42. Facelift
Adam H. Hamawy, Dino R. Elyassnia
PREOPERATIVE EVALUATION
■ Consult with the patient to develop rapport while determining anatomic, psychological, and medical suitability.
■ Establish baseline health and intercurrent illnesses, tobacco use, prior surgeries, and prior cosmetic treatments (i.e., botulinum toxin, lasers, and fillers). Carefully assess surgical risk based on medical history.
■ Perform a systematic facial examination focusing on individual components and how they interact with the whole to give the appearance of facial aging.
ASSESSING THE AGING FACE1
■ Facial aging is a function of soft tissue sagging, volume loss from atrophy, and skin surface changes.
SKIN QUALITY
■ Skin thickness and elasticity are assessed.
■ Dermal atrophy occurs with age and actinic damage.
■ Thin, crêpey dermis is less elastic and less likely to maintain a smooth appearance after redundant skin has been removed.
■ Trimming excess skin will address redundancy and reestablish some tone; however, the degree that can be maintained over time is limited by the residual skin elasticity.
SOFT TISSUE VOLUME
■ Subcutaneous fat is distributed in discrete anatomic compartments.
■ Facial fat compartments lose volume and deflate with time.2
■ The superficial musculoaponeurotic system (SMAS) and platysmal laxity contribute to the downward migration of facial tissues that develops with aging.3
■ Alteration in fat distribution and soft tissue laxity result in a morphologic change from a youthful “heart shape” to an aged, square appearance4 (Fig. 42-1).
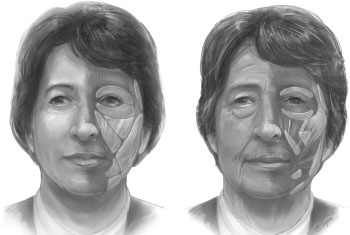
Fig. 42-1 The facial fat compartments and their aging changes. Aging leads to an inferior migration of the midfacial fat compartments and an inferior volume shift within the compartments. Deflation of the buccal extension of the buccal fat aggravates the inferior migration of the medial cheek fat, middle cheek fat, and suborbicularis oculi fat.
■ Restoring volume and proper redistribution of soft tissue can help to restore the appearance of youth.
SENIOR AUTHOR TIP: Patients with significant facial atrophy and age-related facial wasting will generally achieve suboptimal improvement from both surface treatments of facial skin and surgical lifts. Restoring lost facial volume using fat injections can produce a significant, sustained improvement in appearance that is unobtainable by other means. However, age-related facial atrophy rarely exists in isolation, and most patients troubled by it are not always appropriately treated by fat injections alone. Isolated fat injections are of questionable benefit to patients with significant facial sagging. Although aggressive filling of the sagging face can improve facial contour, it generally results in an unusually large, unnatural appearance. It is more logical to perform fat injections in conjunction with a facelift or after ptotic tissue has been treated.
SKELETAL SUPPORT
■ The facial skeleton loses volume and changes with age.5
■ Loss of skeletal support adds to the appearance of facial deflation and aging.
■ Skeletal augmentation can be an effective method to address changes of facial aging and establish support for overlying soft tissue (Fig. 42-2) (see Chapters 27 and 40).
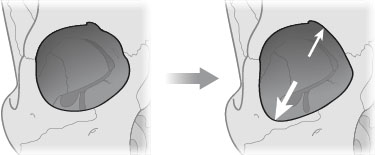
Fig. 42-2 The bony orbit of a young female subject on the left and an older female subject on the right. The aged orbit may be rejuvenated with volume augmentation.
FACIAL ANALYSIS
■ Assess and address the entire face as a whole to maintain facial harmony.
■ The key steps to consistent results are a thorough preoperative analysis and development of an operative plan to address individual aesthetic needs.
Forehead
■ Assess facial proportions. Forehead should represent the upper third of the face, measured from hairline to pupil.
■ Note the presence of active and passive wrinkles on the forehead from frontalis activation and on the glabella from contraction of the corrugators and procerus.
• Passive wrinkles (static rhytids) do not disappear with relaxation. Passive wrinkles are best addressed by skin resurfacing treatments and will only be minimally improved by chemodenervation or surgical lifts.
• Active wrinkles (dynamic rhytids) occur with animation and can be voluntary or involuntary. Active wrinkles can be improved with chemodenervation and possibly browlifting.
■ Evaluate medial and lateral brow position in relation to orbital shape and upper lid.
NOTE: Lateral brow ptosis can give the appearance of excess upper lid skin and should be corrected with a browlift rather than a blepharoplasty.
Upper Eyelid
■ Identify lid ptosis, characterized by a low resting lid margin and high supratarsal crease. Both brow and eyelid ptosis should be addressed in the surgical plan.
■ Assess the amount of upper eyelid skin. Compensate for excess skin from lateral brow hooding by manual repositioning of the lateral brow.
■ Assess periorbital fat, which will most often manifest as deflation and hollowing of the upper orbit.
Lower Eyelid
■ Note the relationship of the orbital rim to the anterior surface of the globe (Fig. 42-3).
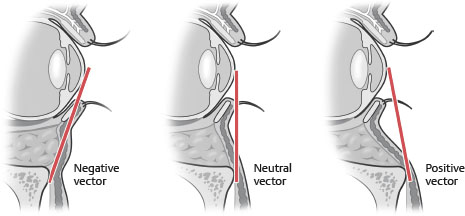
Fig. 42-3 Orbital vectors.
• Positive vector orbits provide better support for lid suspension.
• Negative vector orbits lack support and should be addressed by planning additional lower lid support or midface soft tissue augmentation.
■ Globe prominence may indicate thyroid disease that should be treated appropriately.
■ Assess lid tone and tarsal suspension using a lid snap-back test and lid distraction test.
■ Determine skin laxity and quality. Trimming of excess lower eyelid skin must be very conservative to prevent complications.
■ Assess for laxity of the orbicularis muscle, sometimes evident by the presence of festoons.
■ Note bulging of fat, laxity of the orbital septum, and fat loss in the lower orbit.
Cheek
■ Examine skeletal proportions and the relationship of the bizygomatic diameter and maxillary height.
■ Note the distribution of subcutaneous fat and tissue in relation to underlying bony structure.
■ Assess depth and prominence of the nasolabial folds, which indicate volume loss and inferior migration of overlying tissue secondary to deflation of fat compartments.
■ Jowls indicate shelving from ptotic cheek tissue or excess fat that may need to be addressed. Jowls can be accentuated by tethering at the mandibulocutaneous ligament that should be released or by volume loss along the jawline that should be replaced.
Perioral Area
■ Note the presence of marionette lines from the oral commissures to the mandibular border.
■ Assess for volume loss in the lips and lengthening of the upper lip. Note degree of upper incisor show at rest.
■ The presence of a weak chin should be discussed with the patient and possibly addressed in the surgical plan.
■ Deep perioral rhytids are important to note and will not improve with facelifting. Proper treatment will require skin resurfacing as an additional part of the surgical plan.
Neck
■ Assess for presence of soft platysmal bands visible in repose, and hard bands visible with platysmal activation.
■ Soft bands will respond to repositioning of lax platysma (i.e., platysmaplasty), whereas hard bands will require platysmal myotomy.
■ Excess fat can be located superficial or deep to the platysma. Depending on the extent and location, this can be addressed by liposuction or direct excision.
■ The amount of skin laxity is important to note; however, addressing the skin in isolation without considering the underlying structures will result in a modest improvement at best.
SENIOR AUTHOR TIP: For many patients, subplatysmal fat accumulation, submandibular salivary gland “ptosis,” and digastric muscle hypertrophy will contribute significantly to their neck deformity. As patients age, fat stores generally shift from preplatysmal to subplatysmal, and the small amount of subcutaneous fat present in a typical patient presenting for a facelift is needed to preserve a soft, youthful neck. Excess subplatysmal fat is usually present in patients with firm, obtuse necks who have had lifelong cervicomental fullness. In these patients, partial subplatysmal lipectomy will be productive. Submandibular glands are usually palpable as firm, discrete masses in the lateral submental triangle, lateral to the anterior belly of the digastric muscle and medial to the mandibular border. Glands lying deep to the plane tangent to the inferior border of the mandible and ipsilateral anterior belly of the digastric muscle do not disrupt neck contour and will usually not require treatment. However, glands protruding inferior to this plane are likely to be problematic if excess cervical fat is removed and redundant skin excised. A small subgroup of patients will have digastric muscles with large, bulky anterior bellies that are evident as linear paramedian submental fullness. As in the case of large submandibular glands, large digastric muscles are frequently hidden by excess subplatysmal fat or lax platysma. In these patients, subtotal superficial digastric myectomy should be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




