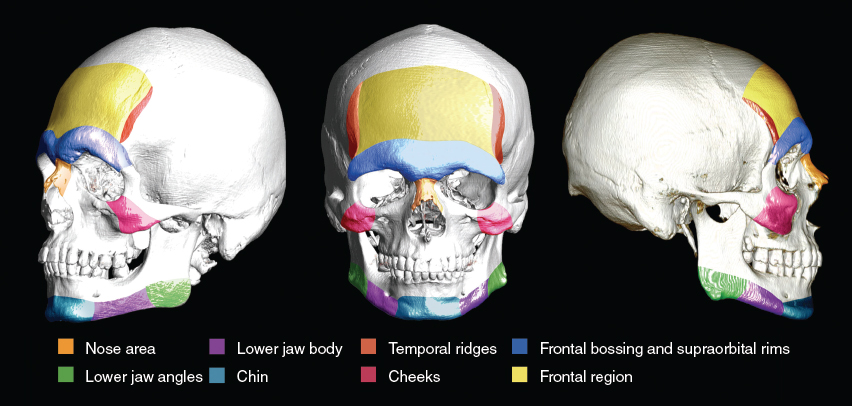
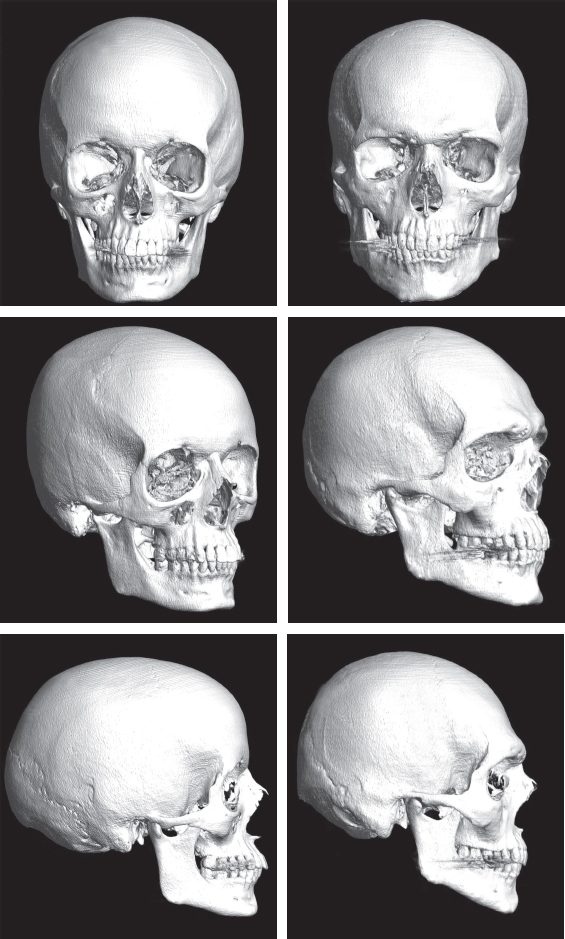
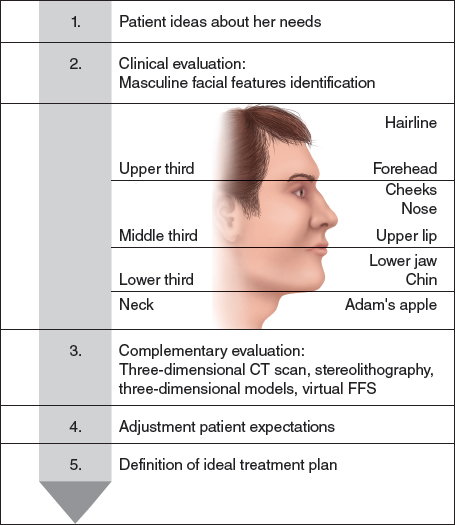
CHAPTER 1 The best way to begin this chapter on facial feminization surgery (FFS) is to pose the following question: Is the face important when it comes to recognizing a person’s gender? Indeed, modifying facial gender in the transition protocol is undoubtedly as important as hormone therapy and genital reconstruction. Feminizing what are visually identified as masculine facial traits raises the self-esteem and confidence of patients, leading to greater acceptance in their personal and family circles, better adaptation in the workplace, and a dramatic decline in social rejection, which unfortunately a large number of transgender patients continue to experience to this day.1,2 From a technical point of view, FFS can be defined as the set of surgical procedures associated with different surgical specialties (oral and maxillofacial surgery, craniofacial surgery, and plastic and reconstructive surgery) designed to soften and modify facial features perceived as masculine, exaggerated, or nonharmonic and therefore decisive in the visual identification of facial gender.3 These features are defined by different craniofacial skeletal structures. In general, the three basic pillars of craniofacial gender are the frontonasal-orbital complex, the nose, and the jaw and chin complex. However, other structural elements, including the cheeks or the trachea, are also important when addressing a patient’s feminization needs and will be discussed in this chapter. FFS is not cosmetic surgery and should not be mistaken as such. However, it does overlap to some degree, and that can cause a great deal of confusion for patients. Facial feminization is based on bone surgery and the readjustment of the overlying soft tissues over the modified bone structure. In some patients, especially older ones, the soft tissue may be too slack to readapt fully to changes in the jaw and chin area. In these patients surgical adjustment (lifting) of the soft tissues may be required. This kind of adjustment should not be undertaken at the same time as jaw and chin surgery but should be done several months later, when the swelling from the jaw and chin surgery has subsided. The purpose of FFS is to treat gender dysphoria, helping the patient feel more comfortable in her own body, but also helping her to be perceived by others as the woman she is. Facial gender modification surgery that is accurate, predictable, and established by protocol must begin with an exhaustive functional, anatomic, aesthetic, and surgical understanding of the craniofacial skeleton. The effect of testosterone and its derivatives, particularly during puberty, conditions the appearance of facial features related to gender identity,4 which can be divided into primary and secondary aspects. Primary aspects—those features determined by the development of the craniofacial skeleton—differentiate the masculine and feminine craniofacial structure in significant ways.5 Generally speaking, the male facial skeleton has greater bone volume and some well-defined features that distinguish it from its female counterpart. These differentiating features appear in the frontonasal-orbital complex, nose, malar region, jaw and chin complex, dentition, and thyroid cartilage (Fig. 1-1). Fig. 1-1 Male skull in three positions, color coded to designate the different areas responsible for facial gender identification. The frontonasal-orbital complex is quite possibly the greatest determinant of facial gender.3,6–9 This region encompasses the forehead, supraorbital ridge, eye sockets, frontal bossing, frontomalar region, temporal ridges, and frontonasal transition. It determines the position of the eyebrows and the positioning of the periorbital soft tissues, such as the eyelids. Typically, all of these areas are more pronounced and have greater bone volume in the male skeleton than in the female skeleton. From the perspective of gender difference, the male nose is generally larger than the female nose because of the increased volume of bone and cartilage. These differences are most visible at the nasal dorsum and tip of the nose. The cheek area (zygomaticomalar region of the facial skeleton) usually has some structural differences that must be defined, because it can readily lead to confusion with regard to facial feminization. As a general rule, malar bone volume is greater in men, which can result in well-defined cheeks. However, prominent, round cheeks in the middle third of the face are compatible with femininity because woman have a greater concentration of fat in this area (that is, the greater volume is not from the bone but from the soft tissues). This has specific implications when it comes to deciding the best treatment for this region. Along with the frontonasal-orbital region and the nose, the complex formed by the jaw and chin constitutes the third pillar of craniofacial gender features. The male jaw has a series of characteristics that can influence the perception of facial gender. To better understand the jaw, we need to consider it divided into the mandibular angle area and the mandibular body. The mandibular angle area is usually squarer, with well-defined corners. The mandibular body typically has greater bone volume, which produces a wider lower facial third in men than in women. It also gives the male jaw its greater vertical height, an important factor when planning mandibular reshaping techniques in FFS. The chin tends to be squarer in men, with more pronounced and defined transitions between the chin and mandibular body, with greater bone volume and a more significant vertical dimension. Gender does not necessarily determine the position of the chin; for instance, retropositioned or overprojected chins can be found in both men and women. However, a well-defined and projected chin may improve the overall aesthetics of the jawchin region. Despite the differences in male and female dentition, which are primarily associated with the format and size of the teeth, at this time this is not a standard line of treatment in FFS. Although some teams have worked with teeth to increase the perception of femininity, few protocols have been established in this area. On its own, this feature is one of the most prominent hallmarks of male gender and a true source of stigma for a large number of transgender women. The tracheal structure, which plays a key role in such basic life processes as breathing and phonation, has a greater volume and is greater in diameter and longer in men. The tracheal structure itself should never be approached with the idea of feminizing it, because this poses the unacceptable and unnecessary risk of damaging the vocal cords or even causing respiratory problems. Only the most prominent part of the thyroid cartilage should be modified. This allows a significant reduction in the Adam’s apple without compromising structural integrity. The development of the structures previously described under hormonal influence is not reversible, and thus these features, which determine a significant part of an individual’s facial gender, can only be approached and modified with surgery. The surgeon must always respect the intrinsic architecture and anatomy of the craniofacial skeleton (Fig. 1-2). In addition to structural facial features, a series of secondary traits are equally important in the identification of facial gender. These include, most notably, the hair and hairline shape, facial hair, skin texture, and the distribution and volume of facial fat. The male hair may be conditioned by androgenic alopecia (loss of hair from hormonal influence) and have an M-shaped primary hairline, with recessions at the temples.10 The hairline of women usually has a rounded shape; their hair is not normally affected by alopecia, and proportionally the hairline implantation is higher in the center than in men.11,12 Almost all men have facial hair, which to a large extent conditions their skin type and quality, making it thicker and rougher. For many patients, facial hair is an important determining factor in their transition process. The distribution and volume of facial fat are equally influenced by hormones. Women have a greater volume of facial fat, with the distribution more concentrated in the middle third of the face (cheek area).13 Because all of these features can be heavily determined by hormones, they generally respond well to hormone therapy.14 Conceptually, secondary features play an important role in determining facial gender, and therefore it is preferable to treat them before beginning structural FFS (Fig. 1-3). Fig. 1-3 Patient before and 1 year after hormone treatment; note the change in secondary aspects (hair, facial hair, skin texture, and facial fat) before any type of surgical procedure was performed. One of the most important preliminary steps in FFS is a meticulous evaluation and diagnosis of the patient. Each patient has a unique facial structure, with specific features responsible for the male identification of the face, so it is important to adapt surgical options to a patient’s individual needs rather than taking a standardized approach. This diagnosis includes an accurate clinical evaluation, imaging tests, an evaluation of patient requests, and adjusting expectations. In addition, it is extremely important that photographs be taken systematically throughout the entire feminization process. Clinical evaluation consists of recognizing the features that contribute to male facial identification in a particular patient and identifying which of these features can be realistically and predictably modified with surgery. In this process, a distinction must be made between secondary aspects, which can be corrected with nonsurgical treatment, and the primary aspects that are conditioned by the individual’s craniofacial structure. This is why it is preferable for the patient to begin her hormonal transition early enough (at least 1 year before surgery), so that the secondary aspects do not obscure the diagnosis. The surgeon’s experience is essential when deciding the procedures that can most effectively contribute to the feminization of the face and therefore achieve a satisfactory result. The features that must be analyzed to obtain a thorough evaluation are listed here. The process is more easily understood when we differentiate four key areas: 1. Upper third: Hairline and frontonasal-orbital complex 2. Middle third: Nose, cheeks, and upper lip 3. Lower third: Jaw and chin 4. Neck: Thyroid cartilage (Adam’s apple) Each of these features must be evaluated not only on an individual basis but also in the context of the proportionality and symmetry of the face as a whole. Later in this chapter we analyze the details related to the evaluation of some specific features. Imaging tests are an essential part of a correct diagnosis and proper surgical planning. Today the combination of CT and three-dimensional reconstruction makes it possible to obtain detailed anatomic information. This is essential to detect the facial features that can be modified; these tests can provide the patient with precise information and assist in surgical planning. Moreover, comparing these preoperative images with postoperative CT results is extremely useful in assessing and explaining the changes made to the bone structure. In some patients we recommend the use of stereolithographic three-dimensional models to improve preoperative planning. In this respect the standardized incorporation of three-dimensional printing is an important advance in diagnosis. It is critical to listen to and understand the patient’s own ideas about her face. She will often provide valid ideas about the features that from her perspective determine the recognition of her facial gender. However, patients often have ideas about the possible results of their feminization surgery that are far from reality. The surgeon must explain that the surgery will modify certain features; at no time will surgery modify the core identity of the patient’s face or change it completely, because this is counter to the principle of naturalness, which is a basic tenet of facial gender modification surgery. If these factors are correctly addressed by the FFS specialist through sufficient consultation methods, the facial feminization treatment has the potential to emerge as a crucial step in the complex process of transition (Fig. 1-4). The entire process of a patient’s facial gender modification must be recorded in photographs, following a clear protocol. These should include clinical photographs, both preoperative and postoperative (7 days, 6 months, and 1 year after surgery), as well as intraoperative photographs of the procedures performed (Fig. 1-5). This complete photographic record gives an objective view of the changes obtained with FFS at different stages of the patient’s postoperative evolution. Fig. 1-5 Representative preoperative and intraoperative photographs taken before and during the FFS procedure. Postoperative results in the same patient after FFS procedure. Virtual facial feminization surgery (VFFS) is a powerful tool that makes it possible to predict the potential results of an FFS procedure with a high degree of realism (Fig. 1-6). It helps the patient to understand the effect of the proposed procedures on her facial gender; it also helps to adjust her expectations. For the surgeon, this tool is particularly useful when evaluating and diagnosing each case. The predicted results are always midterm or long-term depictions after the postoperative recovery phase has ended. Patients must be made aware of this fact when presented with their virtual result. VFFS must be done by experts in facial gender who can realistically predict the expected facial changes after the bone structure has been modified. However, as with all simulations, there is some margin of variability with respect to the results obtained with FFS.
Facial Feminization Surgery: A Global Approach
Key Points
 Facial feminization surgery is primarily based on structural bone modification and the consequent readaptation of the overlying soft tissues to the modified bone structure.
Facial feminization surgery is primarily based on structural bone modification and the consequent readaptation of the overlying soft tissues to the modified bone structure.
 Through bone sculpture, the volume or shape of the craniofacial skeleton can be modified by means of osteotomies, burring, or a combination of both. Bone sculpture is the keystone of facial feminization surgery.
Through bone sculpture, the volume or shape of the craniofacial skeleton can be modified by means of osteotomies, burring, or a combination of both. Bone sculpture is the keystone of facial feminization surgery.
 When facial feminization surgery is performed to adjust the facial features that influence the visual identification of a person’s gender, it can also be called facial gender affirmation surgery.
When facial feminization surgery is performed to adjust the facial features that influence the visual identification of a person’s gender, it can also be called facial gender affirmation surgery.
 Forehead reconstruction, which has a significant impact on facial gender identification, is one of the key procedures in facial feminization surgery.
Forehead reconstruction, which has a significant impact on facial gender identification, is one of the key procedures in facial feminization surgery.
 A preliminary and meticulous evaluation and diagnosis of a patient are essential to adapt the surgical options to her individual needs rather than taking a standardized approach.
A preliminary and meticulous evaluation and diagnosis of a patient are essential to adapt the surgical options to her individual needs rather than taking a standardized approach.
 The goal of facial feminization surgery is to obtain natural results with the use of hidden approaches, protocolized surgical techniques, and standardized postoperative management.
The goal of facial feminization surgery is to obtain natural results with the use of hidden approaches, protocolized surgical techniques, and standardized postoperative management.
What Is Facial Feminization Surgery?
Primary Aspects: Gender of the Craniofacial Skeleton
Frontonasal-Orbital Complex
Nose
Malar Region
Jaw and Chin Complex
Dentition
Thyroid Cartilage (Adam’s Apple)
Secondary Aspects
Evaluation and Diagnosis
Clinical Evaluation
Imaging Tests
Evaluating Requests and Adjusting Expectations
Collecting Photographs
Virtual Facial Feminization Surgery
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine