Eyelid and Periocular
BIOANATOMY AND BIOMECHANICS
The upper eyelid begins superiorly at the superior orbital crease beneath the eyebrow and ends at the free margin of the upper lid. The lower lid begins at the infraorbital crease that corresponds roughly but not exactly to the reflection of the orbital rim. The anatomy of the eyelid is complex and three-dimensional. Prior to performing any form of eyelid surgery, a thorough study of anatomy must be undertaken (Fig. 10.1).
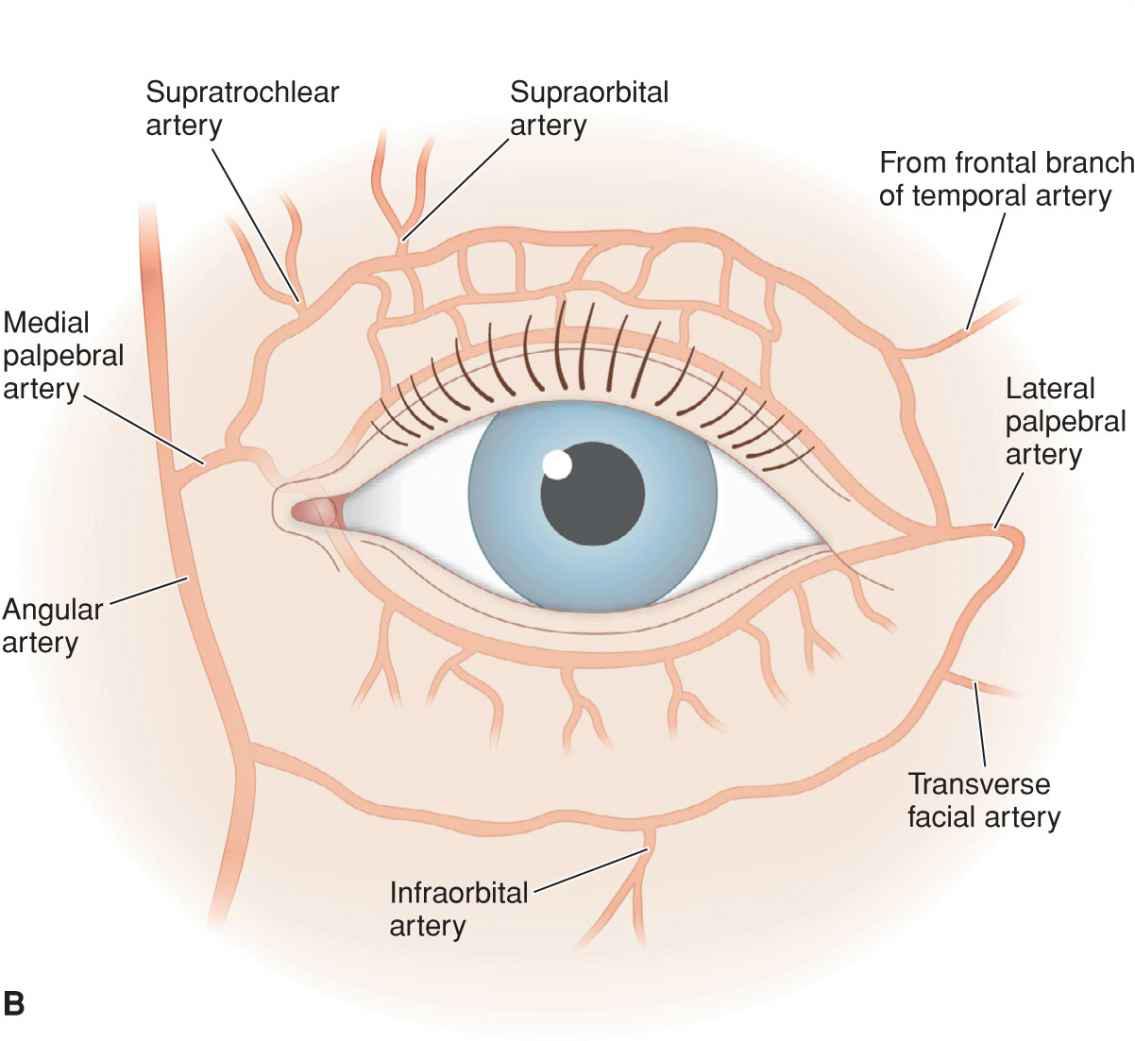
Figure 10.1 Periocular anatomy. (A) Structure of the eyelids. The eyelids are suspended by tendons medially and laterally. The lacrimal gland is located at the superolateral aspect deep to the orbicularis oculi. The lacrimal drainage apparatus is protected by the anterior leaflet of the medial canthal tendon, which is cut away in this diagram. In cross section, the lower lid is composed of conjunctiva, tarsal plate, orbicularis musculature, and skin. (B) Arterial supply of the eyelid. The eyelids receive rich and redundant blood supply from the internal and external carotid systems
The eyelids are suspended medially and laterally by tendons and are multilaminar free margin structures. The lids function to protect the eye from trauma and they keep the eyes moist and lubricated. The anchoring tendons of the eyelid are bifurcated structures with deep and superficial components. The medial canthal tendon originates medially from the anterior and posterior lacrimal crests and from the frontal process of the maxillary bone. The superficial portion of the medial canthal tendon protects the lacrimal drainage system that passes just deep to the tendon insertion to drain into the nasal cavity. The lateral canthal tendon is firmly attached to the zygomatic bone at Whitnall’s tubercle just within the bony orbit. Between the two tendons stretch the dense, fibrous tarsal plates, which provide structural support to the eyelids.
The lacrimal glands, the meibomian glands, and the lacrimal drainage system strike a balance between the creation of lubricants and their removal. The meibomian glands are embedded in the tarsal plate and empty onto the palpebral conjunctiva. The lacrimal glands lie within the superolateral orbit. The canalicular drainage system originates from the medial most upper and lower lids, where two punctae are visible. The canaliculi join posterior to the anterior leaflet of the medial canthal tendon and dive deep from that point medially.
The lids consist of the tarsal plate covered by laminae of mucosa, muscle, fat, and skin. The complex anatomy of the eyelids is beyond the scope of this discussion and is eloquently described elsewhere. The external lids consist of a thin, redundant, mobile epidermis and dermis overlying a circumferential track of orbicularis oculi. The skin of the eyelid is loosely attached to the orbicularis and can be extensively mobilized from the underlying muscle.
The vascular supply to the periocular area is extensive and redundant. As a watershed area, the eyelids receive input from the superficial temporal artery laterally, from the infraorbital artery inferiorly, from the supraorbital and supratrochlear arteries superiorly, and from the angular artery medially. Eyelid flaps are therefore robust and rarely undergo necrosis, even when subject to forces which would compromise repairs in other areas. On the other hand, the eyelid is a free margin, and as such, it is prone to distortion and displacement. Lower lid ectropion and upper lid lag are common sequelae of repairs that place undue vertical tension on the upper and lower lids. If the ectropion is medial, the lacrimal punctae are often displaced anteriorly and away from the globe, thus creating symptomatic epiphora. Upper lid lag is a bit less problematic but can lead to xerophthalmia in some cases. For that reason, it is imperative to plan periocular repairs with substantial caution, always paying attention to the projected final position of the lid on the globe.
The size, shape, and position of the eyelids vary greatly from individual to individual and with time in the same person. With age, the eyelids often become redundant and folds of upper lid skin frequently develop. At the same time, the lids lose their innate elasticity and rebound from stretch with much less force. A vertical tension that is well tolerated in a younger patient may produce a debilitating ectropion in an older patient. It is also important to realize that a repair that looks great at 1 week may still result in an ectropion as maturation of the reconstruction produces vertical contractile forces. For that matter, a repair that is well supported at 1 year may eventuate in an ectropion several years later, thus requiring a delayed revision.
The eyelids heal extremely well following reconstructive surgery. Complex repairs which elsewhere might result in prominent visible scars may heal on the eyelid almost invisibly. Most important in reconstructing the eyelid is its functional integrity and the ability to cover the eye upon lid closure. It is equally important to avoid lower lid ectro-pion and entropion and to maintain, where feasible, the integrity of the upper and lower lacrimal canalicular systems. Finally, notching of the eyelid margin is to be avoided. This chapter deals with the reconstruction of anterior lamellar wounds and small-to-modest full-thickness wounds. Larger full-thickness wounds that require tarsoconjunctival flaps or free tarsal grafts, and those requiring lacrimal system reconstruction, are usually handled in conjunction with an oculoplastic surgeon. For that reason, they are not included herein.
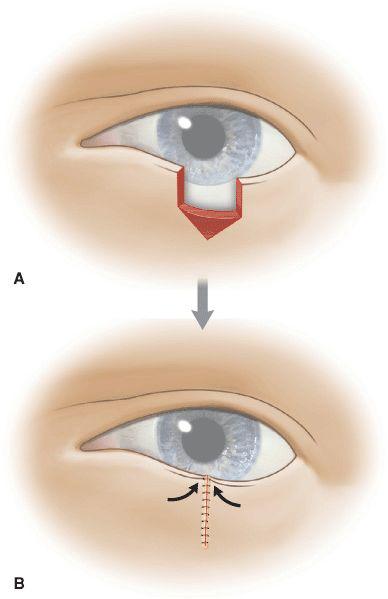
LID WEDGE
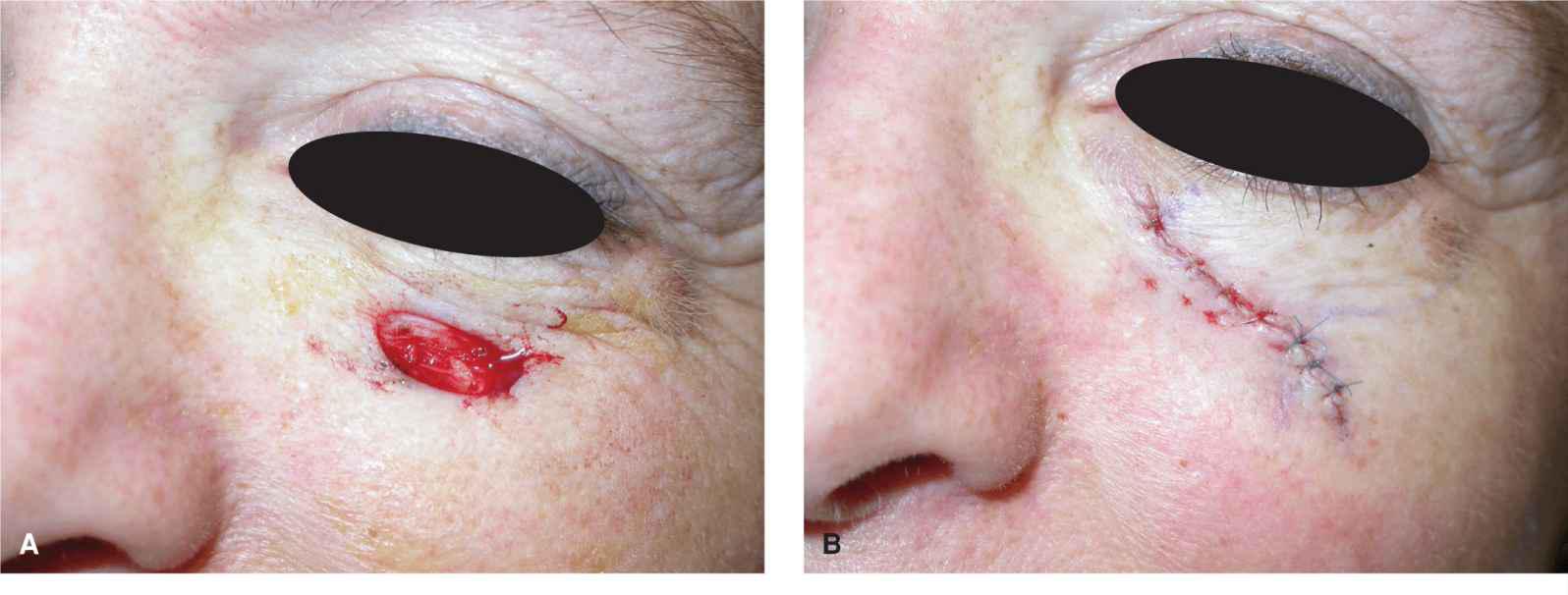
Small-to-moderate defects of the lower eyelid can be repaired simply with a lid wedge.1 The defect generally comprises less than one quarter or one-third of the lower lid and involves the lid margin. The repair is a basic multilayer closure. First, the defect is squared off and any remaining tarsus is removed. Many approaches to the skin of the eyelid have been described, the most popular of which is to create an inverted pentagon. The inverted pentagon design inherently pushes the repair upward, thus mitigating the forces that might cause ectropion. Alternatively, the standing tissue cone can be directed inferolaterally (Figs. 10.2 and 10.3).
Figure 10.2 Eyelid wedge. (A) A lid wedge repair is designed with an inverted pentagon. (B) As the wound is closed side to side, there is an upward motion on the lid margin which limits the potential for lower lid notching or ectropion
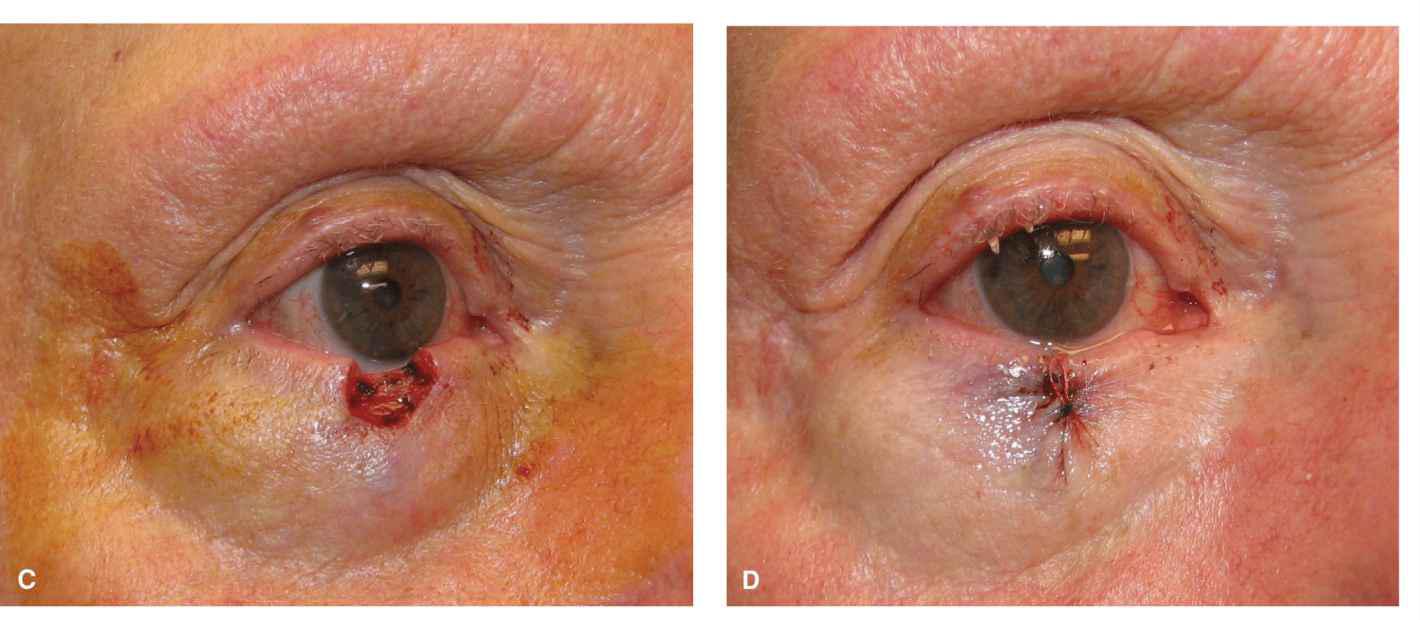
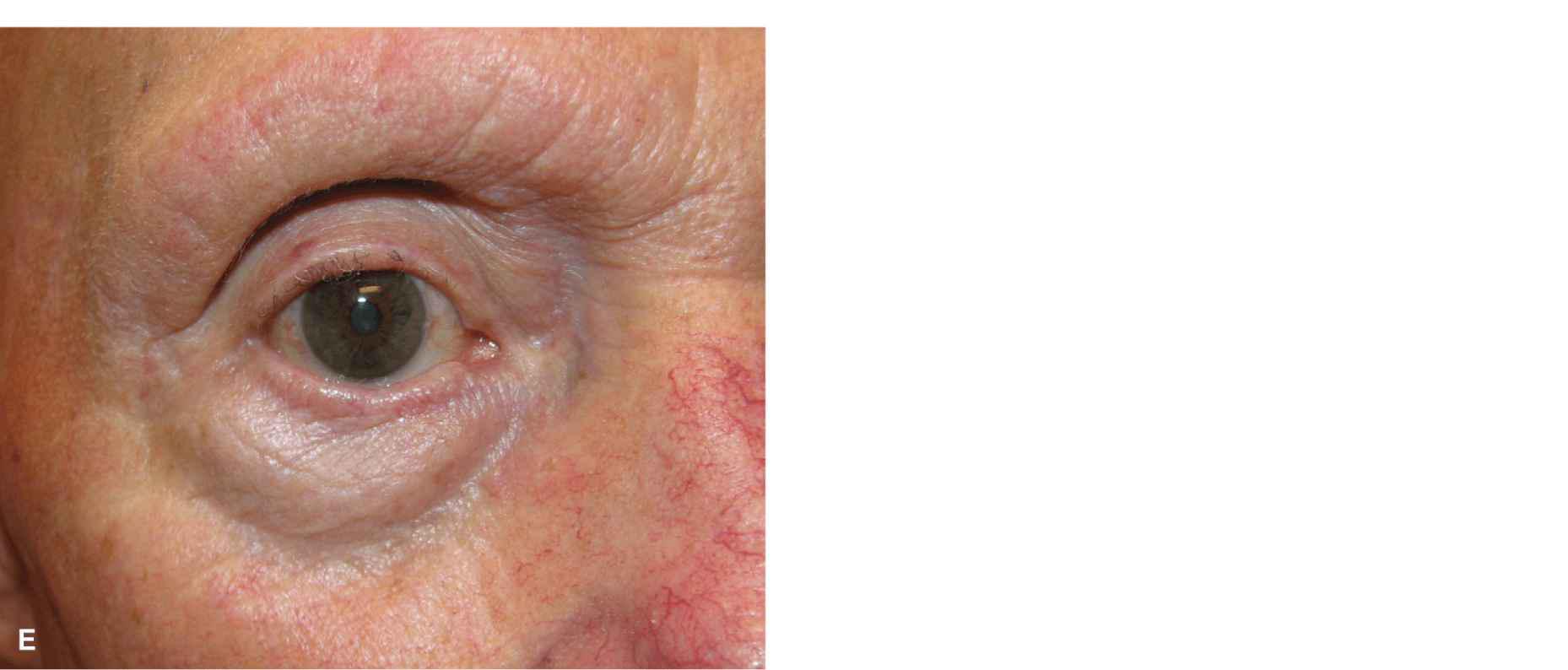
Figure 10.3 Eyelid wedge. (A) A lateral wound constituting about 30% of the lower lid. (B) Adequate laxity exists for a wedge closure. (C) Small full-thickness wound of the lower lid. (D) Immediate repair. (E) Reconstruction at 1 year
The closure Is multllayered. The mucosa is not sutured. A single tarsal suture is often all that is needed to close the operative wound. Sometimes two tarsal sutures are employed. The knots from any tarsal suture should be exterior to the tarsus to avoid disruption of the palpebral conjunctiva with potential corneal abrasion.
The margin of the lid may be closed with a single, soft braided suture such as a silk or Mersilene suture. The lid margin may not need to be approximated superficially at all if the tarsal sutures are very well placed. If the margin is sutured, it is essential that the suture be slightly anterior to the actual lid margin, and the free ends of the suture should be left long and then sewn down to the cutaneous lid to keep them from rebounding and scratching against the eye. As the lid margin is approximated, it is important to ensure that no notching will take place and that there is no undue tension on the lid. If there is a lot of tension, the repair will tend to create an entropion, and the lower lid lashes may rub uncomfortably against the eye. If the repair appears to be under tension, a substantial release of restraint can be achieved by lateral cantholysis, which will provide up to 5 mm of additional horizontal motion. The loose skin of the lid can be approximated with absorbable sutures or sutures to be removed in about 5 days.
Linear Repairs
Many operative wounds of the lower lid can be repaired in a side-to-side fashion, albeit straight linear repairs on the eyelid are uncommon. Defects of the lower lid are rarely vertically oriented and tend to be either circular or oval. The lower lid is also a structure with topography. The lid itself bows slightly inward toward the orbital rim and then reflects convexly to the cheek at the maxillary bone or zygoma. As a result, repairs that bridge the cheek and eyelid tend to tent and form extensive redundant tissue cones. While these do improve with time, avoiding their creation is not difficult. In most cases, the design of a repair as an S-shaped closure will result in the appropriate side-to-side length mismatch to counteract the creation of dog-ear which would otherwise result (Figs. 10.4 and 10.5). The superior limb that rests on the eyelid is curved concave up and the inferior limb is curved concave down. The tension vector is directed medially to laterally at the infraorbital crease, and therefore ectropion is avoided.


Figure 10.4 S-shaped repair of the lower lid. (A) Operative wound and S-shaped repair. (B) Immediate closure. The incorporation of an S-shape into the repair allows for the less dog-ear formation on the lid and cheek and also diminishes the tenting effect of a linear repair at the concave deflection from lid to cheek. (C) Repair at 1 year. Eyelid repairs may be almost invisible on long-term follow-up
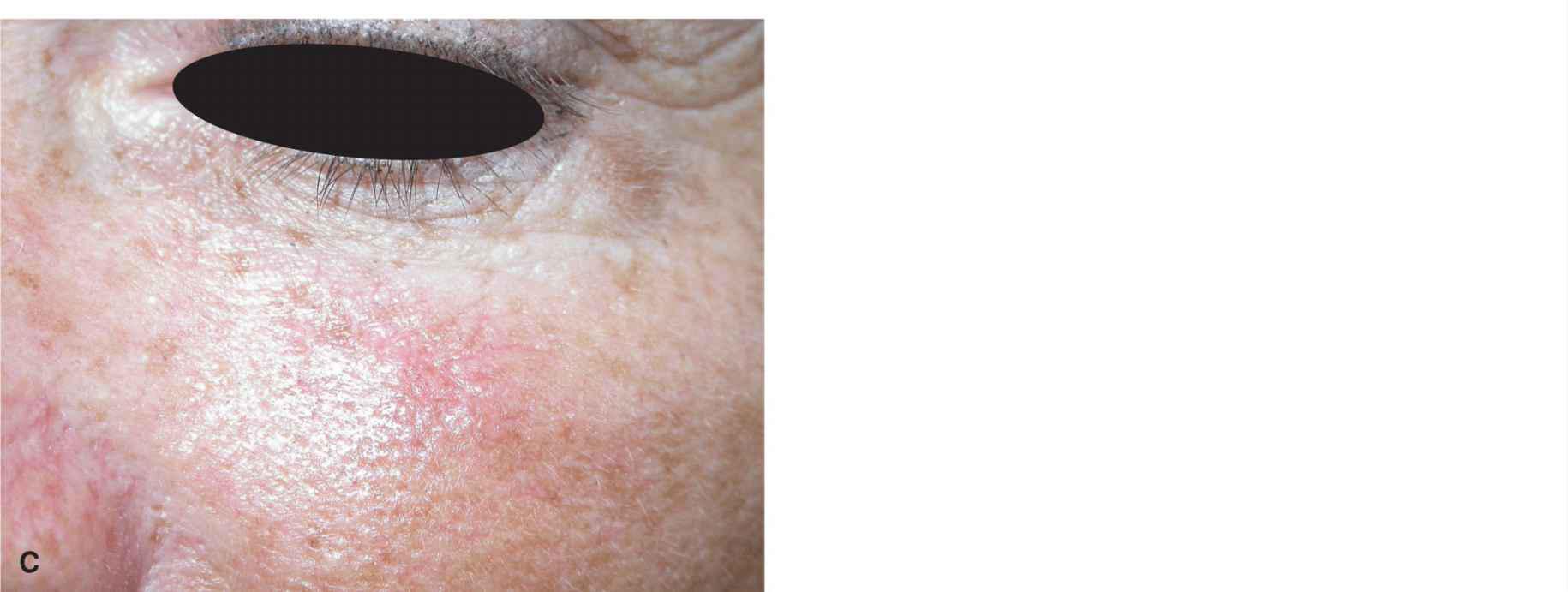
Figure 10.5 S-shaped repair of the lower lid. (A) Horizontal operative wound at the junction of the lid and cheek. (B) S-shaped repair places minimal to no tension on the lower lid margin. (C) Repair at 4 months demonstrating slight erythema
This is a repair where the depth of the closure is best differential. The lid portion of the repair should be performed above the orbicularis oculi. The cheek portion of the repair should be performed at the deeper subcutis above the deepest and most inferior fibers of the orbicularis. Where the lid reflects on the cheek, the two undermining planes are connected. This serves to lyse the adhesion of the eyelid skin to the underlying muscle and allow much greater mobility without pulling on the actual structure of the lid. As the repair heals, the infraorbital crease is nicely recreated and this repair is often clinically invisible.
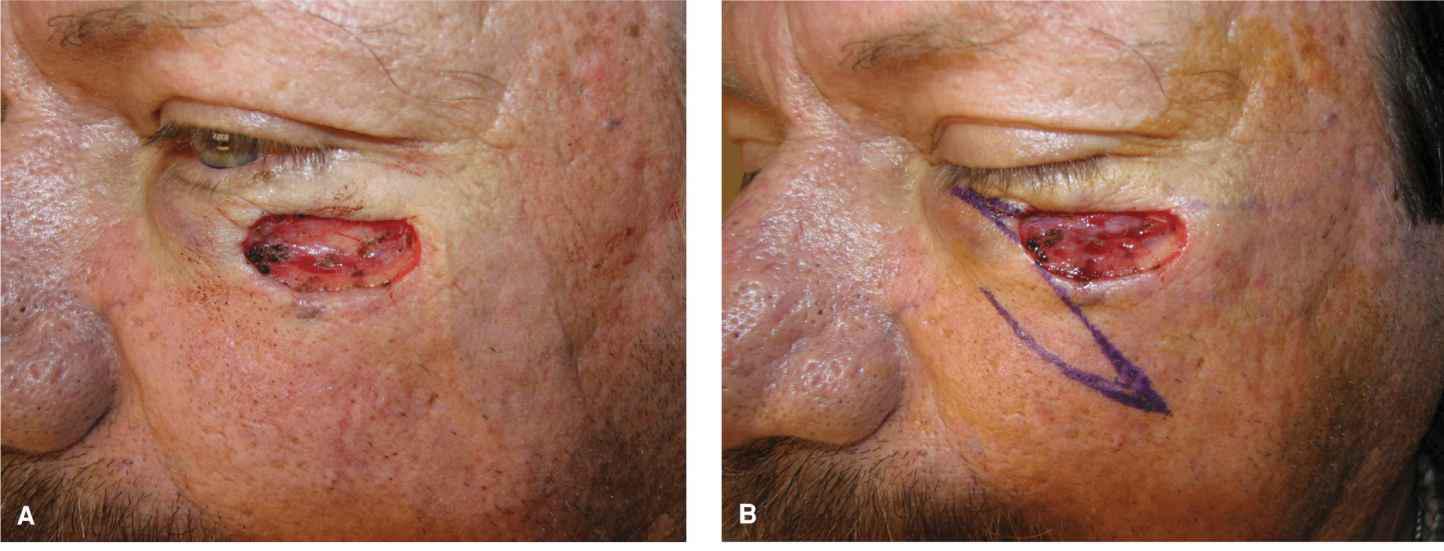
Banner Transposition
Oblique and horizontal wounds of the lower lid can present a challenge. In young individuals with a good lid snap test, an S-shaped closure can be utilized to close fairly sizeable wounds. In older individuals, the lack of lid elasticity predisposes to ectropion and all tension must be directed medially to laterally. In such cases, an innovative repair is a superomedially based banner transposition flap (Figs. 10.6 and 10.7). From the inferomedial aspect of the oval wound, a tangent is dropped inferiorly at about a 90° angle. The banner flap is designed on this tangent and rotates and transposes superiorly with little to no tension. This repair is elevated strictly as a subcutaneous flap. Its vascular supply is from perforators and is exceptional, which is important in this case.
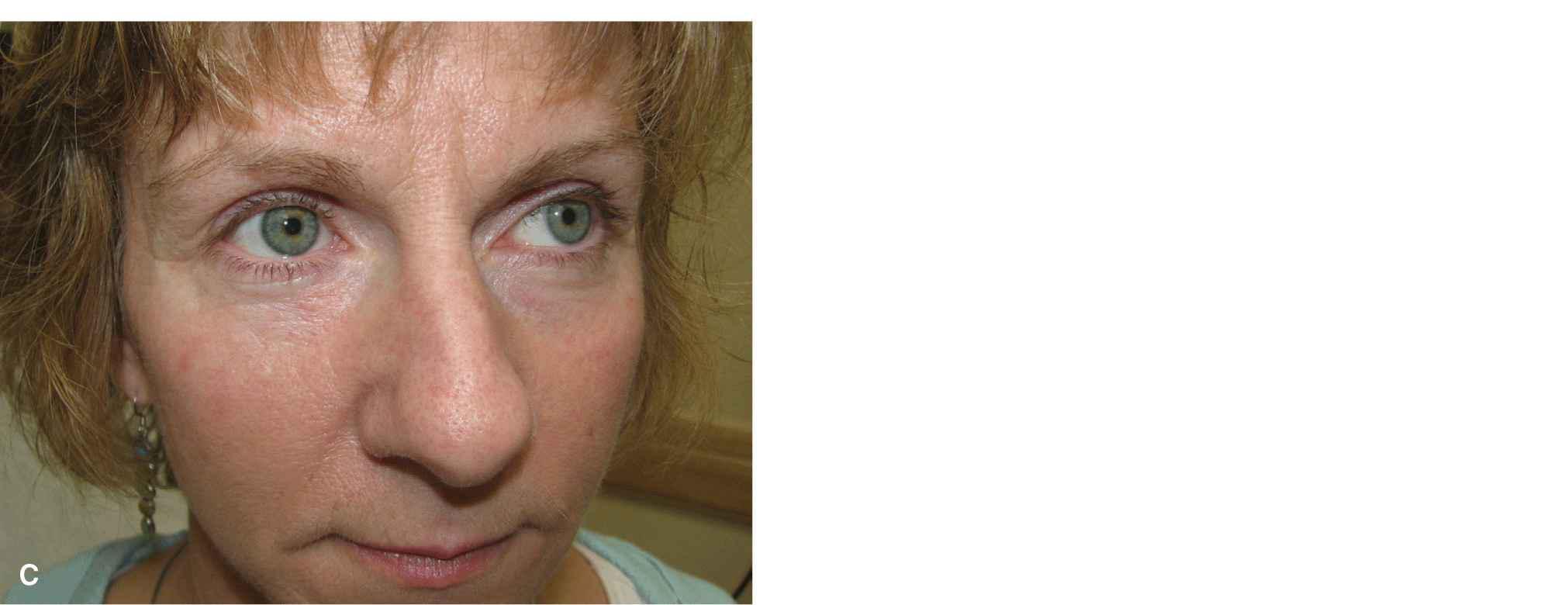
Figure 10.6 Horizontal lower lid wound repaired with a banner transposition flap. (A) Operative wound and planned transposition. (B) Immediate repair. All tension is directed medially to laterally and the flap transposes and rotates into place under little to no tension. Eyelid banner flaps must be meticulously thinned and appropriately sized, and the surrounding tissues should be undermined. Pincushioning is not uncommon. (C) Repair at 6 months

Figure 10.7 Larger, more lateral cheek and lid wound repaired with a banner transposition flap. (A) Operative wound with a greater horizontal than vertical dimension. (B) Planned banner transposition. (C) Immediate reconstruction. All tension has been directed along horizontal vectors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree