This article describes how dynamic infrared thermography (DIRT) can be used in autologous breast reconstruction with a deep inferior epigastric perforator flap. This noninvasive and noncontact technique for indirect monitoring of skin blood perfusion can be used in the preoperative planning and intraoperative evaluation of flap perfusion, as well as the postoperative monitoring of perfusion dynamics of DIEP flaps. DIRT provides valuable information on the perfusion physiology of perforators.
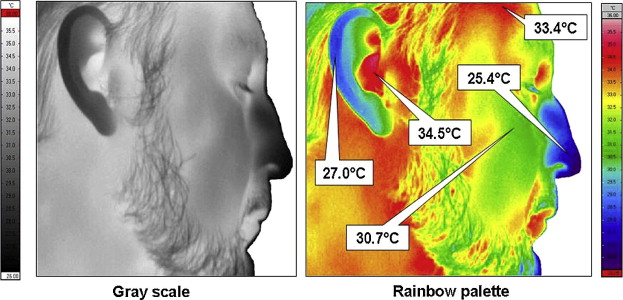
Humans are homeotherms, meaning that they are capable of maintaining a constant temperature that is different from that of the surroundings. This is achieved by keeping a fine balance between heat production and heat loss. The necessary heat to keep this constant temperature is generated by metabolism and muscle contraction. Heat is transported through the body with blood acting as the heat transfer medium. The skin plays an important role in the body’s temperature regulation. Heat loss to the surroundings is possible by conduction, convection, evaporation, and radiation ( Fig. 1 ). Under stable ambient conditions of 18°C to 25°C, the principal mechanism to achieve equilibrium between the body and the environment is by radiative heat loss from the skin to the environment. This radiative heat loss takes place in the form of infrared (IR) radiation.
Skin temperature has been used for centuries as an indicator of the physiologic condition and as an indication of possible pathology. There is a defined relationship between the skin temperature and the emitted infrared (IR) radiation from the skin surface. In medical IR thermography, images are produced of a patient’s surface temperature based on the IR radiation from the skin. Studies in humans have shown that there is a good correlation between skin perfusion and skin temperature. Measurement of skin temperature can therefore provide indirect information on skin perfusion.
The first report on the clinical use of IR thermography as a diagnostic aid came in 1956 when Lawson discovered that the skin temperature over a cancer in a breast was higher than that of normal tissue. He also showed that the venous blood draining the cancer is often warmer than its arterial supply. From then on there has been interest in the clinical use of IR thermography. The technique does not entail the use of ionizing radiation, venous infusion, or invasive procedures. In addition, the technique is easy to perform and images are relatively easy to interpret.
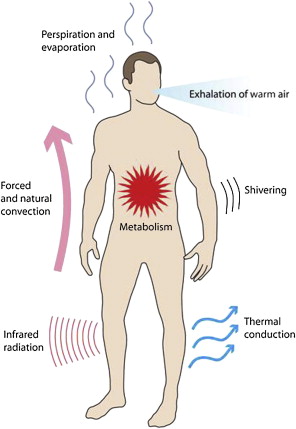
The low sensitivity of early IR cameras made them unsuitable for detecting subtle changes in temperature. Improved IR camera technology with greatly improved temperature sensitivity (<0.1°C) and computer image analysis have led to a resurgence of interest in the applications of medical IR thermography. Modern imaging systems offer real-time digital image capture in combination with state-of-the-art computer-assisted image analysis. In these systems, the thermal images are gray scale temperature coded. It is usual to apply additional color coding, with different temperatures being represented by different colors, which greatly helps in interpreting images. The rainbow palette is a frequently used color coding in medical IR thermography with the red end of the scale representing warm temperatures and the blue end representing colder temperatures ( Fig. 2 ). IR thermography is now used in major fields of medicine, including neurology, rheumatology, dermatology, oncology, and surgery. In free-flap surgery, the perfusion and reperfusion of the flap are crucial for successful surgery. It is therefore surprising that the use of IR thermography in flap surgery is so scarcely reported in the literature.
In static IR thermography, a single image is taken. The interpretation of such an image mainly depends on identifying the distribution of hot and cold spots and asymmetric temperature distribution. One of the assumptions when using this method in clinical medicine is that the distribution of body surface temperature is basically symmetric between the left and right sides of the body.
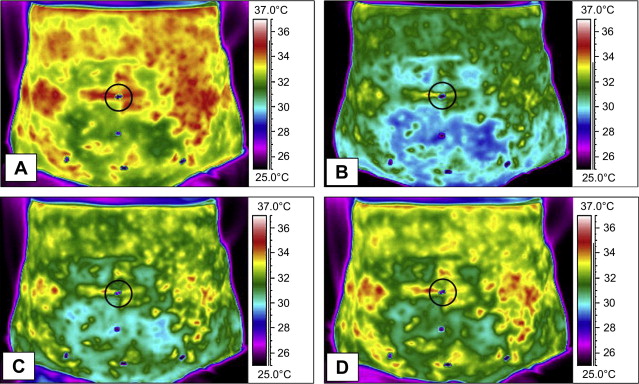
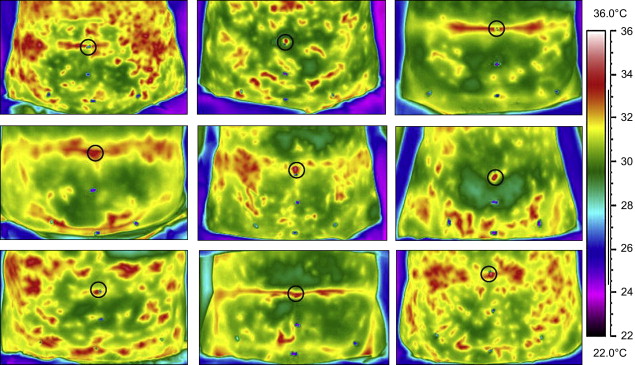
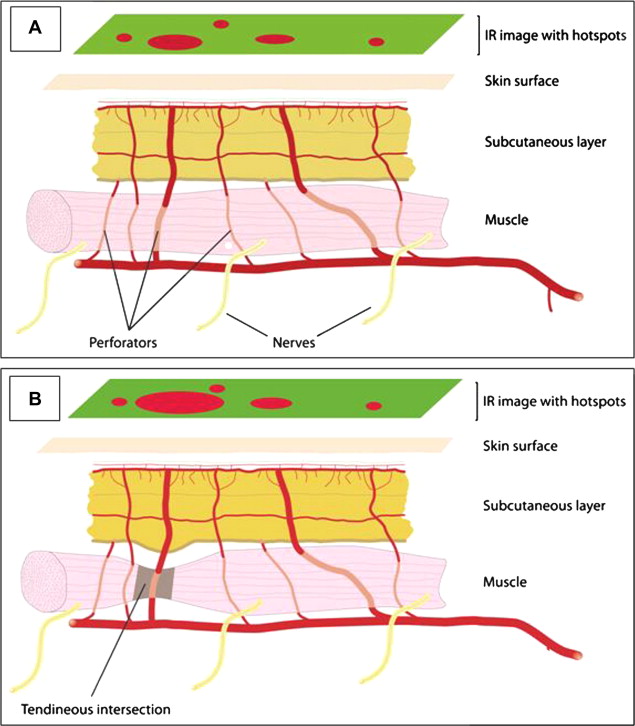
Because of the interference from complex vascular patterns, it has been proposed to monitor the thermal recovery process after exposure of the area of interest to thermal stress. This technique is called dynamic IR thermography (DIRT). Thermal stress can be achieved by, for example, fan cooling or water immersion, and by applying cold or warm objects to the skin surface. The rate and pattern at which the skin temperature recovers toward its equilibrium is registered with an IR camera. Fig. 3 illustrates the rewarming of the lower abdomen after 2 minutes of fan cooling. A special form of DIRT is the perfusion of tissue with warm or cold perfusate, as for example in organ transplantation and cardiac surgery.
In this article, we illustrate how DIRT can provide the plastic surgeon with valuable information in autologous breast reconstruction with the deep inferior epigastric perforator (DIEP) flap.
The use of DIRT in breast reconstruction with a free DIEP flap
Breast reconstruction with a free DIEP flap has become increasingly popular in autologous breast reconstruction. This flap can provide a large quantity of tissue with excellent texture and skin color that allows for the reconstruction of an aesthetically pleasing breast with little donor site morbidity. The disadvantages of using this flap are largely related to the distinct learning curve. Adequate preoperative planning, meticulous surgical technique, and a thorough understanding of the vascular anatomy are crucial for a successful postoperative result. Partial and total flap losses owing to inadequate perfusion of the flap are complications that may occur when using this technique, especially by the inexperienced surgeon. Breast reconstruction with a DIEP flap can be divided into 3 phases: a preoperative, an intraoperative, and a postoperative phase. The use of DIRT in each phase is highlighted in the following sections.
The Preoperative Phase
An important consideration in the preoperative planning of a DIEP flap is the selection of a suitable perforator. Although intraoperative selection of a perforator is possible, the large variability in the size and position of the perforators makes this rather complex. Preoperative mapping of the perforators allows the flap to be designed over a dominant perforator and may reduce operative time. Localization of the perforator is considered at least as important as determining its size. It has been advised to harvest a dominant perforator that is localized closest to the center of the skin flap.
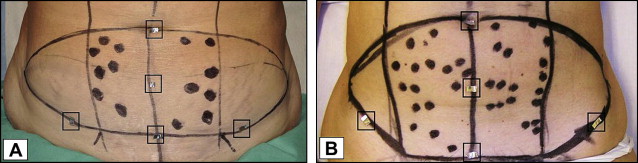
Itoh and Arai illustrated with 2 clinical cases that a perforator flap could be based on the perforator that was identified by the location of a hot spot on the thermal image during the rewarming of the skin after a cold challenge. In 2009, we reported on the value of the use of DIRT in the preoperative planning of the DIEP flap. After the outline of the flap had been drawn on the lower abdomen, the locations of arterial Doppler sounds were marked on the skin with black dots ( Fig. 4 ). All patients were examined in a special examination room with a room temperature of 22°C to 24°C and constant humidity and air circulation. Typically, the exposed abdomen was subjected to an acclimatization period at room temperature before the DIRT examination. A desktop fan was used to deliver the cold challenge by blowing air at room temperature over the abdomen for 2 minutes. This cold challenge causes visible changes in skin temperature that are well within the physiologic range, and has a short recovery period of approximately 5 minutes. The results from the analysis of the DIRT examination for each individual patient revealed large variability in the number and positions of hot spots between the left and right side. There was also large variability in the number and positions of hot spots among patients ( Fig. 5 ). Analysis of the rate and pattern of rewarming of the hot spots allowed a qualitative assessment of all the perforators at the same time. Hot spots that showed rapid and progressive rewarming could be related to suitable perforators intraoperatively. A rapid rewarming at the hot spot indicates that the perforator is capable of transporting more blood to the skin surface than a hot spot with a low rate of rewarming. A rapid progression of rewarming at the hot spot suggests a better-developed vascular network around the hotspot. It appeared that whereas all first-appearing hot spots could be associated with the location of an arterial Doppler sound, not all arterial Doppler sound locations could be related to a hot spot. In addition, the selected hot spot correlated well with a suitable perforator seen on multidetector row computed tomography (MDCT) scans ( Figs. 6 and 7 ).
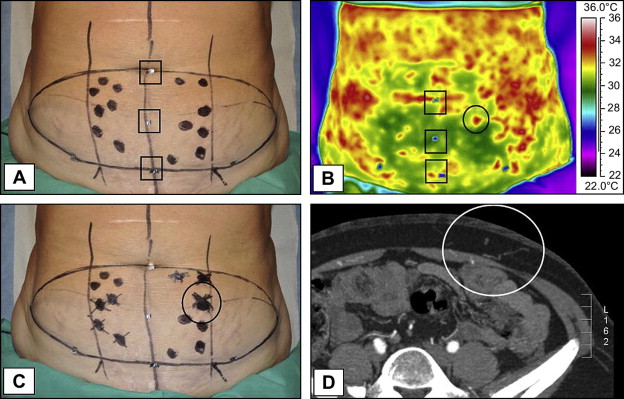
The location of the hot spot on the skin could easily be related to the location where the perforator passed through the anterior rectus fascia, although the hot spot as well as the associated Doppler sound were slightly more laterally positioned. The more laterally positioned Doppler sounds and hot spots are caused by the lateral course of vessels supplying the skin, as shown by the eminent surgeon and anatomist John Hunter (1728–1793). He explained that the orientation of vessels was a product of differential growth that had occurred in that area from the stage of fetus to adulthood. Giunta and colleagues found that the preoperative Doppler location on the skin was located within an average distance of 0.8 cm from that of the exit point of the perforator through the fascia. Interestingly, in our study the selected hot spot on the DIRT images was always associated with an audible Doppler sound and a suitable perforator.
The easiest dissection is reported for those perforators that have a perpendicular penetration pattern through the fascia and a short intramuscular course. Perforators that are located at the tendinous intersection have these characteristics and are reported to be larger than average. Interestingly, these perforators were easily identified with DIRT. The short course of the perforator from the source vessel to the skin explains the rapid rewarming of the skin at the hot spot ( Fig. 8 ). In our series of 8 patients who had an additional preoperative MDCT scan, all the perforators as selected from the DIRT examinations could be related to a clearly visible perforator on the MDCT scan. In 6 of these patients, the selected perforator was located at the tendinous intersection. The results of the DIRT examinations showed a different rate and pattern of rewarming for DIEP and superficial inferior epigastric artery (SIEA) flaps. Although the number of SIEA flaps in our series was small, it appeared that if the SIEA system was dominant, only small hot spots were seen at the center of the lower abdomen in contrast to the situation where the deep inferior epigastric artery (DIEA) system was dominant. The more laterally positioned vascular territory of the SIEA flap, as well as the different vascular anatomy, help to explain the differences in the results obtained from the DIRT examinations of DIEP and SIEA flaps. To reduce donor site morbidity, surgeons may follow the algorithm as proposed by Arnež and colleagues and explore the possible use of an SIEA flap before they decide to harvest a DIEP flap. Using this algorithm, one can rule out the existence of a dominant SIEA system before one uses the results of the DIRT examination for a DIEP flap.
The Use of DIRT in the Intraoperative Phase
The intraoperative phase of breast reconstruction with a DIEP flap can be divided into 3 periods: the period of dissection of the perforator, the period after opening of the anastomoses, and the period of flap modeling and inset.
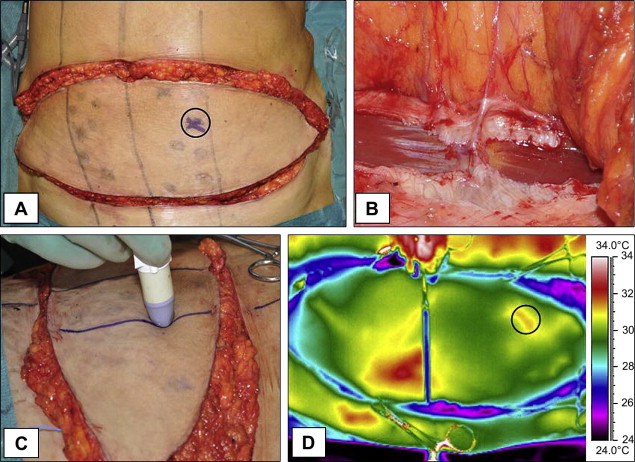
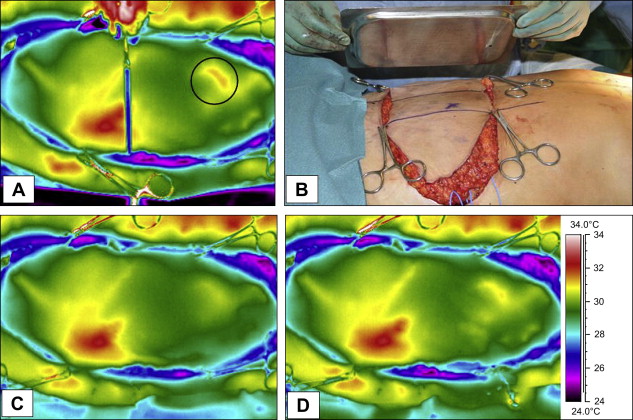
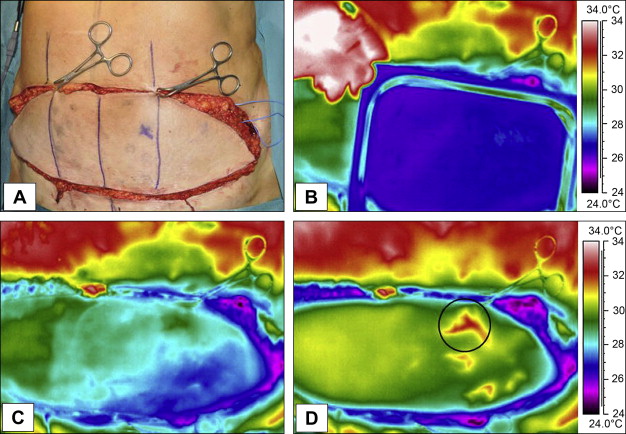
One of the disadvantages of perforator flap surgery is the complex dissection of perforators. A meticulous microsurgical technique is required to avoid inadvertent damage to the perforator. In 2006, we reported on the intraoperative use of DIRT in free DIEP flap surgery. After the selected perforator is dissected and with the flap still at the lower abdomen, DIRT can be used to confirm patency of the perforator. Normally a hot spot will be seen on the IR images that correlates with the location of the entrance point of the perforator into the flap. The quality of the perforator can be assessed by analyzing the rate and pattern of rewarming after the skin area above the perforator is exposed to a conductive thermal challenge. A metal plate at room temperature is gently applied to the skin surface for 30 seconds ( Figs. 9 and 10 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree