80 Eyebrow Transplantation
Summary
Keywords: brows eyebrows brow hair transplant trichotillomania alopecia areata scarring alopecia frontal fibrosing alopecia bimatoprost “stick-and-place” method
Key Points
•Brow hair transplantation is challenging due to the angles, directions, location, and type of hair involved.
•In appropriate cases, choose hair that most closely matches that of the target brow hair (i.e., fine in caliber and single-hair follicular units).
•Grafts should be placed directionally and at as acute an angle as possible while minimizing trauma.
80.1 Why Brows are Important
Brow hair is important for several reasons. It helps shield the eyes from the sun and provides a visual frame to the eyes. It is also a target for several medical conditions that cause its loss including alopecia areata, trichotillomania, and hypothyroidism. A patient who has lost their brows may be as desperate as or even more desperate to regain them than others who have lost hair in other parts of their body. For this reason, special care with diagnosis and surgical planning must be taken with these patients.
80.2 Structure of the Normal Brow
Normal brows start medially approximately superior to the medial canthus of the eye. Brow hair in this area often projects superiorly as a low-profile “tuft,” and within the first centimeter begins to cant laterally. The remainder of the brow typically follows the brow ridge to point slightly beyond the lateral canthus of the eye. The topmost brow hair points both laterally and inferiorly, and plays the important role of establishing where the visual “arch” of the brow is located. Locations of the arch vary, and are often subject to the style of the day, but at least one aesthetic analysis (Fig. 80.1) places it at the lateral border of the iris.1 The bottom row of brow hairs point both laterally and superiorly, creating a slight herringbone appearance as they enmesh the superiorly based hairs. Hair in the middle of the brow flows laterally. All brow hair is angled only a few degrees off the surface of the skin (Table 80‑1).
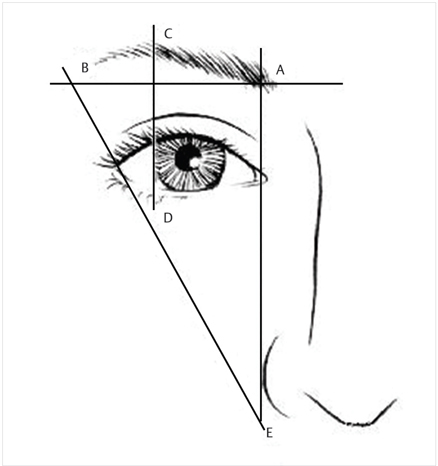
Fig. 80.1 Gunter–Antrobus aesthetic analysis.
Table 80.1 Structure of the normal brow
Brow location | Direction of hair |
Medial | Superior or canted slightly laterally |
Superior edge | Laterally and inferiorly |
Inferior edge | Laterally and superiorly |
Center | Laterally |
Brow hair itself is unique. Short and fine, these hairs usually arise from a single follicular unit with a tapered tip and mild curl. Such specific hair characteristics make choosing donor hair to match the delicate appearance of primary importance. Matching grafts can often be found in the supra-auricular and nape areas of scalp hair. Body hair would seem like a good match for transplantation into the brows, but is less desirable due to a long telogen phase.2
Musculature around the brow area can be complex. Muscles in and around the brows are often targets for Botox treatment, which can limit their tonic contractions and voluntary movement and change the shape of the brow in both desirable and undesirable ways. It is wise to avoid brow transplantation in the case of an unsatisfactory aesthetic appearance from botulinum toxin treatment—the preferable course of action being watchful waiting and adjustment of the botulinum toxin treatment itself. It can take over 4 months for the effects of the treatment to subside, so patients should be counseled accordingly.
Cutaneous innervation of the brow area is provided by the supraorbital and supratrochlear nerves. Interestingly, both nerves are targets for a supratrochlear forehead block during routine hair transplantation at the hairline, but they are not suitable for anesthesia during brow surgery since the most lateral part of the brow is in the territory of the zygomaticotemporal nerve. Retrograde paresthesias of all divisions of the trigeminal nerve (ophthalmic and maxillary, respectively) are not uncommon during a brow surgery.
80.3 Diagnosing Brow Hair Loss
The causes of brow hair loss (Table 80.2) are varied and often coexist.3 Due to the pathological complexity, and the fact that several of the diagnoses are characteristically occult (body dysmorphic disorder, trichotillomania, etc.), physicians should conduct a thorough initial patient consult for all brow cases.
Table 80.2 Differential diagnosis of brow hair loss
•Laser facial treatment (intense pulsed light, hair removal, etc.) |
•Alopecia areata |
•Scarring alopecias (lichen planopilaris, frontal fibrosing alopecia, etc.) |
•Hypothyroidism |
•Threading/plucking/waxing |
•Trichotillomania |
•Body dysmorphic disorder (BDD) |
•Senescent alopecia |
•Trauma (scarring or not) |
•Surgery (Mohs) |
•Tattooing (especially repeated) or tattoo removal |
A complete history should include roughly the same lab studies as would be required for diagnosing female pattern hair loss, particularly thyroid-stimulating hormone (TSH), T3, and T4 (especially with lateral brow loss), and erythrocyte sedimentation rate (ESR) for concomitant autoimmune conditions. The use of a trichotillomania and body dysmorphic questionnaire can help identify unsuitable patients.4 Any history of alopecia areata should raise caution and should be considered active until proven otherwise. All plucking, shaping, threading, waxing, dyeing, and trimming must be stopped 4 to 6 weeks before patient evaluation. “Urgent” brow transplant surgeries should be avoided.
Prior to examination, ask all patients to remove makeup. Globally examine the brows for evidence of native hair growth and observe overall scalp hair for evidence of occult trichotillomania, alopecia areata, psoriasis, etc. Patchy or one-sided growth is more likely to have an underlying medical cause than diffuse loss, but many nonsurgical conditions can mimic less concerning brow loss diagnoses. Microscopic examination of the brow hairs and skin is essential. Exclamation point hairs (alopecia areata), hairs in different stages of growth (trichotillomania), and loss of the follicular ostia (scarring alopecia) can all be clues to the cause of the brow loss.3
Concerns for alopecia areata and scarring alopecias, particularly frontal fibrosing alopecia (FFA), should prompt a biopsy. However, in the cases with clear dermoscopy evidence of either areata or FFA, the diagnosis may be clear enough and biopsy may not be necessary. Many patients will understandably resist the idea of a small scar in the brow area without hair to hide it, and thus making the surgery contingent upon a biopsy proven diagnosis may turn potential surgery patients away. However, the high rate of graft failure with these high-risk situations makes biopsy the preferable course of action.
Should a brow biopsy become necessary, it should consist of a small tapered ellipse in line with the brow, 4 to 6mm long, and contain both affected and unaffected areas for comparison. If possible, two samples should be taken, although the brows may lack a sufficient amount of suitable tissue. It is advisable that an experienced dermatopathologist with special interest in diagnosing hair disorders provide the histological interpretation.5
Devices that simultaneously magnify and digitally photograph are recommended since they allow a detailed discussion of any findings with the patient. This can illustrate the caliber of any remaining recipient area hair (Fig. 80.2a, b) and be used to visually compare different potential donor sites. It is useful to provide toothpicks to both the doctor and the patient in order to point to specific areas of concern as the consultation progresses.
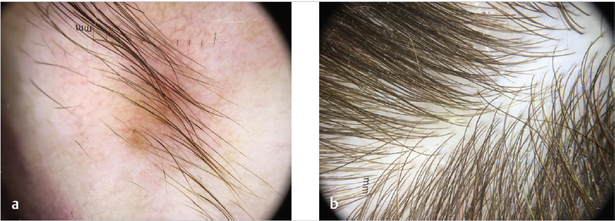
Fig. 80.2 (a) Thin brow hair in a patient seeking restoration. (b) Donor hair shows good color, texture, and caliber match.
80.4 Patient Selection
Experienced surgeons understand the importance of patient selection, and brow hair transplantation is no exception. Assuming active disease processes and mental health diagnoses have been ruled out, patients whose donor hair caliber most closely matches any remaining brow hair are the best candidates. Be prepared to turn away patients with a wide disparity between fine remaining brow hair and thick donor hair since the results will look “bristly” and unnatural (Fig. 80.3).

Fig. 80.3 Brows transplanted with mismatched hair caliber leading to a “bristly” appearance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








