ridge of the mandible and extends posteriorly to the anterior tonsillar pillar (FIG 1A).
Medially, the floor of the mouth (FOM) merges with mucosal, ventral surface of the tongue to the level of the frenulum, which divides the floor into two oval spaces.
The FOM contents include the sublingual salivary glands, submandibular ducts, oral component of the submandibular salivary gland, the geniohyoid and genioglossus muscles, and the lingual and hypoglossal nerves.
The lingual nerve provides sensation to the FOM.
The arterial supply to the FOM is from the lingual arteries, branches of the external carotid artery, as well as the mylohyoid and submental branches of the facial arteries.
The mylohyoid and hypoglossus muscles provide both structural support to the contents of the FOM and serve as barriers to the submental and submandibular triangles of the neck (FIG 1B).
The sublingual salivary glands, located beneath the mucosa of the anterior FOM, drain via the excretory ducts of Rivinus, which drains into the submandibular duct or directly into the FOM through the plica fimbriata (mucous membranes located on either side of the frenulum).
The anterior FOM lymphatic drainage is to the submental and submandibular nodes, whereas the posterior FOM drains to the upper cervical lymph nodes.
PATHOGENESIS
Floor of mouth squamous cell carcinoma (SCC)
Approximately 18% to 45% of all oral SCCs occur in the FOM, and most originate at the anterior midline.1 As with other locations of oral SCCs, there is a strong association with alcohol consumption and tobacco smoking. There is an increasing incidence of HPV-associated head and neck SCCs in patients without traditional risk factors.
SCC tumors typically spread in a superior or horizontal fashion as the muscular floor of the FOM serves as a barrier to tumor spread. However, these tumors can also invade the submucosa, the intrinsic tongue muscles, and the contralateral space in the FOM.
The location of FOM structures and their association with the tumor affects the presentation of tumor invasion. In certain cases, SCCs may obstruct the ostia of the submandibular duct, which is located along either side of the frenulum resulting in inflammatory changes and ductal dilatation. In contrast, the sublingual glands are more prone to direct invasion due to proximity of the tumor. Invasion of the mandible upstages the tumor.
Cervical lymph node invasion is common at time of diagnosis, and hematogenous spread to distant sites including the liver, bones, and lungs must be ruled out.
Floor of mouth salivary gland tumors and sarcomas
These tumors account for 3% to 5% of all head and neck cancers, most commonly appearing in the sixth and seventh decade of life.
The etiology is multifactorial; however, occupations with an associated increased risk include mining, asbestos exposure, and rubber manufacturing.
The most common of these tumors are adenoid cystic carcinoma and mucoepidermoid carcinoma.
Most patients present with a painless slow-growing mass. Others may manifest with perineural invasion resulting in pain or numbness.
Sarcomas of the oral cavity most often arise from the maxilla or mandible as an osteosarcoma, chondrosarcoma, rhabdomyosarcoma, or liposarcoma. Liposarcomas occur with equal frequency in the mandible and maxilla. Similar to other neoplasms of the oral cavity, surgical resection is the primary modality for treatment.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patient history begins with a thorough assessment of the onset of symptoms, duration, course, and associated risk factors, the most common of which are alcohol consumption and tobacco use.
Symptoms of floor of mouth tumors may include an enlarging or recurrent mass, difficulty with speech, chewing or deglutition, odynophagia, halitosis, and red or white intraoral discoloration.
The physical exam begins with inspection and palpation of both the extraoral and intraoral soft tissues. This includes assessment of the lips, intraoral labial mucosa, buccal mucosa, the dorsal and ventral surface of the tongue, the hard palate, and the FOM.
The sublingual, submandibular, and parotid glands are palpated and examined for any abnormalities.
The neck is inspected for signs of cervical lymphadenopathy as floor of mouth cancers typically metastasize to the cervical chain of lymph nodes. Evaluation of the anterior deep cervical lymph nodes, the preauricular and postauricular lymph nodes, is included in the examination.
IMAGING
Numerous imaging modalities are available for both diagnostic as well as treatment planning and include plain radiographs, magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET).
Plain radiographs or panoramic images are routinely used by dentists and may initially suggest a malignant lesion during an initial evaluation. CT scans, however, are currently the standard for primary tumor detection with a specificity ranging from 81% to 100% and sensitivity of 41% to 82%.
PET scan or PET/CT evaluates tissue metabolic activity and is used to assess for metastatic spread to lymph nodes as well as distant tissues.
SURGICAL MANAGEMENT
Successful reconstruction after oncological extirpation is based on the following principles:
Tumor-free resection margins
Maximizing mobility of the remaining tongue
Watertight closure and seal that protects the neck structures from FOM secretions
Maintaining mandibular continuity
Reconstructive options
FOM defects arise most frequently from composite resections of the mandible and FOM or tongue and FOM. Less frequently, resection of soft tissue tumors or salivary gland cancers leads to isolated FOM defects.
Many options exist for reconstruction of the soft tissue FOM defects. In general, the reconstructive options are dictated by the volume and type of tissue that is resected. Thus, soft tissue low volume defects require replacement with low volume soft tissue flaps. Large-volume composite defects that include soft tissues and bone may require reconstruction with osteocutaneous flaps. Rarely, complex cases may require more than one flap for reconstruction; however, in general, most defects of the FOM can be reconstructed with a single flap.
Microvascular free flaps are the preferred reconstructive options for patients with floor of mouth defects because they have excellent blood supply; can be constructed of thin, pliable tissue; and can be customized to fit any defect.
Soft tissue flaps such as the radial forearm, anterolateral thigh (ALT), medial sural artery perforator flap (MSAP) and pectoralis major musculocutaneous flaps are most commonly used for FOM reconstruction. The selection of reconstructive technique depends on patient factors, the extent and complexity of the surgical resection, and surgeon preference.
Patient factors include thickness of the subcutaneous fat layer in the flap donor sites and blood supply/circulation (eg, intact palmar arch).
Surgical factors include primarily the type and extent of resection. For example, complex defects that include wide resection of the FOM musculature and supporting structures may require a large volume composite flaps that include skin and muscle to obliterate dead space, whereas low-volume defects restricted to the FOM mucosa may be better reconstructed with thin pliable flaps.
Ultimately, the flap that is selected for reconstruction should maximize reconstructive goals of obtaining a watertight closure of the defect and maximize the potential to swallow and speak.
Soft Tissue Flap Options
Radial forearm fasciocutaneous free flap
The radial forearm flap was first described by Yang in 1981 and later popularized by Soutar and McGregor in 1986 for intraoral reconstruction and is a skin and fascial flap based on the radial artery, its venae comitantes, and, often, the cephalic vein.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree