47
Dorsal Dislocations of the Proximal Interphalangeal Joint
Rosa L. Dell’Oca and Amy Ladd
History and Clinical Presentation
A 40-year-old right hand dominant mechanic presented with a painfully swollen incongruent proximal interphalangeal (PIP) joint of his right index finger after a tire exploded while he was increasing the air pressure. Closed reduction, although successful, resulted in an unstable joint.
Physical Examination
The PIP joint demonstrated 15 degrees of ulnar deviation with considerable edema and a volar laceration. Tenderness was elicited over the volar and radial aspects of the joint. Pain limited full active flexion, and the middle phalanx subluxed dorsally at 10 degrees of active extension.
Diagnostic Imaging
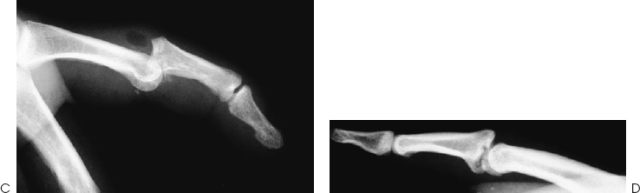
Anteroposterior, lateral, and oblique radiographs of the involved digit were obtained (Fig. 47–1).

Differential Diagnosis
Dorsal dislocation of the PIP joint
Lateral dislocation of the PIP joint
Volar dislocation of the PIP joint
Fracture of the distal proximal phalanx
Fracture of the proximal middle phalanx
Sprain of the PIP joint
Lateral dislocation: greater than 20 degrees of angulation with ulnar/radial stress of the PIP joint; radial or ulnar joint tenderness with or without volar plate tenderness; anteroposterior (AP) radiograph may demonstrate lateral displacement.
Volar/lateral dislocation: lateral radiograph exhibits middle and distal phalanges at an oblique angle as compared with the proximal phalanx.
Volar dislocation: tenderness of the dorsal aspect of the base middle phalanx; lateral radiograph reveals a fracture of the dorsal aspect of the base of the middle phalanx.
Fractures: AP, lateral, and oblique (condyles) radiographs may display fractures of the head of the proximal phalanx or the base of the middle phalanx.
Diagnosis
PEARLS
- Obtaining perfect lateral radiographs to detect the subtlest incongruity
- Obtaining prompt attention by hand specialist, or knowledgeable practitioner and to not ignore this common injury
PITFALL
- Disregarding the injury as a simple sprain without adequate physical and radiographic examination
Dorsal Proximal Interphalangeal Joint Dislocation
Dorsal PIP dislocations are probably common but underreported, because many high-paid athletes play with fresh injuries set in the field, or present with old untreated injuries that may be painful, unstable, or fused. Estimated at 9/100,000/year, the incidence of dorsal PIP fracture dislocations is much higher.
History, physical examination, and radiographs reveal the diagnosis and prognosis, and facilitate treatment. History divulges the mechanism of injury and suggests the final configuration of the joint despite memory lapse or spontaneous or deliberate reduction. The joint may assume the characteristic bayonet configuration or an obvious posture of hyperextension but occasionally subtle subluxation requires radiographic elucidation. Palpation delineates the injured structures and active range of motion may reveal instability with progressive extension. Although pain and edema typically limit flexion, a torn volar plate interposed within the joint must be considered. If radiographic evaluation displays joint congruity, then subtle instability may be elucidated by passive range of motion facilitated by a digital block.
A simple sprain, recognized by a moderate amount of tenderness over the bruised but stable joint with a normal radiograph represents a partially torn ligament.
Despite the check rein ligaments, proximal detachment of the volar plate occurs experimentally with slow hyperextensile forces. Conversely, longitudinal accelerated hyperextensile forces cause distal rupture of the transversely oriented fibrocartilaginous fibers of the volar plate. This injury alone allows greater than the normal 10 degrees of hyperextension. Typically, in these hyperextension injuries there is no history of abnormal joint position, no evidence of instability on active and passive range of motion, and no articular incongruity or fracture on radiographs. Even with an incomplete longitudinal split in the collateral ligament, the remaining intact accessory collateral ligament imparts some stability.
Higher energy forces produce tears between the thin accessory collateral ligament and the thick primary collateral ligament in addition to volar plate disruptions. Experiments suggest that partial volar plate tears represent areas of potential weakness at risk of rupture with repeated stress. Typically, these injuries present with a history of joint misalignment and radiographs may demonstrate a small volar fragment.
Part of the weak volar central trabecular base of the middle phalanx may remain attached to the volar plate, otherwise known as an avulsion injury. Larger volar fragments typically result from greater longitudinal rather than hyperextensile forces, where the proximal phalanx shears off the volar base of the middle phalanx. Smaller volar fragments (<30–50%) retain support from the remaining accessory collateral ligaments and a portion of the primary collateral ligament (Eaton and Dray’s “stable dislocations”), whereas larger fragments portend relying solely on the extensor tendon and dorsal capsule for stability in flexion and have no support in extension, which explains the propensity to redislocate after reduction (Eaton and Dray’s “unstable dislocations”). A direct correlation exists between the percent of volar middle phalanx surface fractured and the likelihood of dorsal subluxation/dislocation. Maximum contact between the articular surfaces of this ginglymus joint, and the action of the flexor and extensor tendons pulling axially through a column consisting of the middle phalangeal base, resting on the proximal phalangeal condyles stabilized by the interdigitation of the intercondylar sulcus and eminence, resist dislocation even in the face of collateral ligament and volar plate disruption. With intraarticular fractures, the residual middle phalangeal dorsal articular surface and shaft form an inclined plane that tends to slide dorsally and proximally as the extensor and flexor tendons pull the distal portion of the middle phalanx volarly and the proximal end of the middle phalanx dorsally, creating a zigzag posture. Furthermore, the slightly different radii of curvature of the condyles allow some rotation despite the inherent lateral stability, which explains disproportionate injury to radial versus ulnar collateral ligaments.
Classification systems with varying emphasis on the degree of ligamentous integrity, the percentage of articular involvement, or the degree of subluxation exist to facilitate the correct treatment. The history of injury, the point and degree of instability, and radiographic evaluation are adequate determinants in our opinion.
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








