The hand surgeon’s familiarity with options for flexor tendon reconstruction is essential. Efforts at primary repair are not always successful nor are the conditions after injury necessarily conducive to primary coaptation of tendon ends. Single-stage and two-stage grafting, tenolysis, and pulley reconstruction are parts of the reconstructive surgeon’s armamentarium. Future interventions of tissue engineering suggest the possibility of creating a theoretically endless supply of available donor material for use in tendon reconstruction.
Early depictions of flexor tendon repair can be found in the writings of Galen ( ad 129–199), physician to the gladiators. A translation of his records states, “I found one of the gladiators called Horseman with a transverse division of the tendon on the anterior surface of the thigh, the lower part being separated from the upper, and without hesitation I brought them together with suture.” The principles of acute tendon repair have evolved to today’s debates on repair tactics, core strand number, early mobilization techniques, and so forth. Principles of atraumatic technique, a bloodless field, asepsis, and pulley preservation in flexor tendon surgery were highlighted by Bunnell in 1918. Kleinert and Kutz’s 1967 presentation, entitled, “primary repair of flexor tendons in no man’s land,” changed the dynamics of modern tendon repair that is practiced today. Primary repair occasionally fails, however, to provide the desired outcome. Lexer reported on the first series of flexor tendon graft use in the hand in 1912. Basset and Carroll first described secondary reconstruction of tendons in zone II using silicone implants in 1963. Hunter refined this technique in 1971. The best results of tendon surgery often rely on the condition of the tissues, patient comorbidities and commitment to therapy, and the initial surgical technique. Undesirable range of motion (ROM) outcomes may require secondary surgery to resolve the assault of scar tissue on tendon glide or tendon rupture.
Proper patient selection should always remain at the forefront of the hand surgeon’s mind before embarking on the reconstruction to restore functional ROM. Before consent documentation, a candid discussion should be had with the patient regarding the prolonged postoperative rehabilitative efforts required for optimal outcome. Regardless of the elegance or precision of reconstructive efforts, poorly motivated patients will not actualize their potential gains.
Outcomes and expectations should be discussed with patients with specific issues in mind. Patient age, tissues involved in scar, occupational/functional demands, and needs for activity of daily living may alter considerations of aggressive reconstruction. Arthrodesis or amputation may be in a patient’s best interest in many cases.
There are several conditions that limit the normal flexion of fingers after flexor tendon repair and rehabilitation. Adhesions, tendon rupture, joint contracture, or soft tissue constraints limit motion. Poor outcomes after primary tendon repair are often a combination of many of these elements. Hand surgeons should address each of these conditions before surgery. Scar-related limitations of motion mandate an aggressive therapy regimen for at least 3 months before considering procedures, such as tenolysis or joint release. Tenolysis before this may endanger nutritional supply and increase rupture rate. The healing tissues are also in an environment of inflammation. Early surgery in this environment mounts inflammation on more inflammation, often making the second surgery counterproductive. As long as gains are made through physical therapy, secondary surgery should only proceed with caution.
Surgical techniques
Flexor Tenolysis
The indications for flexor tenolysis include limited active ROM with greater passive ROM. Consideration must be given to capsulotomy, collateral ligament release, and checkrein ligament release if passive motion is impaired. In general, the technique involves incising scar tissue between the tendons and the phalanges or surrounding tissue. Although any type of anesthesia can be performed for a tenolysis procedure, the more awake a patient is during the surgery, the more of the true active ROM potential can be realized by both patient and surgeon. By keeping patients within an appropriate state of consciousness (or even without sedation), they can participate actively in the surgery to demonstrate the effectiveness of the adhesiolysis. Patients’ direct observations of intraoperative gains after tenolysis may serve to motivate their postoperative efforts in rehabilitation.
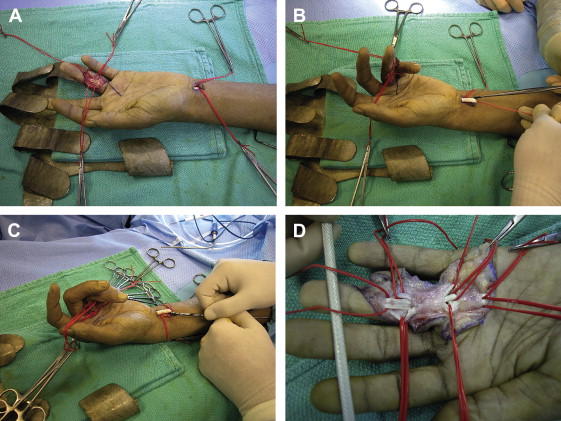
The surgical exposure to the tendons is obtained through either Bruner zigzag incisions or by the midlateral approach supported by Strickland. Midlateral incisions may provide a better bed of tissue to lie across the operative site and reduce wound tension with postoperative digital motion. Adhesiolysis should proceed from the proximal unscarred tissue to the distal scarred areas, identifying and preserving the neurovascular bundles during the process. Although Verdan suggested wide sheath excision during the tenolysis, most surgeons today recommend conservation of as much of the pulley/sheath system as possible. The tenolysis is performed with a small Beaver blade, elevator, fine tissue scissors, or specialized tenolysis instrumentation, such as a Meals tenolysis knife ( Fig. 1 ). The flexor digitorum sublimus (FDS) tendon and the flexor digitorum profundus (FDP) tendons are separated from each other, surrounding annular pulleys, and from the dorsal osseous component of the canal. Surgeons should avoid attenuating the repair site through an overaggressive tenolysis. Strickland advocates the use of a pediatric urethral sound dilator to facilitate annular pulley expansion and tendon passage through the pulley system. Patient participation to actively flex the involved digit ensures adequacy of release. A patient who is under general anesthesia or unable to cooperate with this request can have a proximal incision made in the palm or the wrist to provide access to the proximal tendon. Traction on the proximal tendon confirms the complete release of the distal adhesions. This “traction flexor check,” originally described by Whitaker, illustrates adequate flexion of the digit and signifies complete release of adhesions around the flexor tendons ( Fig. 2 ). An alternative to the traction test is the forearm compression test, where the flexors are compressed in the distal forearm that forces the released or unaffected digits into flexion.

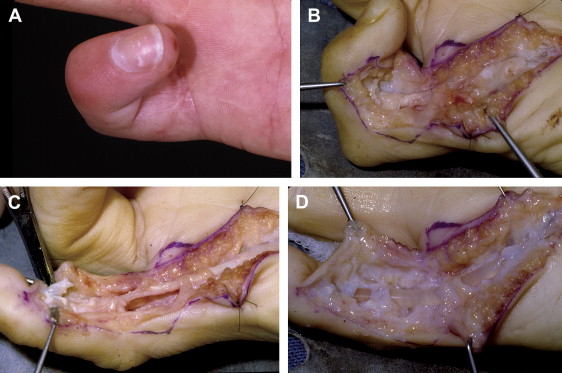
An assessment of the quality of the pulley system and tendon itself should be addressed before skin closure. If greater than 30% of the involved tendon width has been lost or if tendon continuity is only maintained by a segment of scar (gap tissue), the tenolysis may be successful initially but may result in secondary tendon rupture during postoperative therapy. Efforts may be turned to staged reconstruction with a silicone implant if the quality of the tendon is too poor to risk rupture ( Fig. 3 ). The quality of the tendon and pulley system should be conveyed to a therapist to guide the aggressiveness of the postoperative hand therapy.
Although interpositional biologic and artificial inlays have been described for post-tenolysis adhesion reduction, none has achieved reliable results. Various inlays have included cellophane, polyethylene film, silicone sheeting, paratenon, amniotic membrane, gelatin sponge, fascia, vein, and hyaluronic acid derivatives (Seprafilm bioresorbable membrane, Genzyme, Cambridge, Massachusetts). Corticosteroids, intended to reduce the inflammatory phase of healing by local application before wound closure, also are not universally advised because of the risk of tendon rupture and their potential contribution to delayed wound healing.
Postoperative therapy is initiated within the first week and consists of active and passive ROM, edema control, scar message, and strengthening. Therapy continues until the gains in ROM plateau in 2 to 4 months. Surgeons could consider indwelling catheters around the median and/or ulnar nerve in the wrist if pain control in the immediate postoperative period is an issue for patients during therapy.
Joint stiffness may be associated with the tendon adhesions. Patients with joint stiffness have restricted passive motion as well as restricted active motion. Capsulotomies, volar plate release, and collateral ligament release may be required at the time of tenolysis to restore active and passive motion. Unfortunately, the greater the amount of soft tissue release required to achieve motion around the proximal interphalangeal (PIP) or distal interphalangeal (DIP) joints, the worse the outcome. This is likely due to recurrent scarring and periarticular swelling.
Complications of tenolysis surgery are illustrated in Box 1 . All complications can be devastating and may culminate in a functionless digit. Skin loss over the tendon may require flap coverage. Tendon rupture may be a consequence of infection, attenuation of the old repair site, or gap formation at the repair site. Salvage procedures of the ruptured tendon may include tendon grafts if the pulley system was intact, a two-staged silastic rod reconstruction, DIP arthrodesis, tenodesis, or amputation.
- •
Infection
- •
Hematoma
- •
Volar skin necrosis
- •
Tendon exposure
- •
Injury to neurovascular structures
- •
Stiffness
- •
Contracture
- •
Tendon rupture
- •
Bowstringing
Tendon Grafting
The indications for single-stage free tendon grafting are narrow. They include
- 1.
Injuries resulting in segmental tendon loss
- 2.
Delayed presentation greater than 3 weeks, resulting in tendon end fraying or retraction into the muscle belly
- 3.
Delayed presentation of some FDP avulsion injuries.
The pulley system should be intact and supple motion of the digit preserved to proceed with single-stage grafting. Tendon reconstruction in zones III, IV, and V are more amenable to single-stage reconstruction due to lack of a restricted fibro-osseous canal notable in zone II. Although not widely used today, the Boyes preoperative injury classification system for tendon reconstruction provides the principles of current tendon grafting philosophy :
Grade 1—minimum scar, supple joints, no trophic changes
Grade 2—scar-limiting gliding of graft
Grade 3—joint involvement with loss of passive motion
Grade 4—multiple digit involvement with tendon injury
Grade 5—devastating injury with salvage procedures required.
The most desirable preoperative condition for tendon reconstruction is a Boyes grade 1 finger, where joints are without contracture, wounds are well healed, and hand therapy efforts have maximized potential passive gains in ROM. Pulvertaft adds that circulation should be satisfactory and at least one digital nerve intact. Contraindications to grafting include insensate, poorly vascularized fingers; patients who cannot appreciate the needs for strict adherence to postoperative hand therapy regimens (ie, children younger than age 3 years or patients who are mentally debilitated); or those patients who declare that they have minimal functional demands needs (ie, elderly). In more significantly damaged fingers (Boyes grades 2–5), two-stage reconstruction should be pursued. If the intraoperative dissection demonstrates pulley systems in need of significant reconstruction, single-stage reconstruction should be abandoned and efforts turned to two-stage reconstruction. The possibility of a two-staged reconstruction should be shared with patients during the preoperative evaluation.
Common tendon grafts include the palmaris longus tendon, the plantaris tendon, the extensor indicis proprius, the extensor digiti quinti proprius, the FDS tendon to the ring or small finger, and the long toe extensors ( Table 1 ). Tendon grafts can be intrasynovial or extrasynovial. Intrasynovial toe flexor grafts, in theory, replace like with like but the outcomes of any tendon seem similar. The palmaris longus and plantaris tendons are the most frequently used tendon grafts because they are readily available, easy to harvest, and leave minimal donor morbidity. The palmaris longus and plantaris tendons are present in 85% and 80% of subjects, respectively.