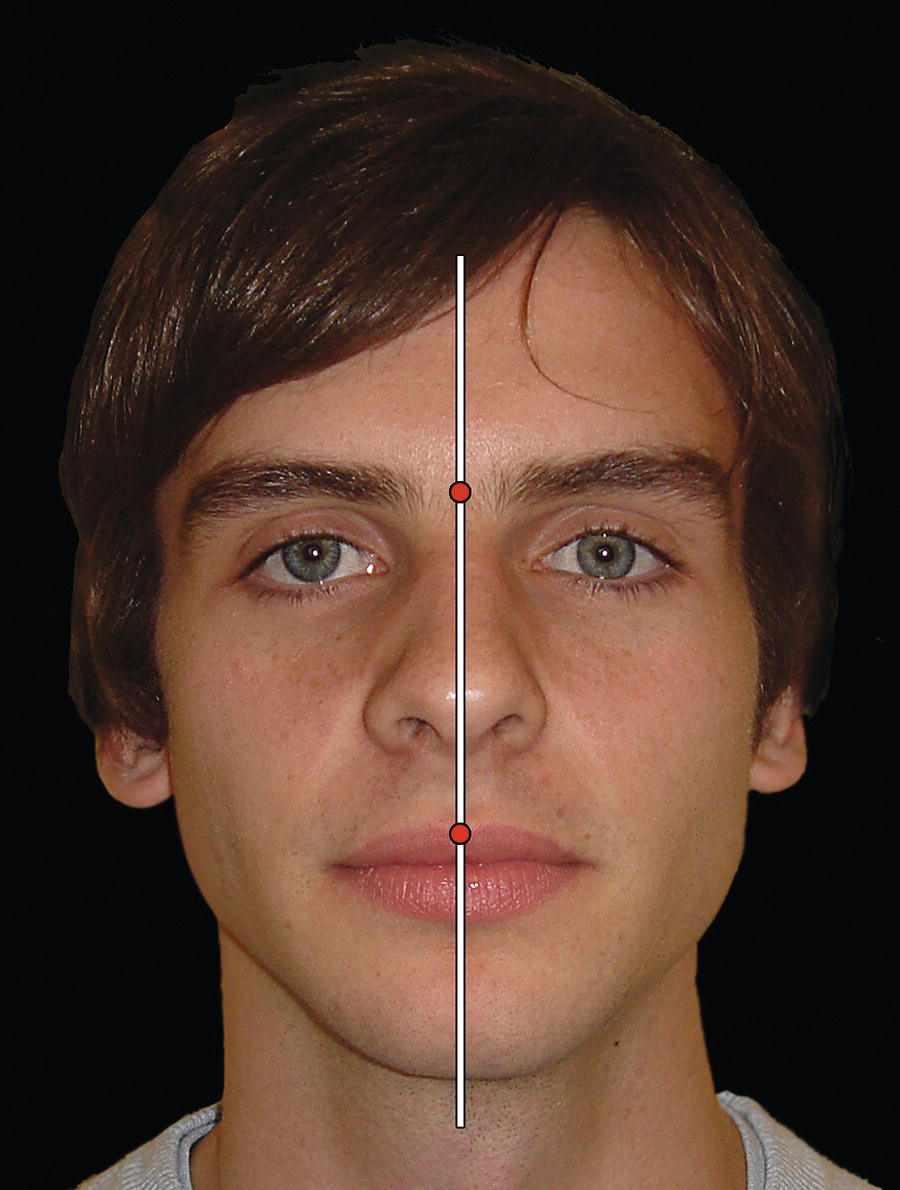
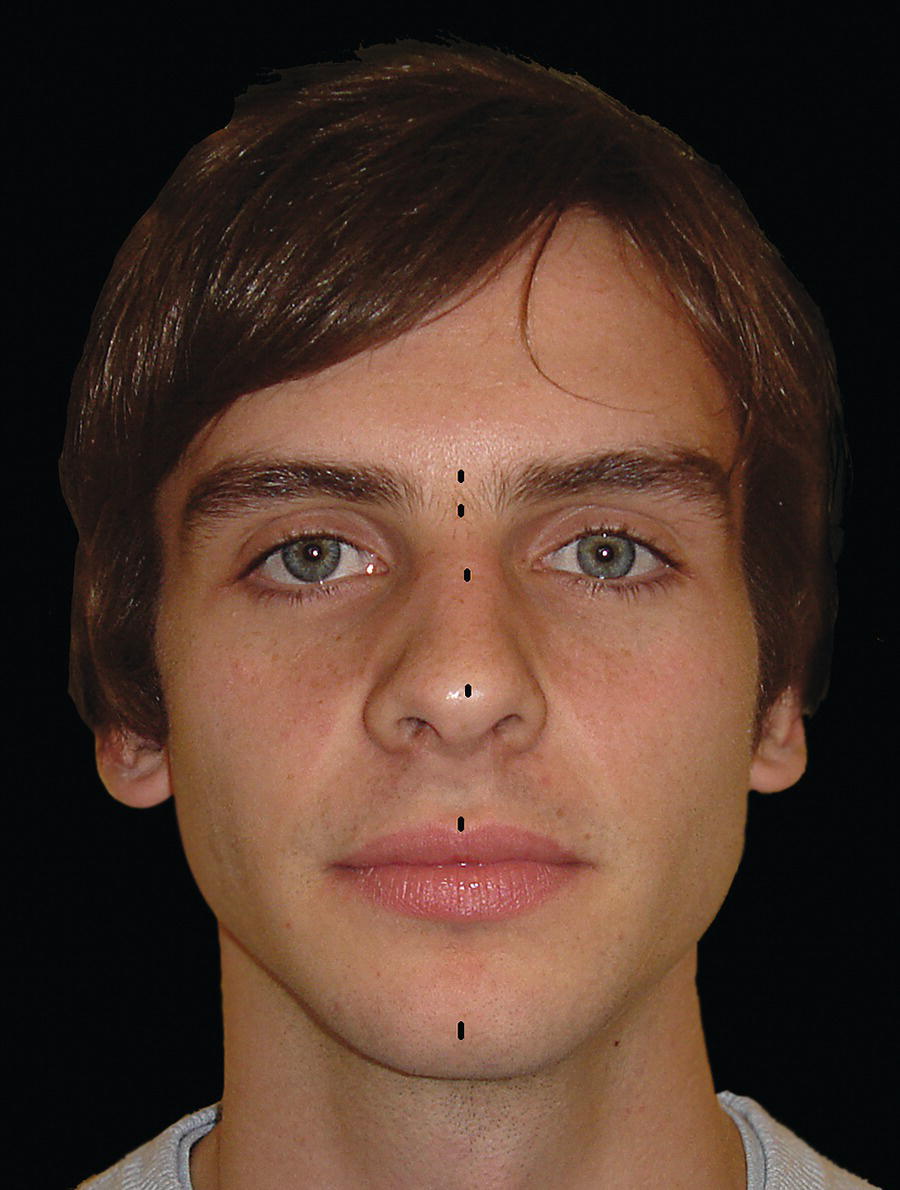
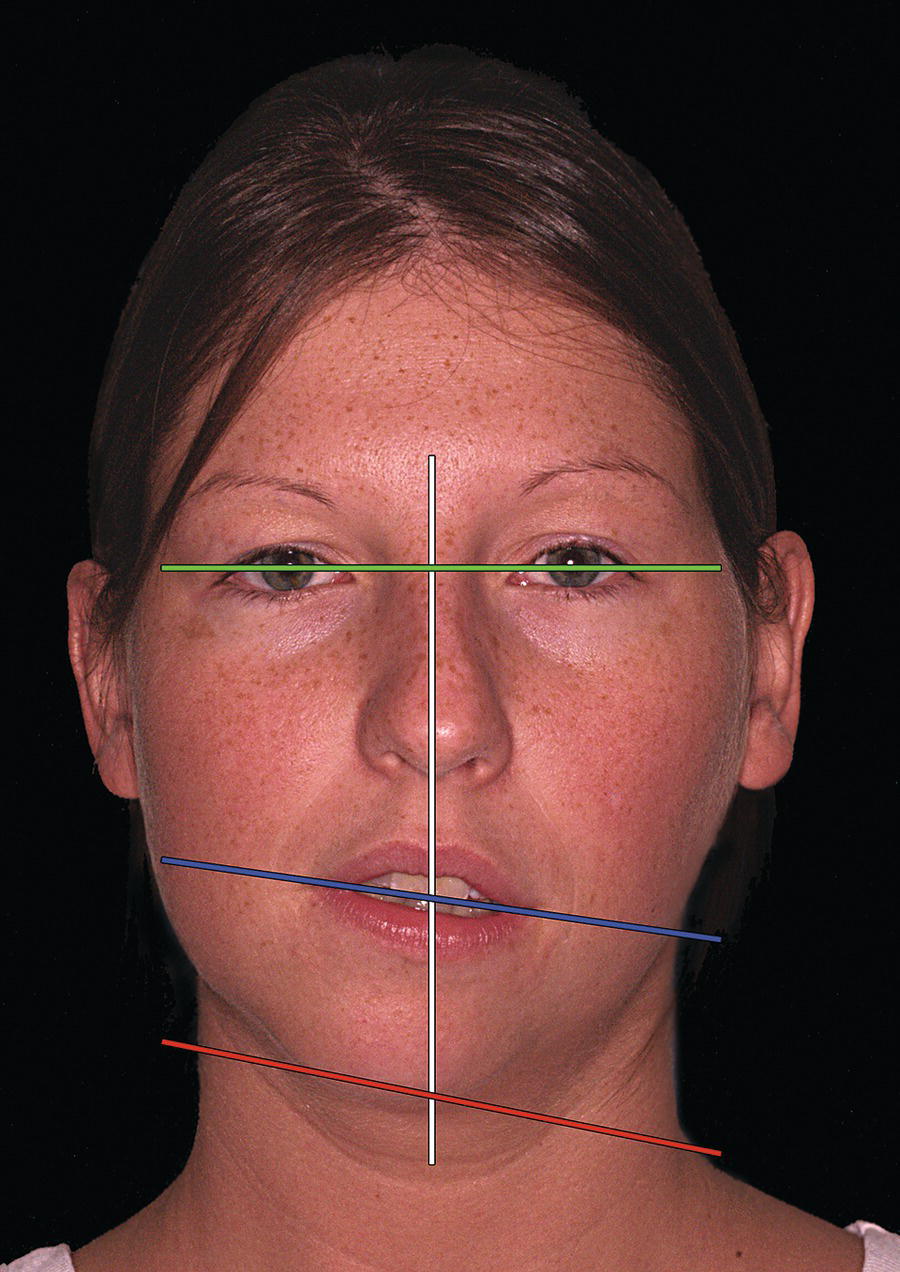
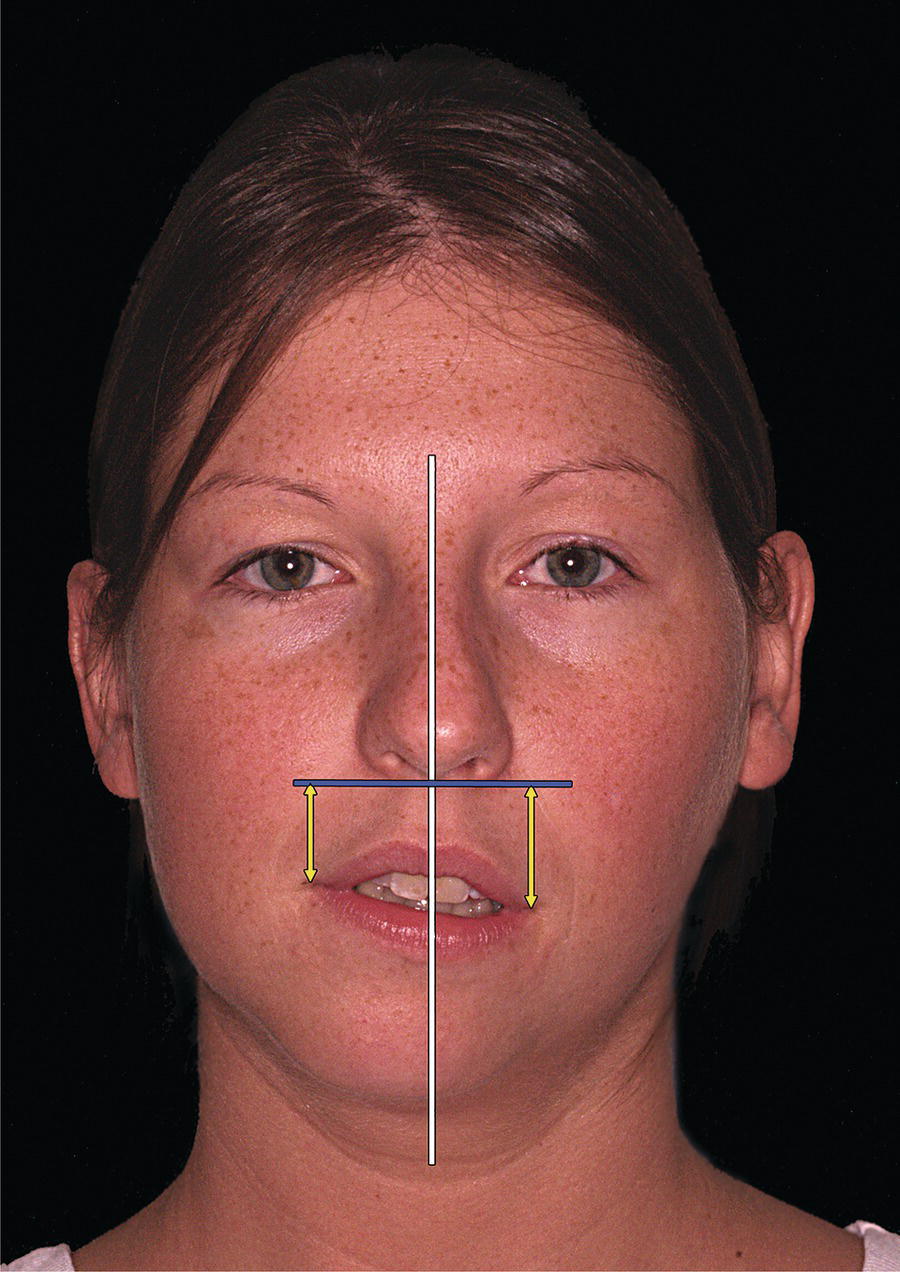
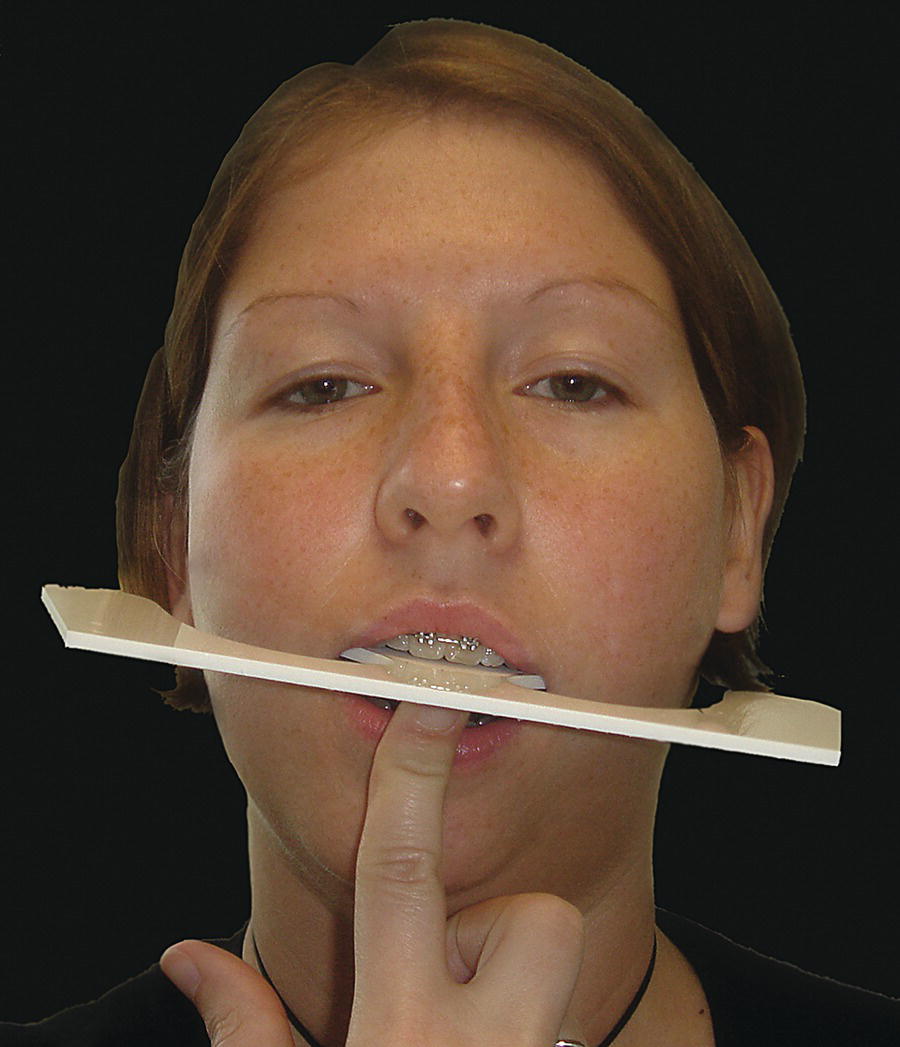
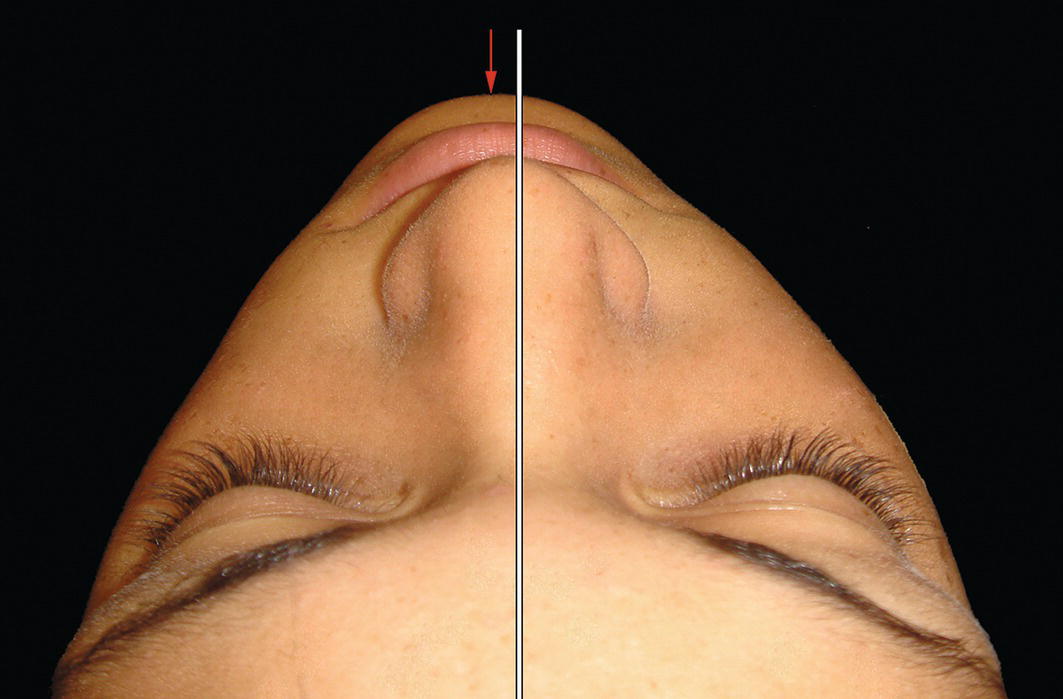
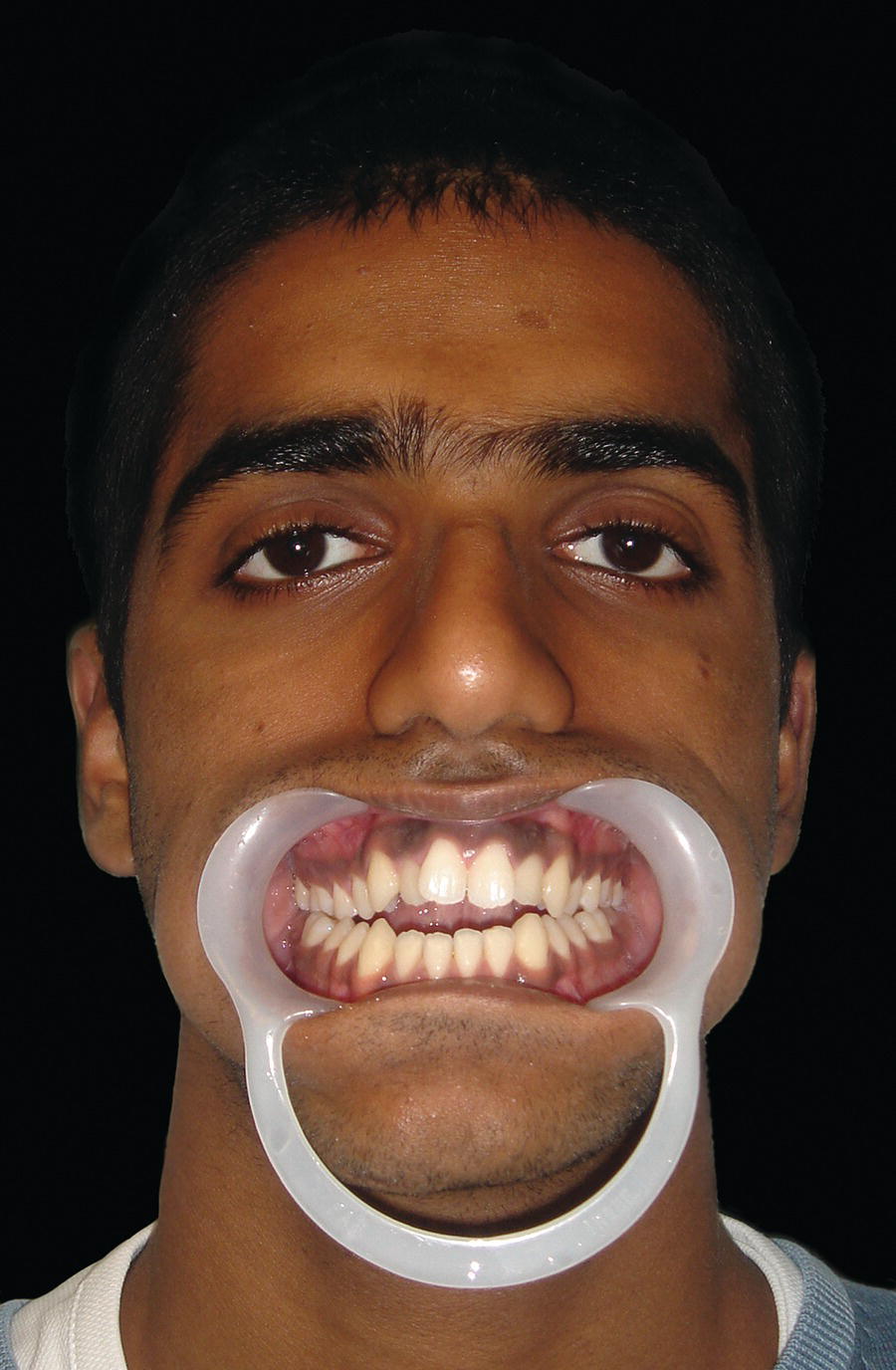
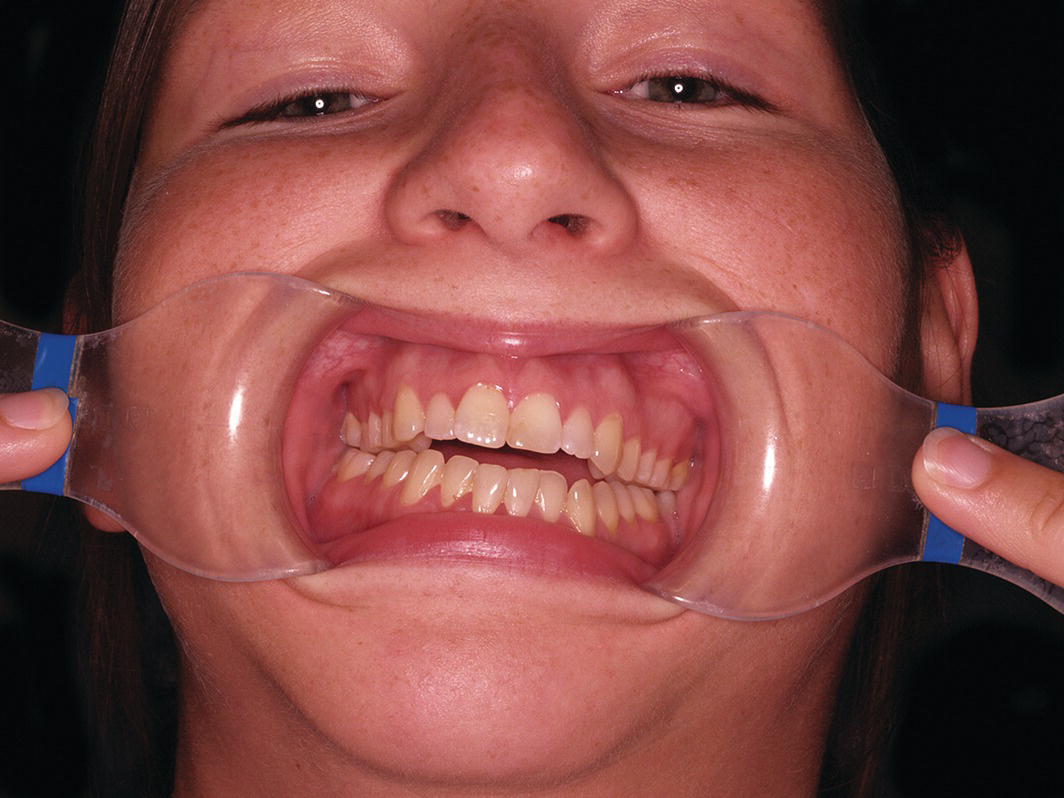
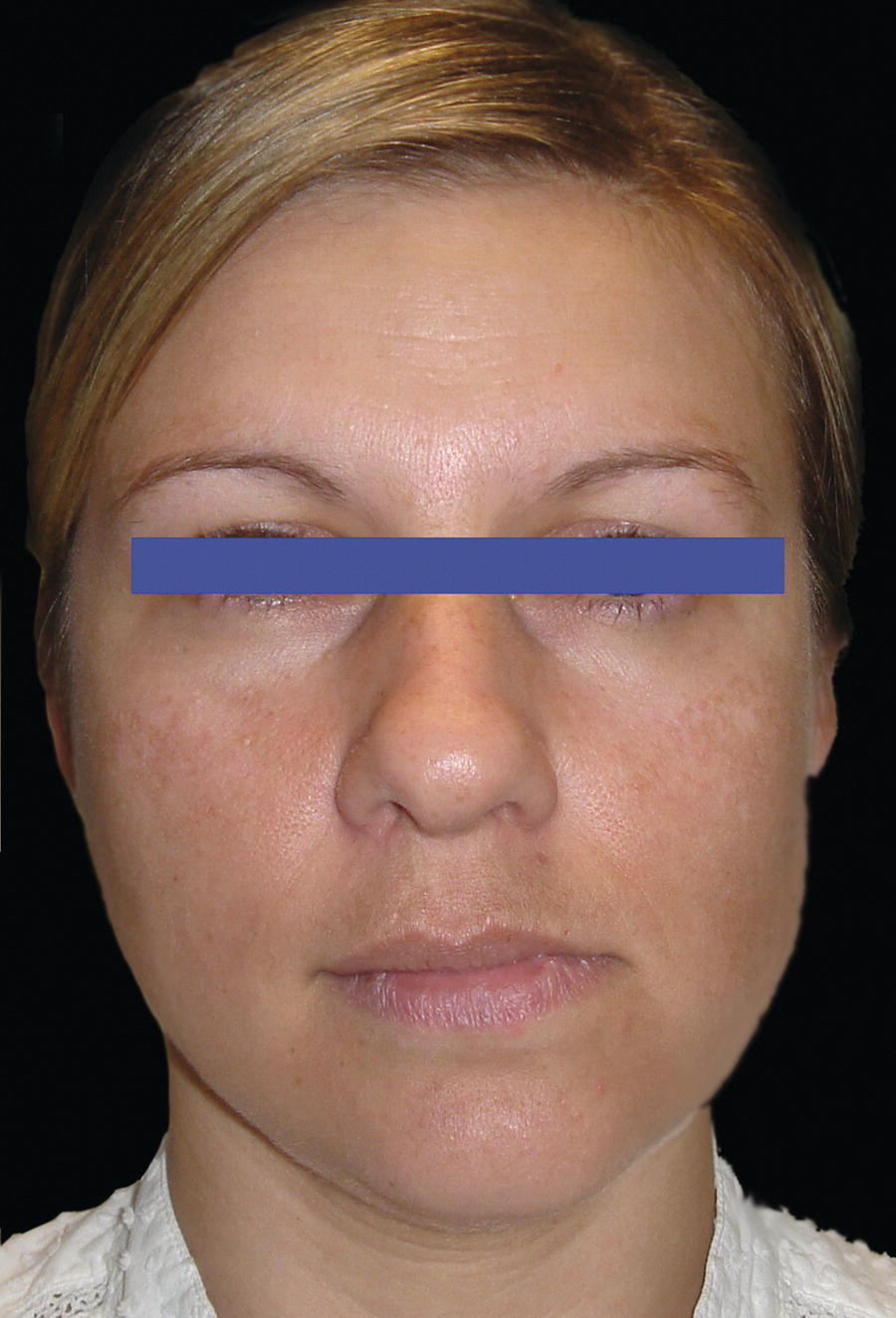
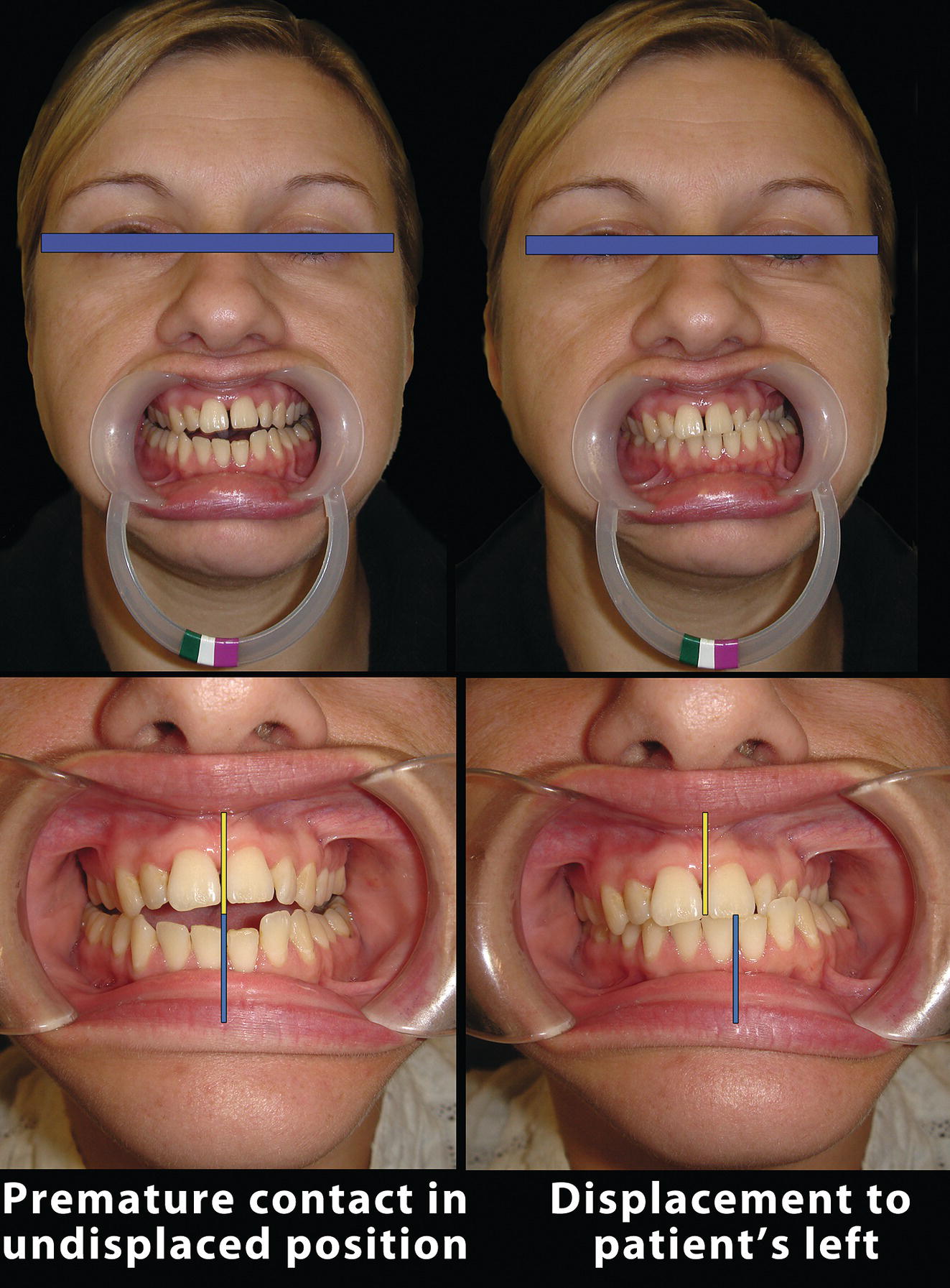
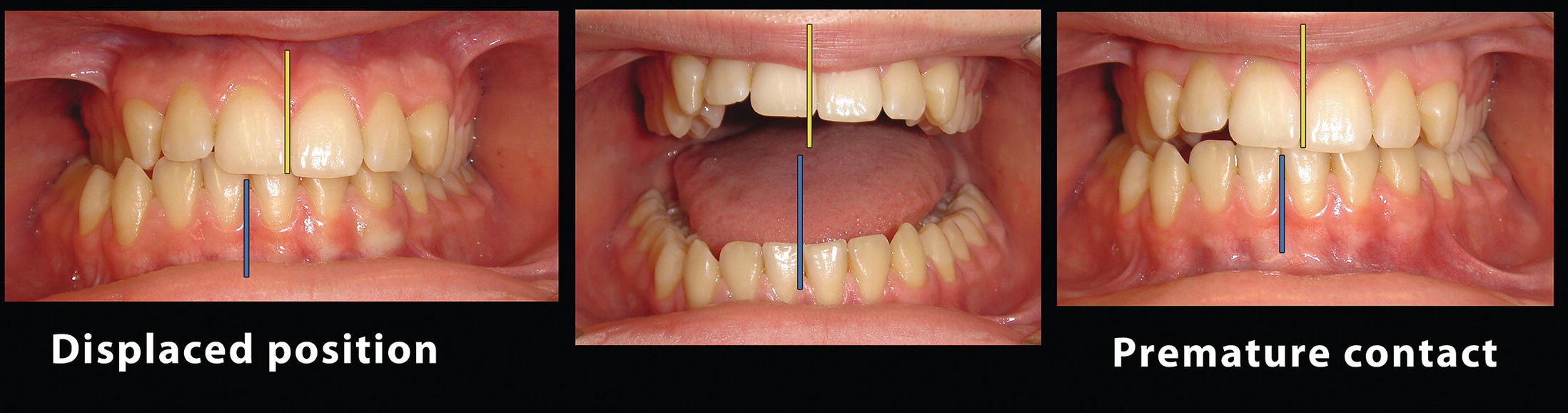
Symmetry may be defined as correspondence in size, shape and relative position of parts on opposite sides of a dividing line or median plane. Asymmetry is defined as a lack or absence of symmetry. The application of this definition to the human face illustrates an imbalance or disproportionality between the right and left sides of the face. No human face exhibits perfect bilateral symmetry. Although a mild degree of asymmetry is normal and acceptable in the average face, greater degrees of asymmetry have been correlated with clinical depression, low self‐esteem and other health problems associated with poor quality of life, such as neurosis and an inferiority complex.1 A number of studies have been published in the psychology literature regarding facial asymmetry and perceptions of attractiveness.2,3 These studies report that facial symmetry is an important factor in facial attractiveness. Perfect bilateral body symmetry seldom exists, and mammals in particular have marked asymmetry in the size, shape and position of the internal organs. Brain function also exhibits asymmetry, a simple example being right and left‐handedness. Craniofacial asymmetry may result from discrepancies in the size, shape or relative position of individual bones in the craniofacial complex and/or the overlying soft tissues. Peck et al.4 evaluated bilateral facial skeletal symmetry in 52 ‘exceptionally well‐balanced’ white Caucasian adults and observed that the degree of asymmetry was greatest in the lower facial third, and that asymmetry reduced as the cranium was approached. Severt and Proffit5 analysed data from patients with dentofacial deformities over an 18‐year period. Of the one‐third that exhibited facial asymmetry, the lower facial third was affected much more frequently than the middle or upper thirds. Only 5% had asymmetry of the upper face, 36% had asymmetry of the mid‐face, mainly just involving the nose, whereas 75% had a deviation of the chin. Facial proportions and facial symmetry are separate yet interrelated entities. In fact, the classical Greek descriptions of symmetry (Greek ‘symmetria’ συμμετρία: a term blending the concept of symmetry with ‘ideal’ proportions) and proportion (Greek ‘analogia’ αναλογία: proportion) are entirely interwoven. In the first century BC, the Roman architect Marcus Vitruvius Pollio wrote the 10‐volume De Architectura (‘On Architecture’). In Book III, Chapter 1, Vitruvius wrote: ‘The design of a temple depends on symmetry, the principles of which must be most carefully observed by the architect. They are due to proportion, in Greek ‘analogia’ (αναλογία). Proportion is a proper agreement between the measures of the parts of an entire work, and the relation between the different parts and the whole general scheme, in accordance with a certain part selected as standard. The principles of symmetry result from proportion. Without symmetry and proportion there can be no principles in the design of any temple. Thus, in the well‐proportioned human body there is a kind of symmetrical harmony … and so it is with perfect buildings.’6 [emphasis added] The principles that Vitruvius described for architecture were based on those described by classical Greek sculptors. These same principles of correct proportions and symmetry are the foundation of diagnosis and treatment planning in the management of craniofacial deformities. ‘It is a safe rule to apply that, when a mathematical or philosophical author writes with a misty profundity, he is talking nonsense.’ Alfred North Whitehead (1861–1947), English mathematician and philosopher, An Introduction to Mathematics (1911)7 The terms balance and harmony are often used by clinicians when describing facial aesthetics. Left–right balance of the face refers to symmetrical relationships, whereas balance between the vertical facial thirds refers to proportional relationships. The term harmonious proportions again refers to ideal proportional relationships, whereas a harmonious facial profile often simply means a profile that is pleasing to the eye. Both these terms are non‐specific and in the clinical setting may serve to confuse. The terms balance and harmony should ideally only be employed when the particular aspect being described is clearly specified; otherwise it is better to employ accurate and quantifiable terms, such as symmetry and proportion, when describing craniofacial morphology. Facial asymmetry may be caused by a range of factors that affect the underlying facial skeleton and/or its overlying soft tissues. Patients with a significant, true skeletal and/or soft tissue facial asymmetry may have a developmental condition, or a growth anomaly resulting from trauma. A complete patient history and medical history, in‐depth clinical and radiographic assessment and an evaluation of the developmental status in children will usually permit the development of a differential, if not definitive, diagnosis. Patients with congenital craniofacial syndromes are often relatively easy to recognize from the physical appearance, e.g. hemifacial microsomia, craniosynostoses (Crouzon and Apert syndrome) and Treacher Collins syndrome. A number of methods have been described to classify the numerous conditions resulting in facial asymmetry. Any attempt to bring order to such a group of disparate conditions is helpful, even if the various classifications crosscut each other.8,9 A useful classification system involves broadly separating the causes of facial asymmetry into three groups: congenital, developmental and acquired (Table 10.1).8,9 Congenital anomalies are conditions acquired during prenatal development, which are usually observed at birth, and may be further subdivided into malformations, deformations and disruptions. Developmental anomalies are conditions arising during postnatal growth through adulthood. For example: Acquired anomalies are conditions arising from either trauma or pathology. Examples of pathological conditions include condylar resorption due to: Table 10.1 A classification of the aetiology of facial asymmetry When evaluating the craniofacial structures for asymmetry, the purpose of the clinical examination is threefold: Having undertaken a thorough clinical examination, the third step is: As with all systematic clinical facial evaluation, an overall qualitative (visual, anthroposcopic) assessment is followed by a comprehensive quantitative (anthropometric and cephalometric) analysis. Having obtained the necessary data, a further qualitative assessment is carried out, to determine whether the results of the quantitative assessment corroborates the qualitative evaluation (i.e. look at the patient, then measure the face, and then look at the patient again). The clinical evaluation should begin with the frontal facial examination. The face must be examined for bilateral symmetry with the patient in natural head position (NHP), bearing in mind that a small degree of asymmetry is present in most individuals and essentially normal. The clinician may need to make minor manual adjustments to the patient’s head position, as patients may have developed a compensatory head posture to minimize the aesthetic impact of their facial asymmetry, often tilting their heads to the right or the left, around the sagittal axis (Figure 10.1). Figure 10.1 This patient developed a compensatory head posture, rotating his head around the sagittal axis. With the patient in NHP, a true horizontal line may be drawn through the mid‐glabellar region (soft tissue glabella), midway between the eyebrows, perpendicular to a true vertical, e.g. a plumb line from the ceiling. From this true horizontal line, a perpendicular facial midline (midsagittal plane) may be constructed from glabella (Figure 10.2). Figure 10.2 Facial midline, parallel to a true vertical line (TrV). In less severe dentofacial deformities, the mid‐philtrum of the upper lip (midpoint of Cupid’s bow) will commonly be in the midline of the face, except in exceptional circumstances, e.g. cleft lip or severe nasal asymmetry distorting the upper lip. A line joining this point to soft tissue glabella forms the facial midline. In the symmetrical face, this line will extend to the midpoint of the chin (soft tissue pogonion). The midpoint of the nasal bridge and the nasal tip (pronasale) should be on this line if the nose is symmetrical (Figure 10.3). With the lips slightly separated, the maxillary and mandibular dental midlines may be assessed in relation to the facial midline, in particular to the mid‐philtrum of the upper lip (midpoint of Cupid’s bow). Having obtained the patient’s permission, these points may be marked on the patient’s face with a skin pencil, in order to permit more accurate assessment (Figure 10.4). Figure 10.3 Facial midline, connecting glabella and the mid‐philtrum of the upper lip (midpoint of Cupid’s bow). Figure 10.4 The midpoints of different structures may be marked on the patient’s face with a skin pencil. Figure 10.5 Vertical references lines. Having established the facial midline, further vertical lines may be drawn parallel to the facial midline through any pair of bilateral landmarks suspected of being asymmetrical. It is then possible to assess: Horizontal reference lines may be constructed by connecting bilateral landmarks. It is then possible to assess: Figure 10.6 Horizontal reference lines. Figure 10.7 The vertical level of bilateral structures to a baseline horizontal reference line may be used to evaluate bilateral facial symmetrical relationships. The presence of a cant in the transverse occlusal plane may be observed in relation to the interpupillary line (or a true horizontal plane) with the patient biting on a wooden spatula (or holding it against the maxillary teeth if there is a lateral open bite), both in the incisor/canine region and the premolar/molar region (Figure 10.8), or a Fox’s occlusal guide plane (Figure 10.9). In the absence of a transverse maxillary cant and/or vertical orbital dystopia, the transverse occlusal plane should be parallel to the interpupillary plane. Figure 10.8 Use of wooden spatula to evaluate the orientation of the transverse maxillary occlusal plane. Figure 10.9 Use of Fox’s occlusal guide plane to evaluate the orientation of the transverse maxillary occlusal plane. Following the frontal facial clinical examination, the asymmetrical face may be evaluated clinically and photographically from a number of different views. Figure 10.10 The superior view. The superior (bird’s eye) view is taken directly from above and behind, with the patient’s head hyperextended. This view is useful for assessment of the symmetry of the nasal bridge, and the horizontal projection of the forehead, orbits and particularly the zygomas and paranasal areas. The submental (worm’s eye) view is taken directly from below, with the patient’s head hyperextended. This view is required to assess the symmetry of the mandibular body and the base of the nose, and is also useful for assessing any asymmetrical projection of the forehead, orbits, zygomas and paranasal areas. Figure 10.11 The submental view. The left and right profile views may be used to compare the contour of the left and right sides of the face. This view is particularly useful for assessment of asymmetry in the contour of the inferior border of the mandible. These views are taken with the patient in NHP, and are useful for assessment of asymmetry of the nose, zygomas, paranasal areas and the mandibular ramus and body outline, including the gonial angle. This view is ideally taken with the patient in NHP. An orthodontic cheek retractor may be placed in order to retract the lips and cheeks (Figure 10.12); alternatively, an assistant may stand behind the patient and retract the cheeks using photographic retractors (Figure 10.13). A transverse cant of the maxillary occlusal plane may be assessed in relation to a true horizontal plane or to the interpupillary plane in the absence of vertical orbital dystopia. Figure 10.12 Transverse occlusal plane view with an orthodontic cheek retractor in position. Figure 10.13 Transverse occlusal plane view with photographic retractors. The basic position of the mandible in relation to the rest of the facial skeleton is referred to as the rest position. The muscles acting on the mandible are in a relaxed state and the condyles are in retruded, unstrained positions within the glenoid fossae. This overall position is also referred to as centric relation. In the rest position, the teeth are out of contact by 2–3 mm, referred to as the freeway space. When the teeth occlude into maximum intercuspation, the mandible should also be in a position of centric relation. Ideally, the path of closure of the mandible from the rest position to the position of maximum intercuspation of the teeth should be a simple hinge movement over the 2–3 mm of the freeway space, with the condyles rotating in their glenoid fossae. Occasionally as the path of closure starts from the rest position, there is an initial, premature contact of the upper and lower teeth. This is uncomfortable for the patient, necessitating a displacement of the mandible to obtain maximum intercuspation of the teeth. If this displacement or functional shift of the mandible is in a lateral direction, then the patient may exhibit an apparent or pseudo‐ mandibular asymmetry (Figures 10.14 and 10.15). Figure 10.14 Mandibular asymmetry due to a lateral mandibular displacement to the patient’s left. Figure 10.15 Premature contact in the undisplaced position, from which the symmetrical mandible is displaced to the left when the patient attempts to achieve maximum intercuspation of the teeth, creating an apparent mandibular asymmetry (i.e. a pseudo‐asymmetry). It is important to evaluate the mandible on opening and closing, in order to check for displacements/functional shifts. Assess the patient from in front, and then stand above and behind the patient as they open and close the mouth, in order to assess any lateral mandibular movement on opening and/or closing. If a lateral mandibular displacement is present, the asymmetry should reduce as the patient opens the mouth, with the upper and lower dental midlines becoming better aligned (Figure 10.16). With longstanding mandibular displacements, the pattern of muscular activity is sometimes such that the displacement cannot be identified by observation alone. Therefore, if no displacement is observed, it is important to double check by clinically manipulating the mandible into occlusion. After explaining to the patient what you are going to do, place the knuckle of your curled index finger under the patient’s chin and your thumb on the mental eminence. Ask the patient to relax, to open their mouth and roll the tip of their tongue towards the back of their throat, then apply gentle pressure to move the mandible up and down, aiming to keep the condyles in their retruded position within the glenoid fossae. Look for the initial, premature dental contact; the patient may be better able to identify this area and point it out to you. Having established the premature contact, ask the patient to bite together and the displacement will become evident. It is absolutely vital to check for mandibular displacements in cases of mandibular asymmetry, as missing a lateral mandible displacement may lead to the incorrect diagnosis of a true (i.e. skeletal) mandibular asymmetry and inevitably to incorrect treatment. It is also important to bear in mind that a patient may present with a combined true mandibular asymmetry and a lateral mandibular displacement (Figure 10.17). The degree of true mandibular asymmetry must always be determined from the undisplaced position. Figure 10.16 On mouth opening the upper and lower dental midlines are almost coincident. Figure 10.17 Mandibular asymmetry is evident in the undisplaced position, but is exaggerated by a mandibular displacement to the same side. Some asymmetry in facial animation is relatively common. It is important not to mistake an asymmetry in facial animation with a dentoskeletal asymmetry, e.g. an asymmetrical smile where the levator muscles of one side cause greater elevation of the upper lip than the contralateral side may be mistaken for a transverse cant in the maxillary occlusal plane (see Chapter 23).
Chapter 10
Facial Symmetry and Asymmetry
Introduction
Relationship between symmetry and proportion
Balance and harmony: a note on terminology
Aetiology and classification of facial asymmetry
Aetiology
Classification
Aetiology
Examples
Congenital (prenatal)
Malformations
Cleft lip and palate (unilateral)
Hemifacial microsomia
Hemifacial hyperplasia
Plagiocephaly
Deformations
Mandibular deformation resulting from sharp lateral flexion of the head with the shoulder pressed against the mandible in late intrauterine growth9
Disruptions
Rare facial clefting
Developmental (postnatal)
Intrinsic jaw growth anomalies
Hemimandibular elongation
Hemimandibular hyperplasia
Unilateral condylar hyperplasia
Secondary jaw growth anomalies
Hemifacial atrophy (Parry‐Romberg syndrome)
Sternocleidomastoid torticollis
Duchenne muscular dystrophy
Cerebral palsy
Functional
Lateral mandibular displacement
Acquired
Traumatic
Condylar trauma
Maxillary/facial trauma
Pathological
Condylar resorption
Idiopathic
Juvenile rheumatoid arthritis
Adult‐onset rheumatoid arthritis
Infection/inflammation
Cysts
Tumours
Clinical evaluation
Purpose of the clinical evaluation
Frontal facial examination
Bilateral symmetry

Facial midline (midsagittal plane)


Vertical reference lines/planes (Figure 10.5)
Horizontal (transverse) reference lines/planes (Figure 10.6)

Superior view (Figure 10.10)
Submental view (Figure 10.11)

Lateral view
Oblique lateral (three‐quarter) view
Transverse occlusal plane view
Dynamic clinical evaluation
Mandibular lateral displacement

Asymmetrical facial animation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








