Evidence-based medicine has become increasingly prominent in the climate of modern day healthcare. The practice of evidence-based medicine involves the integration of the best available evidence with clinical experience and expertise to help guide clinical decision-making. The essential tenets of evidence-based medicine can be applied to both functional and aesthetic rhinoplasty. Current outcome measures in functional and aesthetic rhinoplasty, including objective, subjective, and clinician-reported measures, is summarized and the current data is reviewed.
Key points
- •
Outcomes in rhinoplasty can be assessed by subjective, objective, and clinician-reported measures.
- •
Use of validated measures ensures reliability and consistency in outcomes reporting.
- •
Although most studies demonstrate near-universal support for the efficacy of functional and aesthetic rhinoplasty techniques, future studies should emphasize use of validated outcome measures when reporting data.
- •
Although level 1 evidence studies are currently rare in rhinoplasty literature, evidence-based medicine can be applied to rhinoplasty based on the wealth of data available from case reports, case series, cohort studies, experiments without controls, statements of expert opinion, and basic science research.
Introduction
The practice of evidence-based medicine has become increasingly prominent in the climate of modern day health care. The current pace of technologic innovation has led to the rapid development of novel medical therapies, each necessitating proof of efficacy, safety, and utility. Increasingly, physicians have come to consider evidence-based decision-making as the standard of care, a development that has been paralleled by matching expectations from patients. Far from replacing the traditional teachings of medicine, evidence-based medicine requires the integration of clinical experience and expertise in conjunction with the best available evidence and individual patient values and preferences.
The Oxford Center for Evidence-Base Medicine has developed one of the most widely recognized classifications systems for critically appraising the strength of clinical evidence. At the upper echelon of this 5-tiered schema are systematic reviews of randomized controlled trials (level 1 evidence), followed by comparison cohort studies (level 2), case-control studies (level 3 evidence), case series (level 4), and expert opinion and bench research (level 5). A common mistake is the assumption that higher levels of evidence invariably represent better evidence. This is particularly relevant to the surgical specialties because level 1 evidence data are rare given the inherent ethical concerns in randomizing patients into a placebo treatment (ie, sham surgery) group. Fortunately, although the prevalence of level 1 evidence data may be relatively limited in facial plastic and reconstructive surgery, advancement of knowledge may occur through alternative study designs, including cohort studies, experiments without controls, uncontested expert opinion, or basic scientific research. These types of studies have helped facial plastic surgeons navigate a world in which evidence-based medicine is not considered a luxury but, instead, the standard of care.
The term rhinoplasty when used broadly refers to surgery of the nose that is undertaken either to improve aesthetics, nasal function, or both. When the primary goal of surgery is to improve the appearance of the nose, this is typically specified as aesthetic or cosmetic rhinoplasty. When the primary goal of surgery is to improve nasal function by repair of an anatomic source of obstruction, it is referred to as functional rhinoplasty or nasal valve repair, with these terms often used interchangeably. The goal of this article is to provide a brief summary of current outcomes data regarding functional and aesthetic rhinoplasty surgery to help facilitate evidence-based clinical decision-making.
Introduction
The practice of evidence-based medicine has become increasingly prominent in the climate of modern day health care. The current pace of technologic innovation has led to the rapid development of novel medical therapies, each necessitating proof of efficacy, safety, and utility. Increasingly, physicians have come to consider evidence-based decision-making as the standard of care, a development that has been paralleled by matching expectations from patients. Far from replacing the traditional teachings of medicine, evidence-based medicine requires the integration of clinical experience and expertise in conjunction with the best available evidence and individual patient values and preferences.
The Oxford Center for Evidence-Base Medicine has developed one of the most widely recognized classifications systems for critically appraising the strength of clinical evidence. At the upper echelon of this 5-tiered schema are systematic reviews of randomized controlled trials (level 1 evidence), followed by comparison cohort studies (level 2), case-control studies (level 3 evidence), case series (level 4), and expert opinion and bench research (level 5). A common mistake is the assumption that higher levels of evidence invariably represent better evidence. This is particularly relevant to the surgical specialties because level 1 evidence data are rare given the inherent ethical concerns in randomizing patients into a placebo treatment (ie, sham surgery) group. Fortunately, although the prevalence of level 1 evidence data may be relatively limited in facial plastic and reconstructive surgery, advancement of knowledge may occur through alternative study designs, including cohort studies, experiments without controls, uncontested expert opinion, or basic scientific research. These types of studies have helped facial plastic surgeons navigate a world in which evidence-based medicine is not considered a luxury but, instead, the standard of care.
The term rhinoplasty when used broadly refers to surgery of the nose that is undertaken either to improve aesthetics, nasal function, or both. When the primary goal of surgery is to improve the appearance of the nose, this is typically specified as aesthetic or cosmetic rhinoplasty. When the primary goal of surgery is to improve nasal function by repair of an anatomic source of obstruction, it is referred to as functional rhinoplasty or nasal valve repair, with these terms often used interchangeably. The goal of this article is to provide a brief summary of current outcomes data regarding functional and aesthetic rhinoplasty surgery to help facilitate evidence-based clinical decision-making.
Functional rhinoplasty
Outcome Evaluation in Functional Rhinoplasty
Assessing clinical outcomes following functional rhinoplasty surgery has remained a highly controversial topic. It has long been recognized that significant incongruities can exist between a patient’s self-reported severity of nasal obstruction and objective measurements of nasal valve function. The nasal valve defines the area of the nasal passages with the smallest cross-sectional area and, therefore, the highest resistance to airflow. Traditionally, it is taught that the nasal valve has 2 components, internal and external, that can be involved with nasal valve compromise and nasal obstruction. The internal nasal valve is defined by the caudal edge of the upper lateral cartilages, the septum, and the anterior inferior turbinate. The angle formed between the upper lateral cartilage and the dorsal septum is critical for maintaining patency of the internal nasal valve, with the normative range being between 10° to 15°. The external nasal valve is defined by the nasal ala, caudal septum, the caudal aspect of the lower lateral cartilages, and nasal sill.
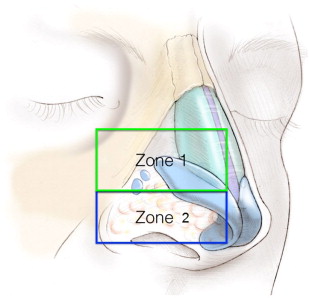
More recent nomenclature has taken into account the dynamic nature of nasal valve obstruction, using the term lateral wall insufficiency (LWI) to refer to the inspiratory collapse of the lateral wall. LWI can be further divided into 2 zones ( Fig. 1 ). Zone 1 is located more cephalad and corresponds to the scroll region and inferior upper lateral cartilage. Zone 2 is akin to the traditionally described external valve. It is located caudal to Zone 1 and corresponds to the skin and soft tissues of the nasal ala.
Generally, assessment of treatment efficacy and outcomes in functional rhinoplasty can be divided into 3 categories: objective measures of nasal function, patient-reported measures, and clinician-derived measures.
Objective anatomic measures
Objective measures can be further subcategorized as either anatomic (measuring structural dimensions) or physiologic (measuring functional or biological parameters). There is much debate regarding the value of objective measures in the assessment of nasal valve compromise and clinical nasal obstruction and, as such, these are used primarily for research purposes instead of for clinical decision-making.
Objective anatomic measures include acoustic rhinometry and radiographic studies assessing nasal cavity dimensions and geometry. Acoustic rhinometry is a diagnostic measure that uses acoustic reflections to calculate nasal airway cross-sectional area as a function of longitudinal distance along the nasal passageway. Nasal passage volumes can then be calculated from contiguous cross-sectional values. This allows for assessment of the dimension of the nasal airway at specific points along the nasal passage. Although its clinical applications are still debated, acoustic rhinometry has seen widespread adoption in clinical research with more than 500 studies published since the late 1980s. Importantly, acoustic rhinometry is a static measurement of nasal dimensions and, therefore, measurements may vary depending on the degree of current nasal congestion. It is, therefore, important to obtain measurements both before and after topical decongestion in order to distinguish between mucosal hypertrophy and true structural deformity.
High-resolution computed tomography (CT) can also be used to directly obtain anatomic measurements of the nasal dimensions instead of the indirect methods used by acoustic rhinometry. In a level 4 case series validating high-resolution CT against acoustic rhinometry, cross-sectional areas and nasal cavity volumes from each method showed significant correlation. Like acoustic rhinometry, it is a static measurement of nasal dimensions and is subject to physiologic variations in nasal mucosal congestion. One additional benefit of radiographic imaging studies is that the angle of the internal nasal valve can be measured. Because the angle of the internal nasal valve is known to play a critical role in nasal valve compromise, this provides additional diagnostic information that can be used in surgical decision making.
Objective physiologic measures
Physiologic measures include rhinomanometry and measurements of peak nasal inspiratory flow. Rhinomanometry is a dynamic diagnostic tool that measures transnasal pressure and nasal volume airflow to calculate nasal airway resistance during nasal inspiration. Generally, rhinomanometry can be differentiated into active and passive methods, with each of these being subdivided further into anterior and posterior techniques. In practice, the active anterior method is the most commonly used because it is the most physiologic technique. In the active anterior technique, the patient actively breathes through one nasal cavity while the transnasal pressure (the difference in pressure from the naris to the nasopharynx) is measured with a pressure probe in the contralateral nostril.
Nasal peak inspiratory flow is another noninvasive physiologic measure that measures the maximum airflow that the subject is able to produce during forced nasal inspiration. It is a reliable method of measuring nasal patency and has been validated against rhinomanometry as well as other objective measures of nasal patency. One significant drawback of this measure is that it includes several potentially confounding factors, including effort dependence and pulmonary function.
Patient-reported outcome measures
In contrast to objective measures, patient-reported outcome measures focus on evaluating the subjective experience of the patient and their self-reported assessment of the efficacy of a given treatment. These measures focus on quality-of-life (QOL) issues and provide a quantitative assessment of otherwise subjective results. Because the primary goal of functional rhinoplasty surgery is to improve nasal obstructive symptoms, QOL measures have been commonly used to evaluate efficacy of surgery. Disease-specific measures are most useful for this because the health status changes from nasal surgery may be too subtle to be appreciated by global instruments. The visual analog scale (VAS) has been one of the most commonly used disease-specific patient-reported tools for assessing nasal function. Patients indicate the severity of nasal obstruction on a linear scale ranging from no obstruction to complete obstruction. More recently, the Nasal Obstruction Symptom Evaluation (NOSE) scale has come into widespread use. Although numerous other scales had been previously described, including the Chronic Sinusitis Survey and the Sino-Nasal Outcome Tool, the NOSE scale is a disease-specific QOL measure that specifically targets issues related to nasal obstruction instead of inflammatory disease. The NOSE scale has been validated as a reliable and responsive measure of QOL issues related to nasal obstruction. The importance of using a validated QOL scale cannot be understated because this allows for consistency in reporting of outcomes.
Clinician-derived measures
Clinician-derived measures are standardized grading scales used after surgery to assess outcomes based on quantifiable physical examination or clinical findings as assessed by the clinician. These are potentially powerful outcome measures that are currently infrequently used. A recently described methodology for description of LWI has been adopted at the authors’ institution and several others. In this system, each zone of the lateral wall is individually evaluated for collapse and rated 0 to 3. This measure of LWI has been validated and its use in reporting outcomes of nasal procedures is burgeoning. Another recent level 2c study described a clinician-derived measure involving a rating of the size of the anterior inferior turbinates. In this grading scale, inferior turbinate was graded on a scale of 1 to 4 based on the space occupied by the anterior aspect of the inferior turbinate relative to the total space available at the same anteroposterior location in the nasal cavity. Grade 1 inferior turbinate occupies 0% to 25% of the total airway space, grade 2 occupies 26% to 50%, and so forth.
Recently, a severity classification system has been developed to provide a clinical context to patient-reported NOSE scores. NOSE scores were obtained from 345 patients with and without nasal obstructive symptoms. Using receiver operating characteristic curve analysis, NOSE scores were categorized as being mild (range 5–25), moderate (range 30–50), severe (range 55–75), or extreme (range 80–100). This allowed the addition of a clinician-derived report of outcomes to provide context to the subjective patient-reported NOSE scores.
Discordance of objective and subjective outcome measures
One of the most significant criticisms of objective measures of nasal patency and airflow as an indicator of treatment success is that there seems to be a poor correlation between these objective findings and patient-reported obstructive symptoms. Interestingly, nasal sensation of airflow seems to play a critical, though not yet fully understood, role in subjective nasal obstruction.
In one of the most comprehensive studies to date addressing this topic, Lam and colleagues performed a prospective cross-sectional study of 290 subjects evaluating nasal dimensions and function via acoustic rhinometry and nasal peak inspiratory flow, correlating these findings with a subjective measure of nasal obstruction (VAS). Their investigation demonstrated no significant correlation between any of the anatomic, physiologic, and subjective categories of nasal measures (level 4 evidence). In a contrasting level 4 study, Kjaergaard and colleagues compared acoustic rhinometry and nasal peak inspiratory flow results with VAS scores in 2523 subjects. Their investigation yielded findings disparate to the Lam and colleagues study, with highly significant associations demonstrated between the subjective sensation of nasal obstruction and corresponding measures for nasal cavity volume, area, and airflow. In a recent systematic review of 21 studies published on this topic, equivocal data were demonstrated (level 2 evidence). There seemed to be greater correlation between objective and subjective measures when symptomatic nasal obstruction was present. In the absence of nasal symptoms, however, correlation between subjective and objective measures was poor. Clearly, the data are currently inconclusive regarding the clinical value of objective measures. Because many factors may play a role in the subjective sensation of nasal obstruction, it is likely that no single objective test, albeit qualitatively and technically reliable, will reproducibly correlate with this perception.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




