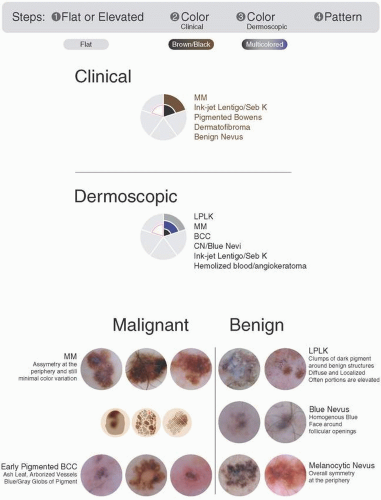
Flat/Brown-Black/Multicolored
Step 1: Is the lesion flat or raised? Flat
Step 2: What color is the lesion on clinical assessment? Brown-Black
Step 3: What is the dermoscopic color? Multicolored
Step 4: Is further elucidation needed to decide whether to biopsy or not? Yes
Is this a malignant or benign pattern?
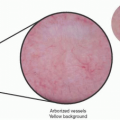
Take a look at the color wheel in Figure 14.1.
We’ve moved into the world of Dark Brown! When we are looking at flat, clinically brownblack, dermoscopically multicolored lesions we are looking at a differential similar to Flat, Brown/Black and Brown, but with a few differences.
Our benign lesions include lichen planus-like keratosis (LPLK) and congenital/junctional nevus.
Our malignancies include superficial malignant melanoma again, but early-pigmented basal cell also makes the list.
Importantly, the majority of dysplastic nevi fall into this category as well. We often struggle to categorize these lesions properly as benign or malignant. While they are not malignant, they should not be treated so simply as benign. Because we are in the world of “flat” lesions, we can recommend short-term monitoring of any dysplastic nevi. However, keep in mind that if the lesion shows any elevation, it must be biopsied. If it is in fact malignant, its elevation would mean that it is already at a more advanced stage and needs immediate removal.
Benign Lesions
Lichen Planus-like Keratosis or Benign Lichenoid
Pearls
Flat/Brown-Black/Multicolored
There are two possibilities for the origin of these lesions:
A solar lentigo undergoing regression or an inflammatory reaction
A seborrheic keratosis undergoing regression or inflammatory reaction
When trying to distinguish between melanoma it is useful to note the following:
LPLKs have more substance/crust on palpation than do superficial spreading MMs.
LPLKs will typically show up on skin types 2 and 3.
LPLKs will generally resemble other lesions on the patient.
Step 4 Pattern Highlights: Review the patterns described in Chapter 1!
The inflammation leads to a nonspecific vascular pattern.
Often, you will see clumps of dark pigment around benign structures:
Diffusely on a background of hypomelanosis
Localized in small clusters
Look for clues of benign features: ridges, sharp borders, moth-eaten borders, fingerprint patterns, milia-like cysts, and comedo-like openings.
These are often the most difficult lesions to differentiate from malignant melanoma and nonmelanoma skin cancers, so we will biopsy these lesions often!
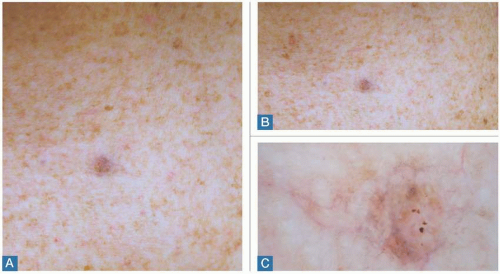
Examples
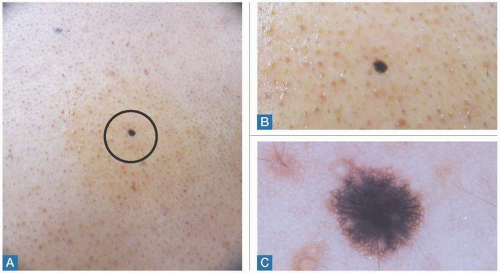
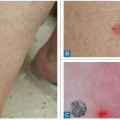
Figure 14.2 shows a clinically flat, brown-black lesion (Figure 14.2A, B), with a dermoscopically multicolored (brown + other = gray, pink, or yellow) pattern (Figure 14.2C). This is an example of an LPLK. We can see a broken reticular pattern and moth-eaten borders, with isolated clumps of gray granularity, which can be difficult to differentiate from melanoma. Remember that flat melanomas will be smooth and not demonstrate the surface changes that we can feel with these lesions, but these can be very difficult to differentiate. This lesion could be classified as either flat or elevated. Diagnosis: Lichen planus-like keratosis.
Bottom line: Biopsy not necessary, but use caution.
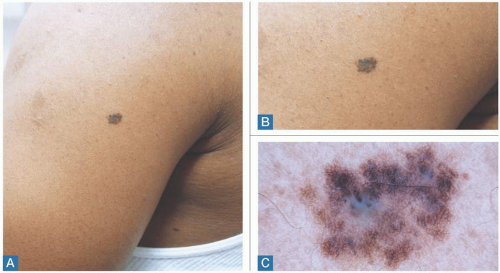
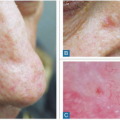
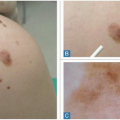
Figure 14.3 shows a clinically flat, brown-black lesion (Figure 14.3A, B), with a dermoscopically multicolored (brown + other = gray, pink, or yellow) pattern (Figure 14.3C). This is an example of an LPLK. We can see a broken reticular pattern and moth-eaten borders, with isolated clumps of gray granularity, which can be difficult to differentiate from melanoma, but you can also appreciate the ridges seen in benign seborrheic keratosis. Remember that flat melanomas will be smooth and not demonstrate the surface changes that we can feel with these lesions. This lesion could be classified as either flat or elevated. Diagnosis: Lichen planus-like keratosis.
Bottom line: Biopsy not necessary, but use caution.
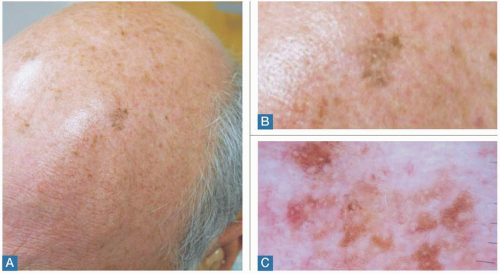
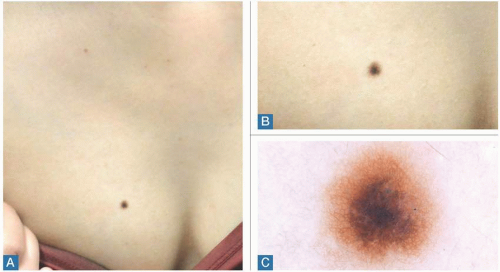
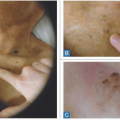
Figure 14.4 shows a clinically flat, brown-black lesion (Figure 14.4A, B), with a dermoscopically multicolored (brown + other = gray, pink, or yellow) pattern (Figure 14.4C). This is an example of an LPLK. We can see a broken reticular pattern and moth-eaten borders, with isolated clumps of gray granularity, which can be difficult to differentiate from melanoma; however, you can also appreciate the ridges and a moth-eaten border seen in benign lentigo. Remember that flat melanomas will be smooth and not demonstrate the surface changes that we can feel with these lesions. This lesion could be classified as either flat or elevated. Diagnosis: Lichen planus-like keratosis.
Bottom line: Biopsy not necessary, but use caution.
Junctional/Combined Nevi
Pearls
Flat/Brown-Black/Multicolored
Clinically, these will have been present since childhood.
If these are a result of iatrogenic causes, such as UV light or rubbing/irritation, the result is multiple colors. You may see shades of brown and sometimes black.
These will resemble other lesions in the area. Patients will have their own “signature” lesion.
Step 4 Pattern Highlights: Review the patterns described in Chapter 1!
Symmetrical reticular pattern with darker dots.
Perifollicular hypopigmentation.
Overall symmetry, especially at the periphery.
Skin types 3 and up will have blue-white veils in benign lesions.
Bottom line: Benign, biopsy not necessary.
Examples
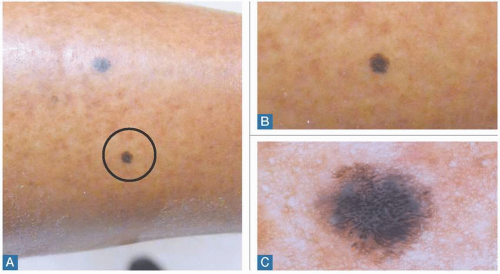
Figure 14.5 shows a clinically flat, brown-black lesion (Figure 14.5A, B) that is dermoscopically multicolored (brown + other = blue/gray, pink, or yellow) (Figure 14.5C). This lesion is characteristic of a congenital nevus that resembles other lesions and has a well-defined border. Dermoscopically, we see a symmetric reticular network pattern with a blue-white veil. Diagnosis: Congenital nevus.
Bottom line: Benign, biopsy unnecessary.
Figure 14.6 shows a clinically flat, brown-black lesion (Figure 14.6A, B) that is dermoscopically multicolored (brown + other = blue/gray, pink, or yellow) (Figure 14.6C). This lesion is characteristic of a congenital nevus that resembles other lesions and has a well-defined border. Dermoscopically, we see a symmetric reticular network pattern with a blue-white veil. Diagnosis: Congenital nevus.
Bottom line: Benign, biopsy unnecessary.
Figure 14.7 shows a clinically flat, brown-black lesion (Figure 14.7A, B) that is dermoscopically multicolored (brown + other = blue/gray, pink, or yellow) (Figure 14.7C). This lesion is
characteristic of a congenital nevus. Dermoscopically, we see a symmetric reticular network pattern with dark dots on the network and an isolated blue-white veil. Diagnosis: Congenital nevus.
characteristic of a congenital nevus. Dermoscopically, we see a symmetric reticular network pattern with dark dots on the network and an isolated blue-white veil. Diagnosis: Congenital nevus.
Bottom line: Benign, biopsy unnecessary.
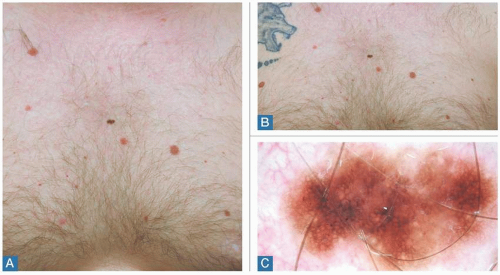
Figure 14.8 shows a clinically flat, brown-black lesion (Figure 14.8A, B) that is dermoscopically multicolored (brown + other = blue/gray, pink, or yellow) (Figure 14.8C). This lesion is
characteristic of a melanocytic nevus. Dermoscopically, we see a symmetric reticular network pattern with dark dots on the network and an isolated blue-gray veil. Diagnosis: Melanocytic nevus.
characteristic of a melanocytic nevus. Dermoscopically, we see a symmetric reticular network pattern with dark dots on the network and an isolated blue-gray veil. Diagnosis: Melanocytic nevus.
Bottom line: Benign, biopsy unnecessary.
Figure 14.9 shows a clinically flat, brown-black lesion (Figure 14.9A, B) that is dermoscopically multicolored (brown + other = blue/gray, pink, or yellow) (Figure 14.9C). This lesion is characteristic of a melanocytic compound nevus. Dermoscopically, we see a symmetric
reticular network pattern. Often lesions that are traumatized or irritated will have multiple colors and can appear malignant.
reticular network pattern. Often lesions that are traumatized or irritated will have multiple colors and can appear malignant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree