74
Environmental and Sports-Related Skin Diseases
Cutaneous Injury Due to Heat Exposure
Thermal Burns
• Traumatic injury to the skin caused by an external heat source.
• The burn depth determines the severity and classification of the injury, its potential for healing and need for surgical intervention (Table 74.1).
Table 74.1
Classification and treatment of thermal burns.
Based on the 2009 American Burn Association revised classification system for burns. http://www.ameriburn.org/Chapter14.pdf
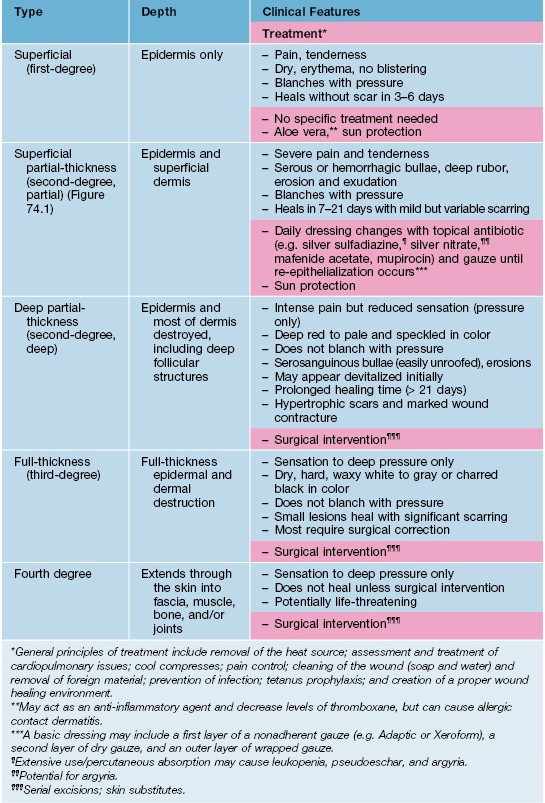
• In 2009, the American Burn Association replaced the traditional classification of burn wounds (i.e. first-, second-, third-degree) with a system that reflects the need for surgical intervention (see Table 74.1; Fig. 74.1).
• The most accurate method for estimating BSA involvement in adults and children is the Lund–Browder chart (http://www.tg.org.au/etg_demo/phone/etg-lund-and-browder.pdf); the ‘rule of nines’ method is perhaps more expeditious in adults, but it cannot be used for children (Fig. 74.2).
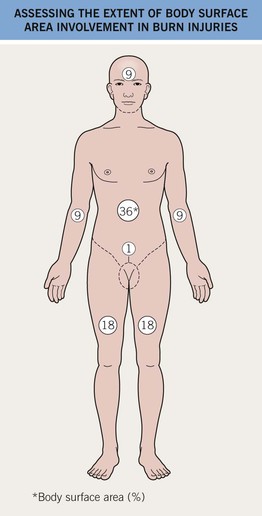
Fig. 74.2 Assessing the extent of body surface area involvement in burn injuries: Rule of nines. In adults, an estimate of burn extent is often based on this surface area distribution chart. Infants and children have a relatively increased head : trunk surface area ratio and this chart is ineffective for them. These estimates are also used for primary cutaneous disorders. The most accurate method of estimating the BSA involvement of burn injury in adults and children is with the Lund–Browder chart (http://www.tg.org.au/etg_demo/phone/etg-lund-and-browder.pdf).
• General principles of treatment are outlined in Table 74.1.
Erythema Ab Igne
• Multiple heat sources have been implicated (Table 74.2).
Table 74.2
Heat sources reported to cause erythema ab igne.
| • Heating pads | • Steam radiators |
| • Hot water bottles | • Heated car seats |
| • Electric stove/heater | • Heated reclining chairs |
| • Open fires | • Heating blanket |
| • Coal stoves | • Hot bricks |
| • Peat fires | • Infrared lamps |
| • Wood stoves | • Microwave popcorn |
| • Sauna belt | • Laptop computer* |
* Anterior thighs >> abdomen.
Courtesy, Mary Beth Cole, MD, and Michael Smith, MD.
• Early lesions: asymptomatic, initially transient, blanchable macular erythema in a broad, reticulated pattern that corresponds to the venous plexus; size and shape approximates that of the heat source (Fig. 74.3A).
• Later lesions: dusky reticulated hyperpigmentation; lesions are fixed and no longer blanchable (Fig. 74.3B).
• End stage: may become keratotic and bullae may appear.
• Rx: remove the heat source; if applicable, identify and treat the underlying source of pain.
Burns Associated with MRI and Fluoroscopy
Fluoroscopy
• This radiodermatitis may be acute, but with time continued changes can develop, e.g. hair loss, desquamation, permanent erythema, and ulceration (Fig. 74.4).
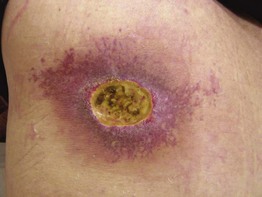
Fig. 74.4 Fluoroscopy-induced radiation dermatitis. The left upper back is a characteristic location for patients who have undergone attempts at coronary artery revascularization (e.g. angioplasty, stent placement). Courtesy, Jeffrey Callen, MD.
Cutaneous Injury Due to Cold Exposure
Frostbite
• Can occur when the skin temperature drops below about –2°C (28°F).
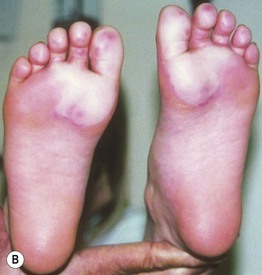
• There are four categories of severity based on depth of tissue injury; these are only recognizable upon rewarming (Fig. 74.5).