■ When considering EPLA, the adenoma must be solitary and clearly localized by preoperative imaging studies. Whether preoperative localizations techniques can rule out MGD with sufficient accuracy is questionable. Therefore, as with other minimally invasive techniques, the risk of missing MGD justifies the use of a quick intraoperative parathormone assay (QPTH).6 The less definitive the localizations studies, the more imperative the need for QPTH.
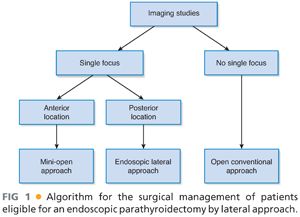
■ When patients are selected on the basis of the abovementioned criteria, no more than 50% of patients are eligible for this procedure (FIG 1).
■ EPLA is technically more challenging than standard cervical exploration and its performance should be confined to tertiary centers. The surgeon must be experienced in conventional parathyroid surgery. Mentoring by a surgeon who has experience with endoscopic neck procedures is also recommended.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Only noninvasive tests should be considered. When these tests are negative, EPLA is not indicated and the traditional open cervicotomy is preferable. The topographic diagnosis should ideally be established by convergence of the results of two different investigations, one providing good anatomic information and the other providing functional information.
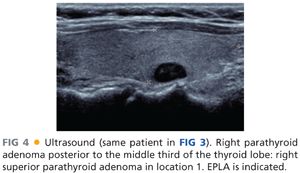
■ High-resolution ultrasonography (US) and technetium-99m (Tc-99m) sestamibi scan are used most commonly in combination.7 US can only assess the cervical region but gives good anatomic information, including useful information about the thyroid gland. The patient should be examined in the supine position with the neck in hyperextension. A pillow can be placed under the shoulders if the patient has a short neck. A high-frequency linear transducer (7.5 to 10 MHz) is used to obtain optimal depth penetration of 3 to 4 cm. A bilateral and comparative scan should be performed in transverse section, then in longitudinal section. In transverse section, the examination concentrates on an area defined by the longus colli muscles posteriorly, the thyroid gland anteriorly, the trachea medially, and the carotid artery laterally. The scan is then performed in cranial and caudal directions. An additional scan can be performed with the head of the patient turned away to the side and during deglutition to optimize the lateroesophageal images. The anterosuperior mediastinum is examined by inclining the transducer deeply in a retrosternal direction. The examiner should note the precise location with respect to surrounding structures, particularly to the thyroid gland, and the depth from the skin. Finally, a color flow Doppler or a power flow Doppler will be performed to test the vascularization of the area and define the artery branches involved.
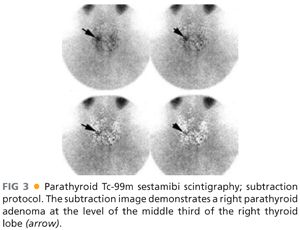
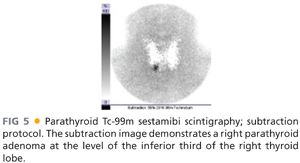
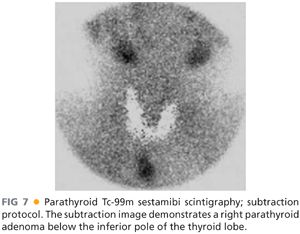
■ Two protocols for sestamibi scanning can be used: the single isotope dual phase protocol and the substraction protocol. The dual protocol requires early (15 minutes postinjection) and delayed images (at 1 and 2 to 3 hours, depending on thyroid washout). In cases of multinodular thyroid disease, additional further delayed images are sometimes needed. When a subtraction protocol is used, Tc-99m sestamibi is used in conjunction with another radionuclide specific to the thyroid. Tc-99m pertechnetate and 123I are the most widely used radioisotopes for thyroid scintigraphy. The main advantage of using 123I is that thyroid and parathyroid images can be acquired simultaneously in a dual energy window setup. The disadvantage is the cost of the protocol related to 123I. Parathyroid scintigraphy should include views of the neck and the mediastinum. Single-photon emission computed tomography (SPECT) can be helpful for more precise localization of adenomas, as it provides simultaneous three-dimensional (3-D) information on both neck and superior mediastinum.
■ Instead of US and Tc-99m sestamibi scan, four-dimensional computed tomography (4D-CT)8 or the use of computed axial tomography-methoxyisobutyl isonitrile (MIBI) image fusion,9 when available, may be preferable.
■ Consideration for EPLA depends on the results of preoperative imaging. EPLA should be strongly considered when the parathyroid adenoma is in close proximity to the recurrent laryngeal nerve, as the nerve is at risk during MIP. Therefore, EPLA is the procedure of choice in all cases where the parathyroid adenomas are deeply located in the neck.
■ Three locations of parathyroid adenomas with regard to the recurrent laryngeal nerve can be described (FIG 2).4 Location 1 is posterior to the two superior thirds of the thyroid lobe (FIGS 3 and 4). These adenomas are superior glands. Location 2 is at the level of or below the inferior pole of the thyroid lobe but in a plane posterior to it (FIGS 5 and 6). These adenomas may be either a superior gland that has migrated posteriorly and in a downward direction or an inferior gland that has fallen posteriorly. These glands can also migrate into the superior and posterior mediastinum. Location 3 is at the level of or below the inferior pole of the thyroid lobe but in a superficial plane (FIGS 7 and 8). These adenomas are always inferior glands and can be found in close contact with the tip of the inferior pole of the thyroid lobe but also along the thyrothymic ligament or into the superior pole of the thymus.
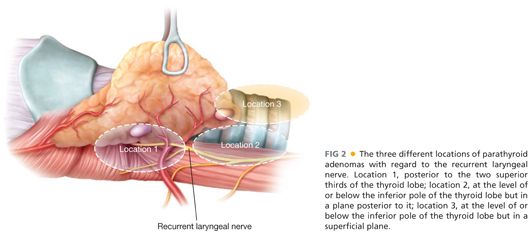
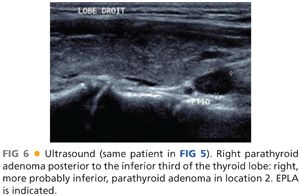
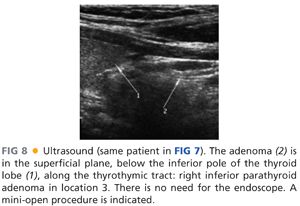
■ Adenomas in locations 1 and 2 are deeply located and are in the vicinity of the recurrent laryngeal nerve. The nerve is at risk and its clear identification during the procedure is recommended. The lateral view, provided by EPLA, permits its easy identification and allows a secure dissection. On the other hand, adenomas in location 3 are at distance from the nerve, which runs more deeply. Its identification is not essential. An anterior mini-open approach without the help of the endoscope is indicated.
■ In conclusion, the need to know preoperatively when the nerve is at risk reinforces the role of preoperative imaging studies. Depending on whether the patient has a deep-seated adenoma or a superficial-seated adenoma, the surgeon can choose between EPLA and an anterior mini-open approach.
■ The main interest of using an endoscope is not that one can perform a parathyroidectomy through a small incision but that one can perform a safe parathyroidectomy through a small incision.
SURGICAL MANAGEMENT
Preoperative Planning
■ Prior to surgery, the patient undergoes a vocal cord check.
■ The procedure is performed under general anesthesia with endotracheal intubation. Trocars are poorly tolerated by patients under local or regional anesthesia. In addition, swallowing and spontaneous breathing present impediments when dissecting in a small operative space.
■ The surgical instruments required include a 10-mm trocar, which will accommodate a 0-degree fiberoptic endoscope, and two 3-mm trocars, which will receive a series of purpose-made instruments (Medtronic Xomed, MicroFrance) including blunt-tipped dissectors, graspers, scissors, a diathermy hook, and an aspiration canula. These instruments measure 25 cm in length (FIG 9).

■ In patients presenting with small parathyroid adenomas less than 2 cm in diameter, a 5-mm trocar and a 5-mm 0-degree endoscope can be used.
■ QPTH assays are performed before and at the time of incision, directly before parathyroid excision and, subsequently, 5 and 15 minutes after parathyroid excision. Parathyroidectomy is considered successful when QPTH value falls by greater than 50% with respect to the highest preexcision level and into normal range (10 to 65 pg/mL).5
■ The surgical team consists of the operator, first assistant, and a scrub nurse. The surgeon and first assistant stand on the side of the diseased gland, with the scrub nurse facing them. The monitor is placed next to the scrub nurse and directly in front of the surgeon (FIG 10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








