9 Endoscopic Evaluation of the Lower Urinary Tract
HISTORICAL PERSPECTIVE
Kelly’s (1894) principal innovation in cystoscopy was developing a technique that provided adequate bladder distention. The Kelly cystoscope, a hollow tube without a lens, was not innovative, but his technique was. The cystoscope was introduced using an obturator, with the patient in knee-chest position. The negative intra-abdominal pressure created by this position allowed air to distend the bladder when the cystoscope was introduced. A head mirror was used to reflect an electric light into the bladder for illumination. The technique was simple but provided an excellent view. Its simplicity dramatically enhanced the accessibility of cystoscopy to all physicians. Kelly’s fame as a genitourinary surgeon, and as the founder of the Johns Hopkins Hospital residency training program in gynecology, the first in the nation, established cystoscopy as a gynecologic technique.
The twentieth century provided many innovations in the cystoscope. Hopkins and Kopany (1954) introduced both a fiber-optic telescope and, later, a rod lens system, which dramatically improved light transmission and resolution. This rod lens design is the system used in today’s rigid cystoscopes. Replacement of the air chamber with a series of glass rods with optically finished ends, separated by intervening air spaces, provides a wider viewing field and permits a change in the viewing angle. The innovation of angled telescopes improved the extent of visualization and facilitated more invasive procedures. Increasingly complex instruments were developed to perform operative procedures through a cystoscope, and, gradually, general surgeons developed the subspecialty of urology around this new technology. The development of the subspecialty of urology coincided with changes in gynecology. The combination of gynecology and obstetrics into a single training program deemphasized cystoscopy in gynecologic training, and gynecologists gradually became less skilled in the technique, whereas urologists continued to develop it.
The most recent development in cystoscopy is the flexible cystoscope. A flexible cystoscope takes advantage of the flexibility of the fiber-optic lens system to create a cystoscope that bends, thereby increasing the range of the field of view. Some authors report an improved view of the bladder neck using a flexible fiber cystoscope, whereas others advocate flexible cystoscopy to limit the necessary instrumentation and improve patient tolerance.
Robertson (1973), the father of urogynecology, reintroduced cystoscopy to gynecology with the development of the Robertson urethroscope. He addressed the deficiencies of the cystoscope for viewing the urethra by applying the rods lens technology of the Hopkins cystoscope to a shorter straight-on telescope with a nonfenestrated sheath designed specifically for viewing the urethra. He subsequently outlined a technique—dynamic urethroscopy—for evaluating incontinent women using the Robertson urethroscope. Dynamic urethroscopy offered a simple office procedure that considerably improved the diagnostic evaluation of the lower urinary tract over the alternatives of the time.
INDICATIONS
The general agreement is that cystoscopy is indicated for patients complaining of persistent incontinence or voiding symptoms following incontinence surgery, but less agreement exists about the role of cystoscopy in the baseline evaluation of patients with urinary incontinence. The refinement of urodynamic evaluation over the last three decades has demonstrated the superiority of this modality for diagnosing the common causes of urinary incontinence, such as urodynamic stress incontinence and detrusor overactivity. However, although urodynamic testing excels at providing an objective assessment of lower urinary tract function, it provides little information about lower urinary tract anatomy. Cystourethroscopy contributes an anatomic assessment of the urethra and bladder that is not achieved by urodynamic tests alone. Anatomic abnormalities, such as urethral diverticula, urogenital fistulas, and intravesical foreign bodies causing detrusor overactivity, might be suspected based on history or urodynamic tests but require an anatomic assessment for confirmation. Cystourethroscopy can also reveal unsuspected neoplasia in the incontinent patient. However, in women with stress incontinence, bladder lesions are found in only about 1% of patients. The Clinical Practice Guidelines of the Agency for Health Care Policy and Research in 1996 noted that the evidence does not support the routine use of cystoscopy in the evaluation of women with simple symptoms of incontinence (Fantl et al., 1996).
INSTRUMENTATION
Rigid Cystoscopy
The three components of the rigid cystoscope include the telescope, the bridge, and the sheath (Fig. 9-1). Each component serves a different function and is available with various options to facilitate its role under different circumstances.
The telescope transmits light to the bladder cavity and an image to the viewer. Telescopes designed for cystoscopy are available with several viewing angles, including 0-degree (straight), 30-degree (forward-oblique), 70-degree (lateral), and 120-degree (retro view). The different angles facilitate the inspection of the entire bladder wall. Although the zero-degree lens is ideal for adequate urethroscopy, it is insufficient for cystoscopy. The 30-degree lens provides the best view of the bladder base and posterior wall, and the 70-degree lens permits inspection of the anterior and lateral walls. The retro view of the 120-degree lens is not usually necessary for cystoscopy of the female bladder but can be useful for evaluating the urethral opening into the bladder. For many applications, a single telescope is preferable. In diagnostic cystoscopy, the 30-degree telescope is usually sufficient, although a 70-degree telescope may be required in the presence of elevation of the UVJ. For operative cystoscopy, the 70-degree telescope is preferable. The angled telescopes have a field marker, visible as a blackened notch at the outside of the visual field opposite the angle of deflection, that helps facilitate orientation.
The bridge serves as a connector between the telescope and sheath and forms a watertight seal with both. It may also have one or two ports for introduction of instruments into the irrigation-working channel. The Albarran bridge is a variation that has a deflector mechanism at the end of an inner sheath (Fig. 9-2). When placed in the cystoscope sheath, the deflector mechanism is located at the distal end of the inner sheath within the fenestra of the outer sheath. In this location, elevation of the deflector mechanism assists the manipulation of instruments within the field of view.
Rigid Urethroscopy
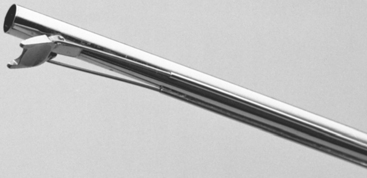
The rigid urethroscope is a modification of the cystoscope designed exclusively for evaluation of the urethra (Fig. 9-3). Because it is primarily a diagnostic instrument, it does not have a bridge. The telescope is shorter and has a 0-degree viewing angle, which provides a circumferential view of the urethral lumen as the mucosa in front of the urethroscope is distended by the distention medium. The 0-degree lens is essential for adequate urethroscopy.
Flexible Cystoscopy
Many urologists prefer the flexible cystoscope because of improved patient comfort, but this applies primarily to male patients. The absence of a prostate and the short length of the female urethra make rigid cystoscopy well tolerated by women. This may offset any perceived advantage of flexible cystoscopy in female patients. Moreover, several disadvantages exist with the flexible cystoscope. The flow rate of the irrigation-working channel is approximately one fourth that of a similar-sized rigid cystoscope and is further curtailed by passage of instruments down the channel. Some tip deflection is also lost with use of the instrument channel. In addition, because the view afforded by the flexible cystoscope is not as clear as that of a rigid cystoscope, greater operator skill is required to completely visualize the vesical cavity. No difference is present in the post-procedural morbidity as compared with rigid cystourethroscopy.