Chapter 9 Facelift with SMAS Flaps
Summary
Introduction
Facelift techniques
Some of the advantages and disadvantages of different facelift techniques are listed in Table 9.1.
Table 9.1 Advantages and disadvantages of different types of facelift techniques
| Facelift | Advantages | Disadvantages and complications |
|---|---|---|
| Skin only | Conceptual and technical simplicity | Secondary facelift deformities caused by skin tension |
| SMAS plication | No sub-SMAS dissection so technically less demanding and time consuming than procedures in which a flap is raised | Wide skin flap undermining; contour irregularities if sutures are not placed carefully; potential injury to facial nerve branches and parotid gland or duct; little if any midface improvement |
| SMASectomy | No sub SMAS dissection required; skin and SMAS can be shifted along different vectors so skin tension can be set low, and sideburn displacement and shifting of cervical wrinkles onto the face can be minimized | Wide skin undermining; facial nerve branches at risk when SMAS excised and sutured; may be contour irregularities; minimal improvement in midface |
| Deep plane | Single-layer dissection so flap elevation is easier and less time consuming than multilayer dissection and flap is thicker with a better blood supply | Potential excessive sideburn displacement, and shifting of cervical rhytids to the face; unnatural appearances caused by extraordinary tension; midface improvement not always as expected; facial nerve branches and other structures at risk |
| Composite | Similar to those for a deep plane lift, but also allows repositioning of orbicularis oculi and raising of lid-cheek junction | Similar to those of deep plane technique, but also may be prolonged periorbital edema and denervation of orbicularis oculi |
| Lamellar SMAS dissection and bidirectional | Skin and SMAS advanced bidirectionally in different amounts along separate vectors, and suspended under differential tension so avoiding skin tension, hairline displacement, and wrinkle shifts | Technique dependent and time consuming; flaps more fragile; facial nerve branches at risk |
| Extended SMAS | Improved effect in the mid face and infraorbital region and increased support of the lower eyelid | More technique dependent and time consuming; flap is more fragile; facial nerve branches at risk |
| High SMAS | Restoration of youthful upper cheek contour; filling of infraorbital region; increased support of lower eyelid; improved correction of nasolabial fold; readily combined with midface fat injections | Similar to those techniques using a sub-SMAS dissection |
| Subperiosteal | Dissection is familiar to most plastic surgeons and is largely deep to facial nerves; avoids many problems associated with skin-only procedures; improvement in infraorbital and upper midface areas in some cases | Generally longer recovery and often hard to obtain optimal improvement along jawline; problems of suspension sutures |
| Endoscopic | Minimal scarring | No means for skin excision; little improvement in lower cheek and along jawline |
| Midface | To improve midface area | Steep learning curve and fraught with complications, especially when performed through a blepharoplasty incision, including lid retraction, ectropion, canthal displacement and dry eye; disappointing results |
| Suture suspension | Seeming simplicity; easy marketability; can often be placed quickly under local or light anesthesia by inexperienced surgeons without surgical training; small incision; lower risk of hematoma, flap compromise and related complications | Support of the face cannot be predictably obtained; infection; extrusion; traction dimples; visible bowstringing; nerve injuries; facial dyskinesias; chronic pain syndromes; abnormal appearances during animation; a tight or choking feeling when used in the neck; palpable knots and sutures beneath the skin and occasional erosion of overlying skin |
| MACS (minimal access cranial suspension) | Seeming simplicity; no formal SMAS dissection; can be performed under local or light anesthesia; a shorter scar; shorter operating time. | Technique dependent and contour irregularities can result; problems associated with the placement of a stiff and rigid suture in the superficial layers of the face; injury to the parotid gland, parotid duct, facial nerves, and other deep facial structures |
| Short scar | Appeal to patients | Limited access to deep layer structures; redundant skin cannot be shifted along proper vectors; prevent skin from being properly excised |
| Mini-lift | Appeal to patients | Minimal improvement |
Skin only
Although the excision of skin formed the foundation of the facelift procedure for the first 70 years or so after its inception, this has ultimately been shown to be ineffective and conceptually flawed, and there are compelling reasons (Box 9.1) not to rely on skin resection only when surgically rejuvenating the face.
Box 9.1 Reasons why skin-only resection should not be relied on when surgically rejuvenating the face
Skin is intended to serve a covering function, not a structural or supporting one
SMAS
SMAS plication
Disadvantages of the SMAS plication technique are:
SMASectomy
Advantages of SMASectomy technique are:
Potential disadvantages of SMASectomy are:
Deep plane
A deep plane facelift consists of a sub-SMAS dissection first described by Skoog and later popularized by Lemon and Hamra in which the cheek skin and SMAS are raised together in one layer as a unified flap (Skoog flap). In the deep plane procedure the SMAS was used to reposition the lower cheek and jowl and the midface was then said to be elevated by ‘extraordinary tension’ on the preauricular portion of the flap.
Advantages of the deep plane technique include:
Composite
Advantages of the composite technique are:
Lamellar SMAS dissection and bidirectional facelift
Disadvantages of procedures that use lamellar SMAS dissections:
Extended SMAS
Disadvantages of the extended SMAS procedure compared with a standard dissection include:
High SMAS
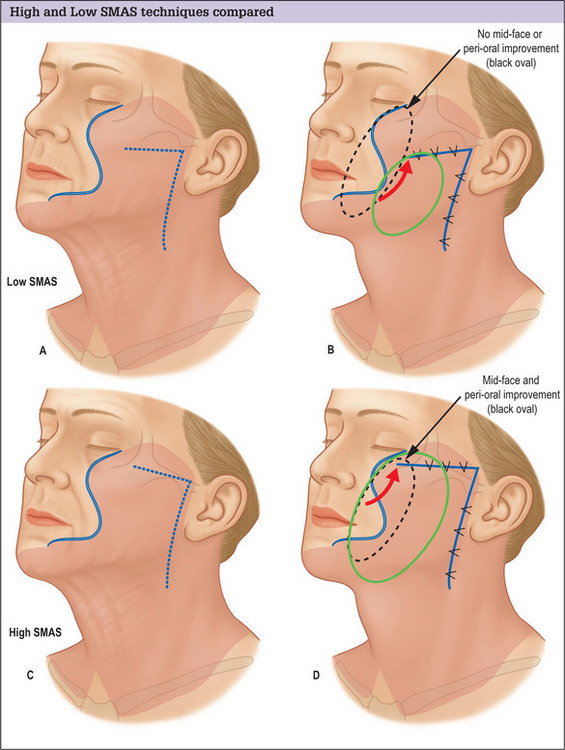
The conventional low cheek SMAS flap design in which the superior margin of the flap is planned below the zygomatic arch suffers the fundamental design flaw that it does not exert an effect on the tissues of the midface and infraorbital region. Low designs target the lower cheek and jowl only, and produce little if any improvement in the upper medial cheek area. Planning the flap higher, along the superior border of the zygomatic arch and making an extended dissection medially to mobilize midface tissue overcomes this problem and produces an improved result (Fig. 9.1A-D).
Advantages of a high SMAS plan include:
For many patients, the repositioning of midface tissue obtained with a high SMAS flap will be satisfactory in achieving the desired effect, and no additional or separate midface lift procedure will be required (Fig. 9.2A&B).
Subperiosteal
Potential advantages of a subperiosteal facelift include:
Potential disadvantages of the subperiosteal technique include the following:
Midface
Although there is merit in the idea of rejuvenating the midface, isolated midface lift procedures are still evolving, and have not been perfected. Most procedures have a steep learning curve and have been fraught with complications, especially when performed through a blepharoplasty incision. These complications include lid retraction, ectropion, canthal displacement and dry eye problems. As a result, many midface lift techniques have come to incorporate potentially problematic aggressive adjunctive surgical maneuvers including can thotomies, canthoplasties and orbicularis oculi muscle suspensions to prevent these problems. These maneuvers often result in a changed look that is disturbing to many patients, however, and carry a high risk of significant and troublesome complications of their own.
Suture suspension
Advantages of suture-lift procedures include:
Disadvantages of suture-lift procedures include:
MACS lift
The MACS procedure has evolved and has been refined from its original description in which one or two plication sutures were placed and non-absorbable permanent monofilament sutures were used. Multiple sutures are now generally placed to more specifically target the midface, cheek, jowl and lateral neck, and this is said to distribute improvement more uniformly over the face and produce a more natural and long-lived improvement. Softer, absorbable sutures have also been substituted for the stiffer more rigid non-absorbable sutures originally recommended.
Potential advantages of the MACS technique include:
Potential disadvantages of the MACS technique include: