63. Female Genital Aesthetic Surgery
Phillip D. Khan, Christine Hamori
■ Incidence of female genital aesthetic surgery has increased as the quest for the aesthetic “ideal” becomes more popular.
• Fivefold increase in the number of patients seeking cosmetic surgery of the vaginal region.1
■ Often, the balance of aesthetic beauty and functional optimization, particularly in terms of sexual intercourse, has played hand in hand.
■ Genital beauty is culturally defined and dependent.2 (Table 63-1)
Table 63-1 Female Genital Aesthetic Surgery Terms and Definitions
| Term | Synonyms/Definition |
| Vulvovaginal plastic surgery | Umbrella term encompassing all procedures defined below |
| Vaginal rejuvenation | Not recommended for use as a proprietary term for medical terminology |
| Labiaplasty/nymphoplasty | Reduction of the labia minora |
| Clitoral hood reduction | Reduction of the clitoral hood |
| Labia majora reduction | Reduction of the labia majora |
| Vaginoplasty | Repair of the vagina to correct vaginal relaxation |
| Perineoplasty | Excision of excess introital and perineal tissue and repair of the perineal musculature |
| Vaginal tightening (colpoperineoplasty) | Both perineoplasty and some degree of posterior vaginal repair for vaginal restoration |
| Hymenoplasty | Repair/reconstruction of the hymen so as to mimic the virginal state |
• In Japan, the “winged butterfly” appearance of the small labia is popular.
• In Western society, protruding inner labia are considered less desirable.
• In part of Africa, in a ritual known as Kudenga, the inner labia are stretched from a young age in the belief it optimizes sexual intercourse.
■ Labiaplasty has become the cornerstone of this multiarea concern
• Aesthetic and functional concerns drive this trend.
• Reasons in Westernized women3:
► Media
► Internet
► Brazilian waxing
► Functional issues like rubbing and hygiene
■ Media influence may increase pressure for women to improve their appearance.4
• Small, hardly visible, symmetrical labia minora have become the norm, with commercial images being altered to reduce the size.4,5
• Growing habit of shaving the genital area, and even the availability of pornography, may influence this ideal image.4
■ A series from Alter6 revealed the following reasons for surgery:
• 85.5% aesthetic reasons, with some discomfort with clothing, exercise, or sexual intercourse
• 13.3% aesthetic reasons alone
• 1.2% medical reasons
■ Ideal aesthetic traits for each segment2,7:
• Labia minora that is symmetrical and does not protrude past the labia majora on standing
• Full labia majora that conceals the labia minora completely with minimal bulkiness in tight clothing
• Inconspicuous clitoral hood
• Mons fat pad that does not protrude in clothing
LABIA MINORA ENLARGEMENT
■ Labia enlargement is classified by measurement (Table 63-2).8
Table 63-2 Felicio Classification of Labia Minora Enlargement
| Type | Measurement (cm) |
| I | <2 |
| II | 2-4 |
| III | 4-6 |
| IV | >6 |
CONDITIONS AND CAUSES
■ Enlargement or hypertrophy in both length and width9–16 (Box 63-1)
Box 63-1 CAUSES OF LABIA MINORA ENLARGEMENT
Congenital
Most common
Acquired
Pregnancy, birth control pills, aging, exogenous hormones7,11
Topical estrogen12
Stretching or weight attachment of the labia13
Dermatitis secondary to urinary incontinence14
Vulvar lymphedema from infections with filarial sanguinous14
Myelodysplastic disease15
Repetitive stretching from pregnancy, sexual intercourse, chronic masturbation16
• Most feel that 5 cm in length, measured from the base of the minora to the labial edge, is the upper limit of normal.4
• Some have suggested that those seeking reduction have a mean labial width of 3.52 ± 0.71 cm8,9
• Felicio classification8 (see Table 63-2)
■ Atrophy or hypoplasia
■ Issues driving correction
• Aesthetic
► Loss of self-esteem/social embarrassment
■ Functional
• Interference with intercourse
• Chronic local irritation
• Hygiene problems
► Almost 50% of patients seeking correction report difficulty performing adequate local hygiene10
• Discomfort during walking, cycling, sitting, wearing more formfitting pants
CLITORIS AND CLITORAL HOOD1,17
NOTE: Clitoral hood conditions may develop either separately or along with labia minora hypertrophy.
■ Excessive, unattractive skin from preputial fold hypertrophy
• Can occur in the horizontal and vertical dimension
• Parallel folds lateral to the clitoral hood
• Drape-like folds that separate the anterior vulvar commissure on standing1
• May protrude to give the appearance of a small penis
• Apparent hypertrophy of hood after aggressive edge trim labiaplasty17
• “Buries” the clitoris
NOTE: This quite often becomes noticeable after a labiaplasty that does not address the clitoral hood concomitantly or after aggressive trimming of the labia minora. Hood redundancy is the most common reason patients seek revision surgery.18
• Phimotic clitoral hood over the clitoris
• Clitoral glans hypertrophy
► Elongation or general size
► Primary or secondary from hormonal changes
► Genetic abnormalities such as disorders of sexual development
► Clitoral hood varies greatly and is commonly asymmetrical.19
♦ Length of 2-6 cm measured from the midline of the anterior labial commissure to the distal clitoral prepuce
♦ Smooth or with multiple folds
♦ May have a parallel fold lateral to the main clitoral hood
♦ Variable thickness depending on the amount of subcutaneous tissue (dartos fascia)
♦ May protrude, if enlarged, to give the appearance of a small penis
LABIA MAJORA
■ Primary hypertrophy2
• Volume excess
• Fatty infiltration of the labia majora and ptosis of the anterior labial commissure20
■ Secondary hypertrophy
• Volume loss, creating excess skin
■ Fat and skin excess
• Creates overhang and droop, often with a central crease from the introitus
• Protuberance
► Creates two concerns:
♦ Overly fatty, full labia majora
♦ Fat deficient, stretched labia majora with skin excess
■ Issues driving correction
• Same as those for labia minora reduction
• Aesthetic concern
• Functional concern
► Discomfort, fitting of clothes, hygiene, secondary sexual dysfunction, chronic irritation
• Weight-related issues are key concerns.
► Weight gain and obesity with resultant fat and skin enlargement
► Secondary to weight loss or time after pregnancy
► Ptosis of mons from massive weight loss, creating majora laxity and skin excess
MONS PUBIS
■ Lipodystrophy
■ Descent of tissue
• Massive weight loss
■ Excess skin
• Massive weight loss
NOTE: Mons hypertrophy or redundancy is seen in both the transverse and vertical dimension.21
KEY POINT: Enlarged mons fat is usually associated with large, protuberant labia majora as a result of fat excess and stretched skin and is rarely eliminated by weight loss.7,20,22
GOALS OF TREATMENT
■ Varies across cultures, particularly in relation to the labia minora
■ Aesthetically desirable result, addressing any functional issues
■ Preserving sensory innervation and physiology is critical.
LABIA MINORA
■ Create an aesthetically pleasing labia minora while addressing functional concerns4,6
■ Reduction of the hypertrophic labia minora
• Thin and straight labia
• Light colored, with optimal color and texture match of the labial edges
• Nonredundant edges
• Symmetry
NOTE: This has been a topic of debate with some feeling that the minora are not perfectly symmetrical, citing a functional advantage of one labia being larger than the other as a sealing mechanism for protection against vaginitis (see below).8
• Preservation of the introitus
• Maintenance of neurovascular supply
• Preservation of sensitivity to the labium and labial edge
► Malinovsky et al23 reported several different groups of nerve endings involved in sexual sensitivity with labial hypertrophy
■ Improve volume of the atrophic or hypoplastic labia minora8
• Aesthetic
• Some point out a functional aspect
► May provide greater comfort for some with sexual intercourse
► May provide more shock absorption as well as aid in tightening of the vaginal space
CLITORIS AND CLITORAL HOOD
■ Reduce excess skin
■ Release entrapment
■ Resuspend to the pubic symphysis
LABIA MAJORA
■ Reduce excess skin redundancy and tissue descent
■ Reduce fat volume
■ Enhance contour
■ Augment atrophy
MONS PUBIS
■ Lift and tighten
• Decrease protuberance of excess fat
• Lift descent
• Contour excess or ptotic skin
• Smooth transition from the lower abdomen to pubic area
■ Correct ptosis of the anterior labial commissure
■ Increase visibility of the genitalia
■ Decrease pressure on urinary bladder and sense of urinary urgency
PERTINENT ANATOMY3,7,24,25 (Fig. 63-1)
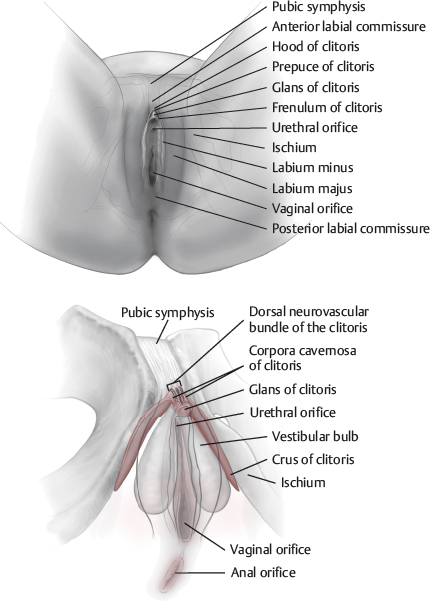
Fig. 63-1 Pertinent anatomy.
CLITORAL REGION
■ Clitoris, prepuce, frenulum, clitoral hood
Clitoris
■ Erectile organ typically 2 cm in length and <1 cm in diameter
■ Attached to the pubic symphysis by the suspensory ligament of the clitoris
■ Consists of a root, body, and glans
• Body
► Composed of two corpora cavernosa and two crura which diverge inferiorly and laterally to attach bilaterally to the ischium
► Corpora cavernosa enclosed within the fibroelastic tunica albuginea
• Glans
► Most highly innervated organ of the area
■ Covered by thinly cornified stratified squamous epithelium devoid of sebaceous, apocrine, or sweat glands
■ The subcutaneous tissue (dartos fascia) of the hood is superficial to the deeper Buck fascia.
■ Dorsal neurovascular bundle travels at the 11 o’clock and 1 o’clock positions at the junction of the glans and body.
• Travels within the deep Buck fascia directly on the tunica albuginea
Prepuce
■ Covers the glans
■ Formed from folds of the labia minora that pass dorsal (anterior) to the glans
Frenulum
■ Extends from ventral (posterior or deeper) glans bilaterally
■ Meets with an extension of the hood to form the labia minora
Clitoral Hood
■ Appearance varies and is frequently asymmetrical19
• Length 2-6 cm
• Smooth or corrugated
• Parallel folds
• Variable thickness
• Protrusive if hood is thickened or clitoris enlarged
LABIA MINORA3
■ Other names include nymphae or labium minus pudenda.
■ Two longitudinal, hairless cutaneous folds
• Varying in size and devoid of fat
• Internally situated between the labia majora
• Paired folds surrounding the vestibule of the vagina
■ Skin is smooth, pigmented, and mildly rugose at the edges.
• The dermis has a comparatively thick connective tissue component.
► Composed mainly of elastic fibers and small blood vessels, making up erectile tissue
• The dermis is similar in thickness to eyelid dermis. This varies patient to patient. Some patients have very thick dermis of the labia minora.16
■ Core of spongy connective tissue
• Contain erectile tissue and many small blood vessels and sensory nerve endings
• Contribute significantly to engorgement and thickening during sexual stimulation
■ Inner surfaces of each labium have numerous sebaceous and eccrine glands, along with sensory nerve endings.
• Pink color of mucus membranes
■ Anteriorly
• Each labium divides into upper (anterior or dorsal) and lower (posterior or ventral) parts
► Upper part passes above the clitoris to meet the contralateral side.
♦ Creates an overhang known as the preputium clitoridis (prepuce)
♦ Often asymmetrical
► Lower part passes below the clitoris to meet the contralateral side, forming the frenulum of the clitoris.
■ Notable sensibility
• Highly innervated for the entire edge, which is notable for sexual response10,26–30
• Genital corpuscles for erogenous sensibility, as well as Pacinian and Meissner corpuscles26,31
LABIA MAJORA25
■ Prominent folds of skin surrounding the pudendal cleft
■ Each contains:
• Loose subcutaneous tissue with smooth muscle
• The termination of the round ligament of the uterus
• Membranous fat, which is continuous with the superficial perineal fascia
■ Externally, covered with pigmented skin (variable), sebaceous glands, crisp pubic hair
■ Internally, pink and hairless
MONS PUBIS
■ Rounded, fatty prominence anterior to the pubic symphysis, pubic tubercle, and superior pubic rami
■ Mass of fatty subcutaneous tissue
• Typically increases at puberty, decreases at menopause
■ Surface continuous with the anterior abdominal wall
VESTIBULE
■ Space between the labia minora containing openings of the urethra, vagina, and ducts of the greater and lesser vestibular glands
■ Urethral orifice is located 2-3 cm posterior to the glans of the clitoris.
■ Bulbs of the vestibule
• Paired masses of elongated erectile tissue (~3 cm in length) along the sides of the vaginal orifice
• Covered by the bulbospongiosus muscles
• Homologous to the bulb of the penis and corpus spongiosum
■ Vestibular glands
• Greater vestibular glands are partially overlapped posteriorly by the vestibular bulbs.
► Open in the vestibule on either side of the vaginal orifice
► Secrete mucus during sexual intercourse
► Open into the spaces between the urethra and vaginal orifice
► Secrete mucus into the vestibule to moisten the labia
■ Superficial perineal muscles
• Superficial transverse perineal
• Ischiocavernosus
► Attaches to the ischial ramus and partly surrounds the crus of the clitoris
► Contraction during arousal creates blood flow to the corpora cavernosa and compression of deep dorsal veins, contributing to clitoral engorgement (erection).26
• Bulbospongiosus
► Arises from perineal body to pass around the vagina
► Inserts into the clitoris
► Covers the bulb of the vestibule and the greater vestibular glands
► Weak constrictor of the vagina when acting together
SENSORY INNERVATION
■ Anterior labial nerves
• Ilioinguinal nerve
• Genital branch of the genitofemoral nerve
• Perineal branch of the posterior cutaneous nerve of the thigh
■ Posterior labial nerves
• Run posterior to anterior toward the mons
• Pudendal nerve
► Perineal branches
► Posterior labial branches
• Terminal branches of the posterior cutaneous nerve of the thigh
■ Autonomic innervation from the pelvic and hypogastric plexus
• Increases vaginal secretion
• Erection of the clitoris
• Engorgement of erectile tissue in the bulbs of the vestibule
■ Malinovsky et al23 demonstrated multiple different groups of sensory nerve endings in hypertrophy of the labia minora involved in sexual sensitivity.
VASCULAR SUPPLY19,32
■ Extensive collaterals
• External superficial pudendal artery branches
► External superficial pudendal artery anastomosis with the posterior labial artery (branch of the internal pudendal artery)
♦ Supplies much of the labia majora
♦ This arch gives rise to multiple arches supplying labia minora
• Internal pudendal artery branches
► Perineal, posterior labial, dorsal clitoral arteries
PREOPERATIVE EVALUATION
■ A thorough discussion regarding patient’s aesthetic and functional goals is essential.
■ Examine in both standing and lithotomy positions.
■ Evaluate area as a unit comprising the mons, pubic area, labia minora and majora, clitoral hood and clitoris, introitus.
NOTE: Patients should use a mirror while pointing out areas of concern in each position. Surgeons can identify areas of resection or proposed lift.
LABIA MINORA6,7
■ Protrusion
• Length (base to most projecting point)
• Length in anteroposterior direction
■ Thickness
■ Symmetry
■ Skin quality
■ Skin color
■ Relationship of the introitus
► High posterior lip
► Opened introitus from previous episiotomy
LABIA MAJORA
■ Excess of loose skin
■ Excess or lack of fat
■ Projection in the anteroposterior direction
■ Anterior labial commissure in relation to the pubic symphysis
• This is a guide point, particularly in procedures with a planned pubic lift
■ Must evaluate alongside mons pubis descent and pubic lipodystrophy
NOTE: Evaluating the labia majora with the legs abducted and adducted is critical. The relationship to the inner thighs is noted here. This helps to prevent possible overresection of the labia majora and secondary tethering of skin, a complication that can lead to vaginal splaying.
CLITORIS AND CLITORAL HOOD
• Evaluate patients while they are in standing and lithotomy position.
• Note protrusion, symmetry, hyperkeratotic or darkened skin, extra folds (horizontal and vertical), clitoral gland size, and degree of clitoral exposure.
• Hood deformities are best noted with patient standing.
MONS PUBIS
■ Mons descent
■ Observe the related enlargement, descent, or protrusion of the labia majora.
• Assess the labia majora with simulated elevation of the pubic fat pad, noting the amount of inferior labial protrusion.
• Examine the majora with the mons lifted.
■ Panniculus
• Determine the amount of pubic skin above the hairline that will need to be excised transversely.
• Simulating a possible lift, note the position of the anterior labial commissure.
► Should be at the pubic symphysis
► Reference point for magnitude of lift and subsequent amount of skin to be excised
NOTE: The skin excision extent may vary with fat removal.
INFORMED CONSENT
■ Postoperative course and complications
■ Labial swelling
• Labia minora and clitoral hood edema
■ Change in position of the anterior labial commissure
■ Inadequate reduction
■ Pain
■ Color change
• Suture line may create a contrast between lighter and darker tissue or between coarse and finer hair.
• Seen in all forms of labia minora and labia majora reduction
■ Reduction of one area of the total complex may result in prominence of other areas.
• Reduction of the labia majora alone may result in more prominence of the labia minora or clitoral hood.
■ Sexual dysfunction
■ Change in position, sensation, or even tethering of the vaginal introitus
■ Exposure of the clitoral glans
■ Vaginal dryness
■ Changes in sexual sensation
■ Scarring—widened, hypertrophic, painful
■ Hematoma
■ Infection
■ Transient dyspareunia
■ Fistula or major wound dehiscence
TECHNIQUES
All techniques are performed with patients in the lithotomy position. Markings are made, and local anesthesia is injected.
LABIA MINORA
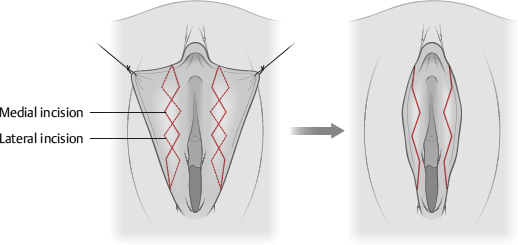
Volume Reduction (Fig. 63-2)
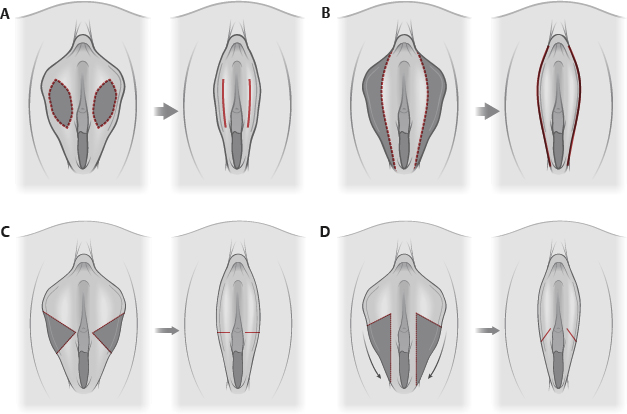
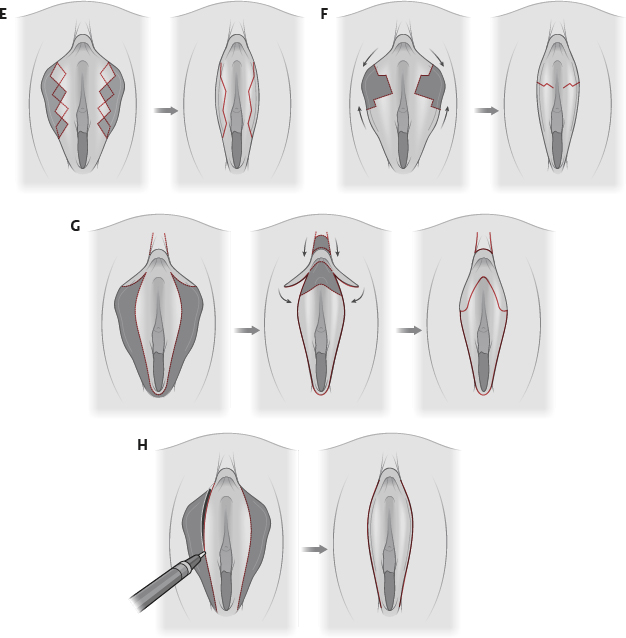
Fig. 63-2 Labiaplasty. A, Deepithelialization; central portion of labial mucosa deepithelialized and reapproximated. B, Direct excision; full-thickness excision using contoured excision parallel to each labia minora, sparing the fourchette. C, Central wedge resection; central wedge of excess tissue excised and labium reapproximated. D, Inferior wedge resection with superior flap; inferior wedge of tissue is resected and labium reapproximated. E, W-plasty excision (zigzag technique); complementary, running, W-shaped resections along medial and lateral aspects of each labium minus, sparing clitoris and fourchette. Interdigitating reapproximation of tissue. F, Z-shaped wedge resection; Z-shaped incisions to excise central wedge of tissue with approximation of each labium minus. G, Composite reduction; curved excision with narrow, superiorly based pedicled flaps and frenulum clitoris preserved. Crescent of tissue below clitoris removed to an extent to which the clitoris will move caudally. Central, rectangular skin segment cranial to the clitoris excised and reapproximated. H, Laser excision; laser used to excise tissue similar to direct excision and wedge resection.
■ Labiaplasty (labia minora reduction)
• Edge trim (most common) 3
• Wedge resection patterns, as originally described by Alter6,18–20 or a variant of such techniques
• Bilateral deepithelialization technique
• Composite reduction33
• Laser excision technique9,34
• Elliptical incisions12,13,17,35,36 (Box 63-2)
Box 63-2 LABIA MINORA REDUCTION TECHNIQUES–ELLIPTICAL EXCISION: PROS AND CONS
| Pros | Cons |
Edge irregularities are reduced. Techniques are powerful for those with extreme hypertrophy.35 Removal of pigmented edge. Debulks thick leading edge of labia minora. | A scarred, stiff suture line subject to tenderness and scar retraction remains. Potential for excess tissue resection, especially if minora retracted laterally during marking and subsequent excision. Some pigmentation may remain depending upon location and amount of labial hypertrophy. The transition zone between the labium, frenulum, and clitoral hood may become distorted, resulting in an abrupt-ending clitoral frenulum and large, noticeable, overhanging clitoral hood. |
► Markings
♦ Traction is placed over the most prominent portion of the labia.
♦ The most anterior portion of the resection is kept to within 1 cm of the clitoral hood and does not include the frenulum.
♦ Posteriorly, the markings are stopped before they cross the midline of the posterior fourchette.
♦ Anteriorly, markings are stopped within 1 cm of the urethral opening to avoid distortion.
► Technique
♦ Full-thickness edge resection of minora
♦ Closure with interrupted or running absorbable suture. Avoid excess tension on suture line to avoid suture track scarring.
• Zigzag technique (Maas and Hage37) (Box 63-3)
Box 63-3 ZIGZAG TECHNIQUE: PROS AND CONS
| Pros | Cons |
Preservation of natural border Elimination of the labia minora edge scar, thus creating a more rounded lateral edge. | Color mismatch or asymmetry. Pigmentation is lost along the labial edge.3 Excess bulk from Z-plasty35 |