© Springer Nature Singapore Pte Ltd. 2018
Ichiro Katayama, Hiroyuki Murota and Takahiro Satoh (eds.)Evolution of Atopic Dermatitis in the 21st Centuryhttps://doi.org/10.1007/978-981-10-5541-6_2222. Drug Therapy: Systemic
(1)
Department of Dermatology, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, 465 Kajii-cho, Kawaramachi-Hirokoji, Kamigyo-ku, Kyoto 602-8566, Japan
Abstract
Systemic therapy is indicated for patients with severe atopic dermatitis (AD) who do not respond to adequate topical treatment or who cannot continue to receive topical therapy due to its side effects, such as skin atrophy. Before administering systemic immunosuppressive or immunomodulatory pharmaceuticals, clinicians should check whether the diagnosis of AD is correct, consider possible differential diagnoses, and examine whether the patient’s adherence to topical treatments is sufficient. The currently available immunosuppressive and immunomodulatory drugs mainly produce their anti-inflammatory effects by suppressing the proliferation and functions of lymphocytes. However, since they can cause a range of adverse effects, strict monitoring before and during treatment is mandatory. Patient education regarding the possible adverse effects of treatment, the pathogenesis of AD, and the practical measures for treating AD is very important.
Keywords
CyclosporineAzathioprineMycophenolic acidMethotrexateAntihistamine22.1 Introduction
Atopic dermatitis (AD) is a disease characterized by relapsing eczema and pruritus. Type 2 cytokines play critical roles in the pathogenesis of allergic inflammation in AD [1]. The current evidence-based strategies used to treat the condition consist of three primary measures: (1) the use of topical anti-inflammatory agents, such as topical corticosteroids and topical calcineurin inhibitors; (2) the application of emollients/moisturizers to treat cutaneous barrier dysfunction; and (3) the avoidance of exacerbating factors [2]. Most patients with AD can control their skin disease with these approaches. Systemic therapy is required in patients with severe AD who do not respond to these treatments. The systemic treatments for AD are subdivided into three categories: (1) immunosuppressive and immunomodulatory pharmaceuticals, (2) antihistamines, and (3) others. In this chapter, I briefly review the information about currently available systemic treatments for AD.
22.2 Immunosuppressive and Immunomodulatory Pharmaceuticals
22.2.1 Before the Start of Immunosuppressive and Immunomodulatory Pharmaceutical Treatment
Before judging that a patient’s condition is refractory to treatment with topical corticosteroids and topical calcineurin inhibitors, clinicians should check whether the diagnosis of AD is correct and consider possible differential diagnoses including allergic contact dermatitis, seborrheic dermatitis, prurigo simplex, cutaneous mycosis, scabies, miliaria, ichthyosis, xerotic eczema, hand dermatitis (nonatopic), cutaneous lymphoma, psoriasis, immunodeficiency diseases (hyper-IgE syndrome and Wiskott-Aldrich syndrome), collagen diseases (systemic lupus erythematosus and dermatomyositis), and Netherton syndrome [2]. In addition, allergic contact dermatitis caused by topical medications is often misdiagnosed as refractory AD [3].
During the treatment of AD, if the expected effects are not obtained with topical corticosteroids and topical calcineurin inhibitors, it is important to confirm whether these drugs have been correctly applied. Physicians should educate patients and their caregivers about the appropriate amount of the prescribed drug to apply (e.g., a blob of ointment (~0.5 g) measuring 5 mm in diameter that is pushed out from a tube onto the area between the tip and first joint of the second finger is appropriate for covering both palms of a British adult, i.e., approximately 2% of the body surface area of an adult (fingertip unit)) [2, 4, 5]. We should monitor patients’ treatment adherence because poor treatment adherence often prevents patients from achieving disease control. Poor adherence can also be misinterpreted as a poor response to treatment, which might lead to the patient receiving more powerful and potentially dangerous systemic medications. In general, oral medication is associated with significantly better adherence than topical medication.
In patients with severe chronic eczema, hospitalization for a few weeks often leads to the patient’s AD being brought under control with intensive topical therapy, and education aimed at increasing the patient’s understanding of the mechanism responsible for their disease and improving their treatment adherence can also be provided [2, 6].
Before starting any immunosuppressive or immunomodulatory drug therapy for AD, a detailed clinical and laboratory examination of the patient is essential. In particular, underlying active infectious diseases including hepatitis B and C, HIV infections, and syphilis have to be ruled out. The organ function tests that should be performed before and during therapy depend on the drugs prescribed [7].
22.2.2 Cyclosporine
Cyclosporine, a cyclic non-ribosomal peptide composed of 11 amino acids, inhibits T-cell activation and proliferation by preventing the dephosphorylation of nuclear factor of activated T cells [8]. Cyclosporine inhibits the production of cytokines, such as interleukin (IL)-2, IL-3, and IL-6, by T cells, and, thus, has immunosuppressive effects.
In randomized placebo-controlled trials, cyclosporine has been shown to have significant beneficial effects on skin lesions and pruritus and, hence, to improve the quality of life of adult patients with severe AD [9, 10]. The efficacy of cyclosporine against severe childhood AD has also been demonstrated in clinical studies [11, 12]. A meta-analysis assessing the effectiveness of systemic cyclosporine in patients with severe AD showed that cyclosporine consistently decreased the severity of AD and was similarly effective in children and adults [13]. It also revealed that 6–8 weeks of cyclosporine treatment had a relative effectiveness of 55% (95% confidence interval, 48–62%).
Cyclosporine has been approved as a first-line systemic treatment for severe AD in children and adults in some European countries. In Japan, cyclosporine is licensed for use in patients with severe adult AD who do not respond to conventional treatments and exhibit eruptions and marked inflammation involving ≥30% of their body surface area. The initial dose of cyclosporine for adult patients with severe AD is 3 mg/kg per day in Japan, which should be increased or decreased in accordance with the patient’s symptoms, but it should not exceed 5 mg/kg per day [2].
It is recommended that cyclosporine to be tapered and eventually discontinued after an improvement in the patient’s AD has been achieved. In Japan, the package insert for cyclosporine warns physicians that the cyclosporine treatment period should be limited to ≤12 weeks in AD patients. Some clinical studies have examined relapse rates after the discontinuation of cyclosporine treatment in AD patients [12, 14, 15]. In these studies, the treatment protocol allowed the use of topical steroids after the discontinuation of cyclosporine. In one study, about 50% of patients relapsed within 2 weeks of the discontinuation of cyclosporine, and about 80% relapsed within 6 weeks [14]. In another study, 73% of the patients relapsed within 24 weeks [15]. In pediatric patients with AD, 86% of patients relapsed within 9 months [12]. Interestingly, Kim et al. compared the efficacy and relapse rate of cyclosporine treatment combined with topical therapy involving topical corticosteroids and topical calcineurin inhibitors with those of cyclosporine alone in moderate-to-severe AD patients [16]. The treatment success rate was significantly higher in the combination group. The combination group had a shorter median time to response, a lower cumulative dose, and a longer time to relapse than the monotherapy group [16].
Renal dysfunction and increased blood pressure are the most concerning adverse effects of cyclosporine and are particularly associated with long-term prescription. It is necessary to monitor patients’ blood pressure, serum creatinine levels, complete blood counts, and blood biochemistry before and during cyclosporine therapy [7, 17]. Gastrointestinal symptoms and headache are the most commonly reported adverse events associated with cyclosporine treatment in pediatric patients with severe AD [13]. Adverse events appear to be more common in patients treated with higher doses [13]. Cyclosporine should not be combined with phototherapy because it increases the risk of nonmelanoma skin cancer [18].
22.2.3 Azathioprine
Azathioprine, an imidazolyl derivative of 6-mercaptopurine, is converted to 6-mercaptopurine, which blocks the synthesis of RNA and DNA and, thus, inhibits the proliferation of T and B cells and suppresses the functions of natural killer cells [8]. It is widely used as immunosuppressant drug during solid organ transplants and as a treatment for rheumatic arthritis and inflammatory bowel disease [8]. Unlike cyclosporine, azathioprine takes several weeks to reach a steady-state level in the blood and is therefore slow to take effect [18]. Thiopurine methyltransferase (TPMT), one of the enzymes involved in the metabolism of 6-mercaptopurine into inactive compounds, is affected by genetic polymorphisms, and inherited changes in its activity can impact on patients’ responses to azathioprine [8].
Regarding the efficacy of azathioprine against AD, some case series have indicated that azathioprine might be a useful treatment for recalcitrant pediatric, adolescent, and adult AD [19–24]. Two double-blind, randomized controlled trials have also demonstrated that treatment with azathioprine produced clinically relevant improvements in moderate-to-severe AD [25, 26]. In one study, 54 (86%) participants completed the study, 2 (3%) withdrew from the placebo group, and 7 (11%) withdrew from the azathioprine group. By week 12, azathioprine had brought about a 37% improvement in mean disease activity compared with the 20% improvement produced by the placebo [26]. In another study, 37 subjects were enrolled, and 16 were withdrawn (12 during azathioprine treatment and 4 during placebo treatment). After 3 months, the eruption score had fallen by 26% in the group treated with azathioprine, whereas it had only fallen by 3% in the placebo group [25].
The major adverse effects associated with azathioprine include gastrointestinal complaints, such as nausea, liver dysfunction, and leukopenia. Patients who exhibit reduced or no TPMT activity (about 10% and 0.3% of the population, respectively) are at higher risk of profound immunosuppression [27]. Reduced TPMT activity is also related to the risk of fatal myelosuppression [18]. Thus, patients’ TMPT activity should be checked before the start of azathioprine treatment because the serious adverse effects of azathioprine treatment are dose-dependent [17]. Furthermore, an increased risk of nonmelanoma skin cancer has been detected in transplant recipients on long-term azathioprine treatment [18]. It is proposed that this is mediated via azathioprine-induced increases in photosensitivity, so all patients that receive such treatment should be advised about photoprotection [18].
22.2.4 Mycophenolic Acid
Mycophenolate mofetil is rapidly absorbed and hydrolyzed into the active compound mycophenolic acid [8]. Mycophenolic acid inhibits inosine monophosphate dehydrogenase, which is required for de novo purine synthesis, and has immunomodulatory effects on T and B cells [17]. Recently, enteric-coated mycophenolate sodium (EC-MPS) was developed as a way of decreasing the adverse gastrointestinal effects of mycophenolic acid treatment [18].
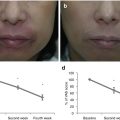
In an open-label pilot study, 1 g mycophenolate mofetil was administered orally twice daily for 4 weeks to ten adult patients with moderate-to-severe AD, which was followed by 500 mg twice daily from weeks 5 to 8 [28]. Treatment with mycophenolate markedly reduced the severity of AD within 4 weeks in all patients, and after 8 weeks, the mean ± SD SCORAD (SCORing Atopic Dermatitis) index had dropped from the pretreatment value of 49.2 ± 13.8 to 21.9 ± 26.5 (P < 0.01). In the latter study, most patients tolerated the treatment well, except one patient who developed herpes retinitis after 4 weeks. In a retrospective chart review of 20 adult patients with moderate-to-severe AD, the conditions of 17 patients improved within 4 weeks of the start of mycophenolate mofetil treatment [29]. Ten patients achieved disease remission and were subsequently able to discontinue mycophenolate mofetil. Two case series of pediatric AD patients also demonstrated positive responses to mycophenolate mofetil treatment [20, 30]. Haeck et al. performed an observer-blinded randomized controlled trial, in which the efficacy of EC-MPS was compared with cyclosporine as a maintenance treatment for adult patients with moderate-to-severe AD [31]. Although the clinical improvement achieved with EC-MPS was delayed in comparison with that induced by cyclosporine, both treatments were similarly effective as maintenance therapies in patients with AD. Interestingly, the disease activity of the patients in the cyclosporine study arm was significantly greater than that seen in the EC-MPS study arm after the withdrawal of medication, suggesting that EC-MPS might exhibit more prolonged treatment effects.
In studies of AD, mild headaches and nausea were the most commonly reported adverse effects of mycophenolic acid therapy [17, 28, 29, 31]. Treatment with mycophenolic acid also increases the risk of liver enzyme abnormalities and infections, such as herpes zoster, herpes simplex, or staphylococcal infections [28, 29, 31, 32]. Therefore, it is necessary to monitor patients’ complete metabolic panels, liver enzyme levels, and complete blood counts before and during therapy with mycophenolic acid [17].
22.2.5 Methotrexate
Methotrexate is an analogue of folic acid, which inhibits purine and pyrimidine synthesis and, thus, suppresses cellular proliferation [8]. It is also considered to negatively affect T-cell function and is used to treat chronic inflammatory diseases, such as rheumatic arthritis and psoriasis.
A randomized controlled trial including 40 pediatric patients with severe AD, who ranged in age from 8 to 14, found that oral methotrexate (initial dose, 5 mg; maintenance dose, 7.5 mg weekly) and cyclosporine (2.5 mg/kg/day) exhibited similar efficacy during 12 weeks’ treatment [33]. Mild and temporary adverse effects were reported in some patients in both groups. In another randomized controlled trial, the efficacy of methotrexate (dosage, 10–22.5 mg/week) was compared with that of azathioprine (dosage, 1.5–2.5 mg/kg/day) in adult patients with severe AD [34]. Both treatments displayed similar efficacy levels (42% versus 39% SCORAD reduction, respectively). Although no statistically significant differences in the number or severity of adverse events were detected, blood count abnormalities were more common in the azathioprine group. Therefore, it was indicated that methotrexate is an alternative first-line systemic treatment for severe AD [18, 35].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree