55A Evaluation, Planning, and Donor Concerns with Follicular Unit Excision
Summary
Keywords: follicular unit excision hair angle safe donor harvesting zone transections FUE scars donor area donor depletion
Key Points
•It is imperative that the surgeon understand the limits of the donor area in terms of graft numbers and safe zone.
•Hair direction often differs from that at the surface compared to the course within the skin. To avoid transections, the surgeon must be aware of these possible angle changes.
•Scars are created with follicular unit excision (FUE) and excessive harvesting may limit the ability of the patient to wear his or her hair extremely short.
55A.1 Introduction
Follicular unit excision (FUE) refers to the harvesting of individual follicular units (FUs) from the donor area by means of a punch.1 FUE has grown in popularity for harvesting as patients have become increasingly concerned about the linear donor scar that results from strip harvesting. The scars from strip harvesting can be excellent and the ability to conceal the scars is usually simple, but some patients are nevertheless worried about possible evidence of the strip procedure.
The current hairstyles, featuring short hair and even shaved scalps, have further motivated patients seeking hair replacement to consider the FUE procedure. Also, surgeons recognize that FUE may be particularly appropriate for young patients who are uncertain as to whether they want to commit to future hair transplant surgeries if their balding progresses. In addition, there are patients who have undergone strip harvesting, but a subsequent lack of mobility of the scalp prohibits doing further strip harvesting. For these patients, FUE may be the only means to obtain more grafts.
Understanding the judicious use of hair in the donor area is crucial to obtaining overall excellent results with FUE. In this chapter, we review various considerations for the donor area when undertaking FUE (Video 55A.1).
55A.2 Evaluation of the Donor Area
As with the donor evaluation for strip harvesting, the surgeon should consider the patient’s age, possible future hair loss, gender, ethnicity, family history, medical and surgical history, and scalp health. The physician must also consider hair color, caliber, curl/wave, scalp laxity, skin texture, density of FUs, types of FUs, and the extent of miniaturization if present. The physician ought to be particularly cautious in proceeding with surgery if there is evidence of scalp disease, DUPA, or general thinness of the hair in the donor areas as harvesting could create an even thinner appearance.
Skin characteristics can have a major influence on sharp motorized FUE results. Skin can be hard, rubbery, and difficult to penetrate versus soft, nonrubbery, and easy to penetrate. If the skin is too hard, it dulls a sharp punch or causes slide. If it is too soft or mushy, it is susceptible to torsion forces. Skin can also be flexible or loose, allowing for a lot of movement when subjected to external force, versus firm or stiff, allowing for less movement
The degree of curl is important to assess as patients who possess hair with a severe curl may experience increased transection of hair follicles upon harvesting.
It is important to assess the hair exit angle and determine how to manage the changes in angles that may occur as one harvests grafts in the mid-occipital area versus the lateral areas. In general, the hair exits more acutely at the sides and toward the nape. As the exit angle is usually different than the angle within the skin,2 it may be helpful to obtain test grafts prior to the actual surgery to determine these changes and assess follicular length as well as the depth of the follicles. Obtaining test grafts may be especially helpful when considering FUE for patients with extremely curly hair.
Whether for FUE or strip harvesting, examination of the hair can be facilitated with the use of a magnification device. Such devices can be quite simple such as a handheld mobile phone with camera lens or a dermatoscopic or a more sophisticated device exemplified by the Folliscope (Anagen Corp, Seoul, Korea) or Follisys (HTI, Nicosia, Cyprus) machine or Canfield system (Canfield Scientific, Parsippany, New Jersey, United States). By using these devices, the surgeon can better evaluate the hair characteristics including follicular density, average hair/FUs, hair density, hair exit angles, and caliber.
In planning larger cases, the surgeon might want to consider what he or she can endure in terms of harvesting time and ergonomic stress. This will differ depending on the surgeon’s skill and experience. Likewise, it is important to be aware of the patient’s endurance and general attitude. A fidgety, restless patient can make harvesting difficult and very prolonged.
During the evaluation, it may be reasonable to examine or at least discuss alternative sites of donor harvesting such as body hair3 and beard hair. The patient needs to be advised that there are differences in the caliber and growth of these alternate sources of hair as compared to scalp hair.
In observing the follicular groupings, the surgeon should be considering what size punches might be utilized. If the grouping is tight, a smaller punch may be used and similarly if the FUs are wide, a slightly larger punch might be appropriate. In general, most try and use the smallest punch that does not increase the degree of transection. Testing different punch types and depth of incision at the beginning of surgery helps determine this. The size that can be used will differ with surgeon skill and type of punch and system used.
As part of the consultation and examination of the donor area, the surgeon ought to convey to the patient that although FUE does not create a linear scar, it is not a scarless procedure or without risk. The wounds created by the punch have the potential to leave round scars that can be hypopigmented. Additionally, overaggressive harvesting can thin out the donor area, making it unsightly. Thus, the patient needs to be advised that there is a limit to graft numbers with FUE as there is with strip harvesting.
The patient should also be informed that in most instances the donor area must be trimmed to a very short length (1–2 mm) or shaved to perform the procedure. This drastic change in look can be a problem for some patients. Some physicians try to get around this issue by keeping the donor hair long and only harvesting small linear or rectangular patches of donor area. The longer hair can cover these patches until the shaved hair regrows. This approach does have the risk of creating a noticeable window effect when higher-density unharvested hair is adjacent to a lower-density FUE harvested area. Recently, nonshaven techniques, as described in Chapter 72, have been developed; however, they are more difficult, take longer, and less grafts can be obtained per procedure.
Determining the safe number that can be harvested per surgery as well as over the lifetime of a patient is a key skill needed for FUE surgery. There is still controversy about what these numbers are in different patients. It is obvious the number will change depending on the patient’s age, starting donor supply and hair characteristics. Many experienced FUE physicians feel it is generally safe, in the average patient, to harvest at least a lifetime total of 5,000 to 6,000 grafts in two sessions. It is the ability to predict those patients who can have larger numbers of grafts harvested (per session and over their lifetime) that is still controversial and needs to be refined. Just like with FUT surgery, we have seen examples of great results with larger FUE sessions (>8,000 grafts) as well as terrible disasters. Perhaps more objective donor supply measuring techniques, like coverage value (CV), may help more accurately predict what can be harvested in different patients. However, the effect of hair loss progression has consistently surprised us in the field of hair transplantation. It will take time, careful observation, and caution before we can consistently predict the safe donor supply in all patients. The concept of using both FUT and FUE to maximize the total donor supply that can be harvested over the life of patients without pushing either technique to the extreme has been proposed as one method to more safely achieve higher numbers in those that need it.
55A.3 Surgical Planning for Harvesting
The surgeon will use all the information gained from the donor evaluation to plan the donor harvesting strategy.
A key consideration in planning is an understanding of the “safe donor area” for harvesting.4,5 This zone represents the area of donor scalp that the surgeon can be confident obtaining grafts from, ensuring that these grafts will not be subject to androgenetic alopecia in the future. Dr. Unger has noted that perhaps a better descriptive terminology for this zone is the “safest zone” or “relative” safe zone. The reason for this specificity is that we now know that hair within this zone hair can, to a small degree, miniaturize and be lost over time as well. However, the loss in the safest zone is to a much lesser degree than the hair outside this zone, which can and often is lost completely (Video 55A.2).
Apart from the concept of the safe zone, it is interesting to note that it is within this zone, at the horizontal midline, that the best terminal hair generally exists for transplantation. The surgeon may want to assess this area to ascertain how much hair can be safely obtained from this “subzone” without creating thinness. The surgeon should be cognizant of the need to try to randomize the harvesting to avoid creating a patterned or overharvested appearance of the donor hair that could be perceptible to the patient or an observer.
Careful examination of the safe zone area is of utmost concern when considering hair transplant surgery in young patients. When examining young patients, it may not be clear as to how they will progress in the balding process during their lifetime. Erring on the conservative side of harvesting with these patients is generally advised.
Historically many physicians have relied on the “safe zone” areas as described by Alt and Unger.5 Their calculations were made with follicular unit transplantation (FUT/strip harvesting) or punch harvesting in mind. More recently, Cole6,7 has advocated a safe zone area for FUE harvesting that is larger than that described by Alt and Unger. Some surgeons have also sought to discern the extent of the safe area by examining the donor area for hair miniaturization. Seeing hair miniaturization superiorly in the occipital and temporal areas can indicate that hairs in these areas are already destined to be lost due to androgenetic alopecia. Sometimes wetting the hair in the donor can expose portions of thinning hair and the extent of future hair loss.
As a practical example of determining the area of the safe zone, using Unger’s measurements and borders and assuming a length from ear to hear of approximately 30 cm (author’s measurement), the surface area would amount to about 165 cm2. Using Cole’s methodology, he observed an average surface area of approximately 200 cm2. These surface area numbers could vary markedly based on head size and apparent density.
FU density varies widely. Densities as low as 50 or so FUs to over 100 FUs/cm2 are reported. The average density is believed to be in the range of 60 to 80 for most Caucasians. Using an average density of 70 FU/cm2 (normal density reported as 60–80),8 the number of FUs present would amount to almost 12,000 with Unger’s measurement and 14,000 with Cole’s safe zone.
It is stated that 50% of hairs can be taken from an area before thinning is obvious. If this is true, then one could theoretically remove 6,000 to 7,000 FUs from the safe zone depending on the safe zone boundaries utilized. The figure of 50% is based on the work by Merritt in which he plucked hairs.8 Dr. Merritt did not indicate what length the remaining hair was at when the study was done. For a shaved head or short hair, the percentage of hair that can be removed before a lowered density would be observed might be altered downward from 50%.
Again, such numbers could have a wide range of values as FU densities vary markedly and hair characteristics such as caliber and curl could also affect perceived density.
Other prominent hair restoration surgeons have voiced opinions on the amount of FUs that can safely be taken in patients. Rassman has related that he believes that 5,000 grafts9 are very reasonable and Shapiro (personal communication) believes that most patients can obtain 5,000 to 6,000 grafts.
As a personal note, the author has observed that many patients who seek hair transplants in later life have donor areas where the occipital border superiorly is significantly less than the measurement by Unger and Cole and similarly lateral borders that are less than that typically described for the donor safe zone.
Another way to look at the effects of FUE harvesting on the donor area is to observe the initial densities of the donor area centrally and at the lateral aspects. Examining density photographs from the donor area of various patients, it is apparent that the surgeon can obtain from a “virgin” scalp approximately one-seventh or so of the available FUs before the surgeon would harvest two adjacent FUs (Fig. 55A.1). This amounts to approximately 14% of the total grafts available in the area. Assuming a donor area of 12,000 to 14,000 grafts, this amounts to almost 1,700 grafts. If we use the number 14,000, the result is almost 2,000 grafts.
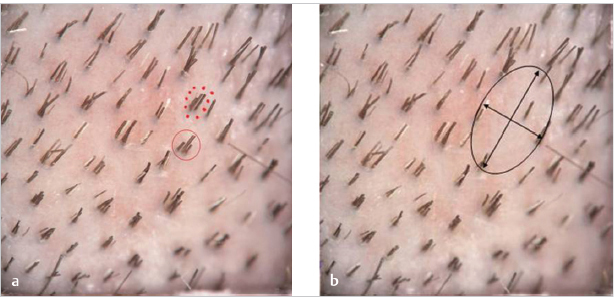
Fig. 55A.1 (a) Photograph of follicular units (FUs) demonstrating possible choices for removal of neighboring grafts without causing adjacent FU voids (solid red circle is a typical FU). In a virgin scalp, this is usually one-seventh or one-eighth of the original number of grafts. (b) If an adjacent FU is removed (dotted circle), a significant area of hairless skin remains.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







