Ask the patient:
When did you first notice hair loss?
When did your hair last seem normal?
Was it sudden or gradual?
Is hair falling out (and seen in the drain or brush) or do you notice thinning (not as thick)?
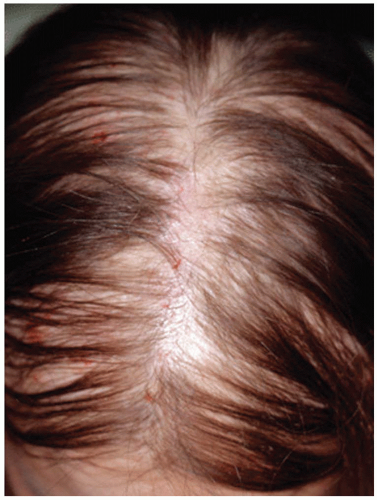
Is the hair loss diffuse or patchy?
Is it only on the scalp or in other areas?
Any recent trauma, physical, or emotional? If yes, when did this occur?
What treatments have you tried?
Detailed inquiry about:
Hair care, products, styling
Use of tools (hot combs), relaxers or dyes, heat, use of extensions or weaves, and styling that pulls or binds (corn rows, ponytails, etc.)
|
List medications, especially new medications
Consider undeclared use of anabolic cortico steroids
Corticosteroids is one word use of prescription or over-the-counter herbs or supplements
Recent illness, surgeries, anesthesia, weight loss (diets)
Thyroid disease
Ob/gyn issues: menstrual irregularities, infertility
Skin conditions: acne, hirsutism, etc.
|
Balding male or female family members Thyroid disease |