Facial Artery Perforator Flap
Julian J. Pribaz
Simon G. Talbot
DEFINITION
Perforator flaps are a relatively recent addition to our reconstructive techniques.
They have evolved as a result of meticulous studies of vascular blood supply to the skin, which have demonstrated a rich network of perforator vessels arising from all major vessels, allowing for the elevation of safe and customized flaps based on these vessels.
ANATOMY
Arterial
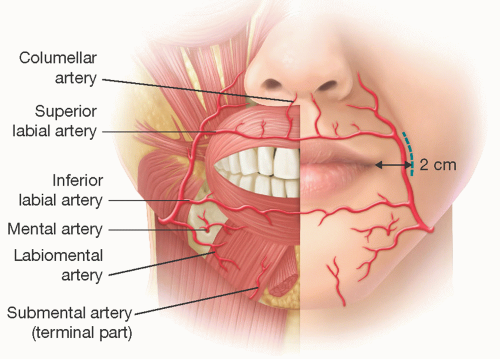
The facial artery enters the face by hooking around the lower border of the mandible at the anterior edge of the masseter muscle. It follows a tortuous course through the cheek, passing upward and medially toward the oral commissure and then to the alar base, where it becomes the angular artery (FIG 1).
It passes deep to the muscles of facial expression and gives off two major named vessels—the inferior and superior labial arteries—as well as multiple perforators to all surrounding structures, including the superficial and deep muscles, skin, and mucosa.
Hofer mapped out the perforators supplying the skin and found that these were multiple, with at least three perforators having an average diameter of 1.2 mm. His injection studies showed that a single perforator can supply a large area of facial skin, thus making it useful for perioral reconstruction.7
Venous
The main facial vein does not run with the artery but is located more laterally in the cheek and approaches the facial artery near the angle of the mandible.
There are multiple small venous channels in the soft tissues that provide adequate drainage to perforator flaps. However, it is important not to skeletonize the pedicle but rather leave a cuff of soft tissue to allow for venous drainage.
This is an important distinguishing feature of facial artery perforator flaps compared with those harvested from other parts of the body in which the perforating vessels are routinely skeletonize to maximize flap reach and rotation. Because of the tortuous nature of the artery and the mobility of tissues in this region, it is still possible to rotate safely the flap up to 180 degrees.
PATIENT HISTORY AND PHYSICAL FINDINGS
The soft tissues making up the nasolabial fold and jowl area are lax and mobile. Fortunately (from the reconstructive point of view), these qualities increase with aging, when the need for flaps from this donor site also increases to deal with surrounding defects created after tumor extirpation. The tissue laxity facilitates primary repair of the donor site.
In addition, this area of the skin lies directly over the course of the facial artery and its perforators, allowing for safe flap elevation and repair.
Superiorly and inferiorly based pedicled nasolabial flaps with a skin bridge have been used successfully since ancient times. The inclusion of a skin bridge makes the flap bulky, limits its mobility, and distorts the surrounding anatomy. It also requires a secondary procedure to divide and inset the flap.
A better understanding of the anatomy of perforators refined and developed island flaps supplied by one or more perforators devoid of skin bridge, which has made it easier to rotate the flap and perform more one-stage reconstructions.
Perforator flaps based on the facial artery can be considered for all substantial defects of the perioral region, lips, distal nasal, and cheek (FIG 2).
They have the advantage of using local “like tissue” adjacent to the defect, which results in aesthetically superior reconstructions. This includes the use of hair-bearing skin from the jowl area for mustache and beard reconstruction.
As the facial artery is sandwiched between the superficial muscles of facial expression and the deeper buccinator and
mucosa (which are all supplied by the facial artery), it is possible to raise a composite full-thickness cheek island flap if this is what is needed for reconstruction.
To avoid injury to the muscles of facial expression, the deep part of this flap can be harvested just inferior to the risorius muscle, where only the buccinator muscle is taken with the flap (FIG 3).
 FIG 2 • A. Patient with nostril sill and upper lip defect after excision of basal cell carcinoma. B. Superiorly based island perforator nasolabial flap. C. After single-stage flap transfer.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|