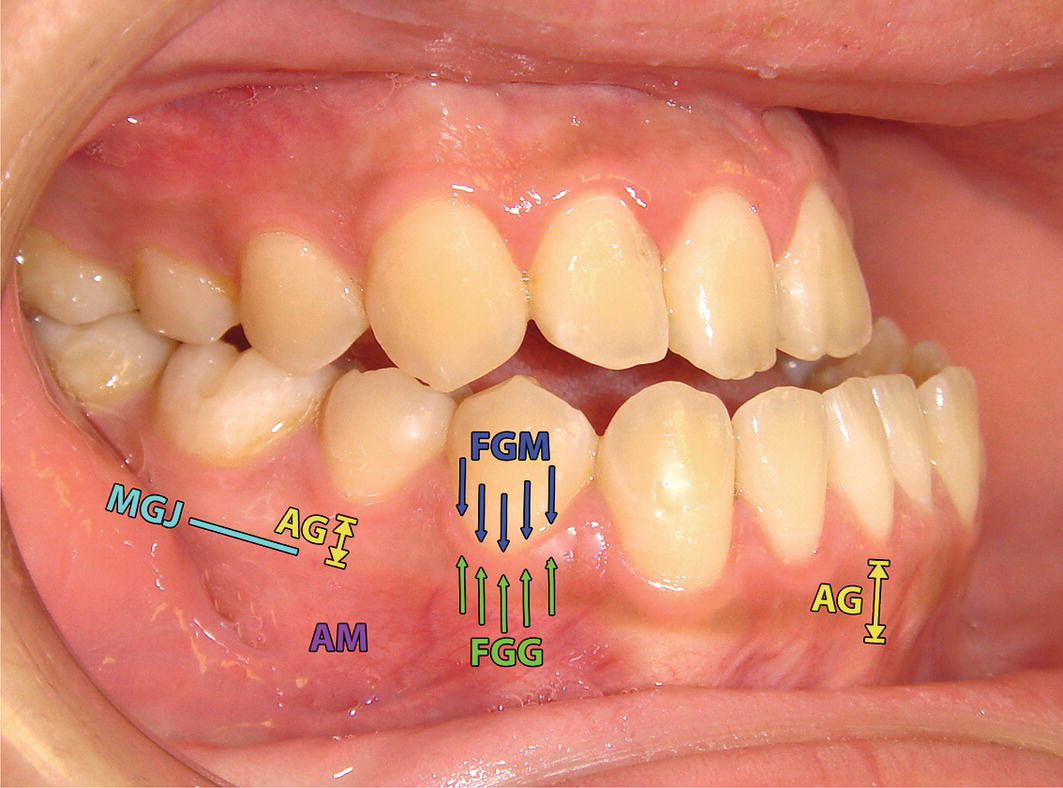
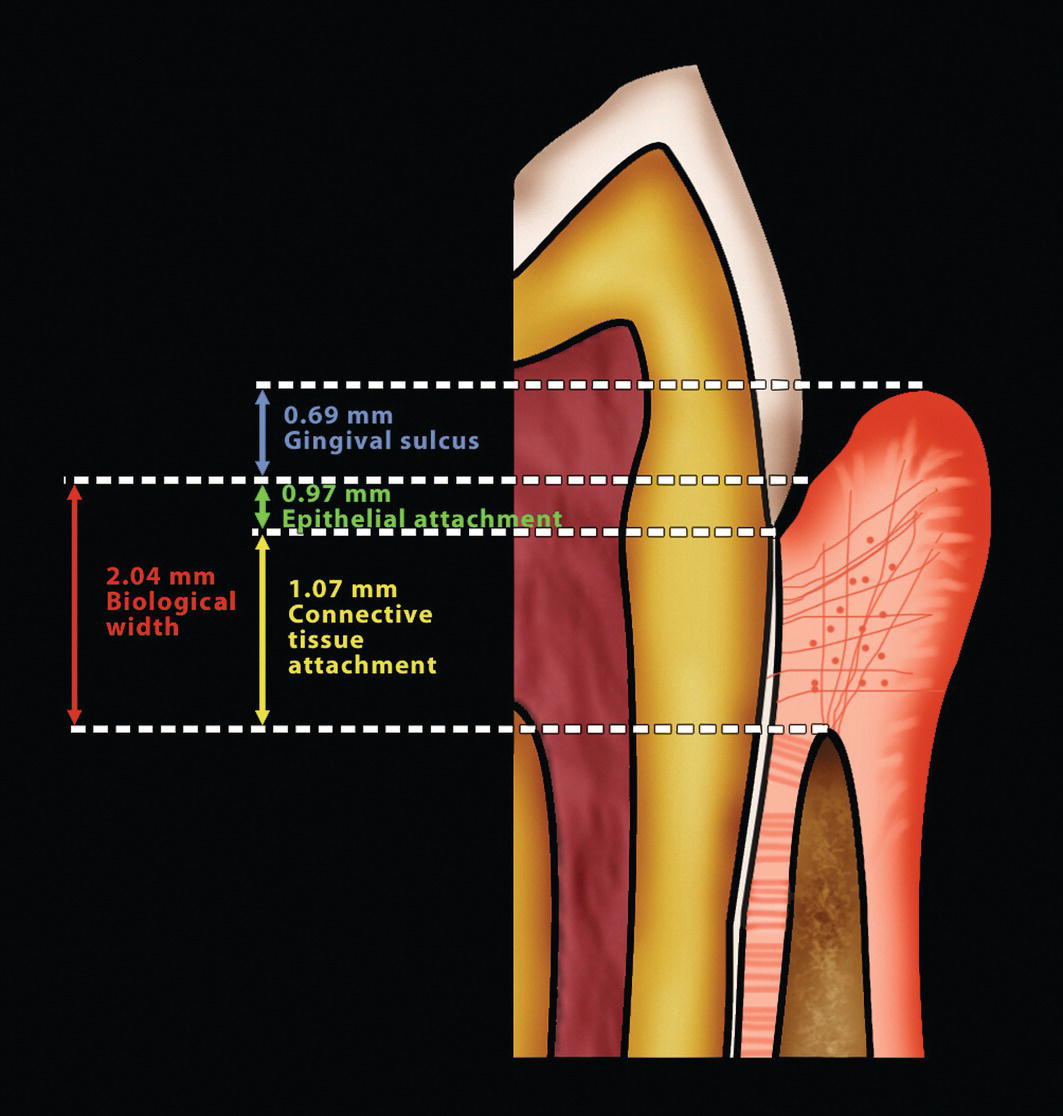
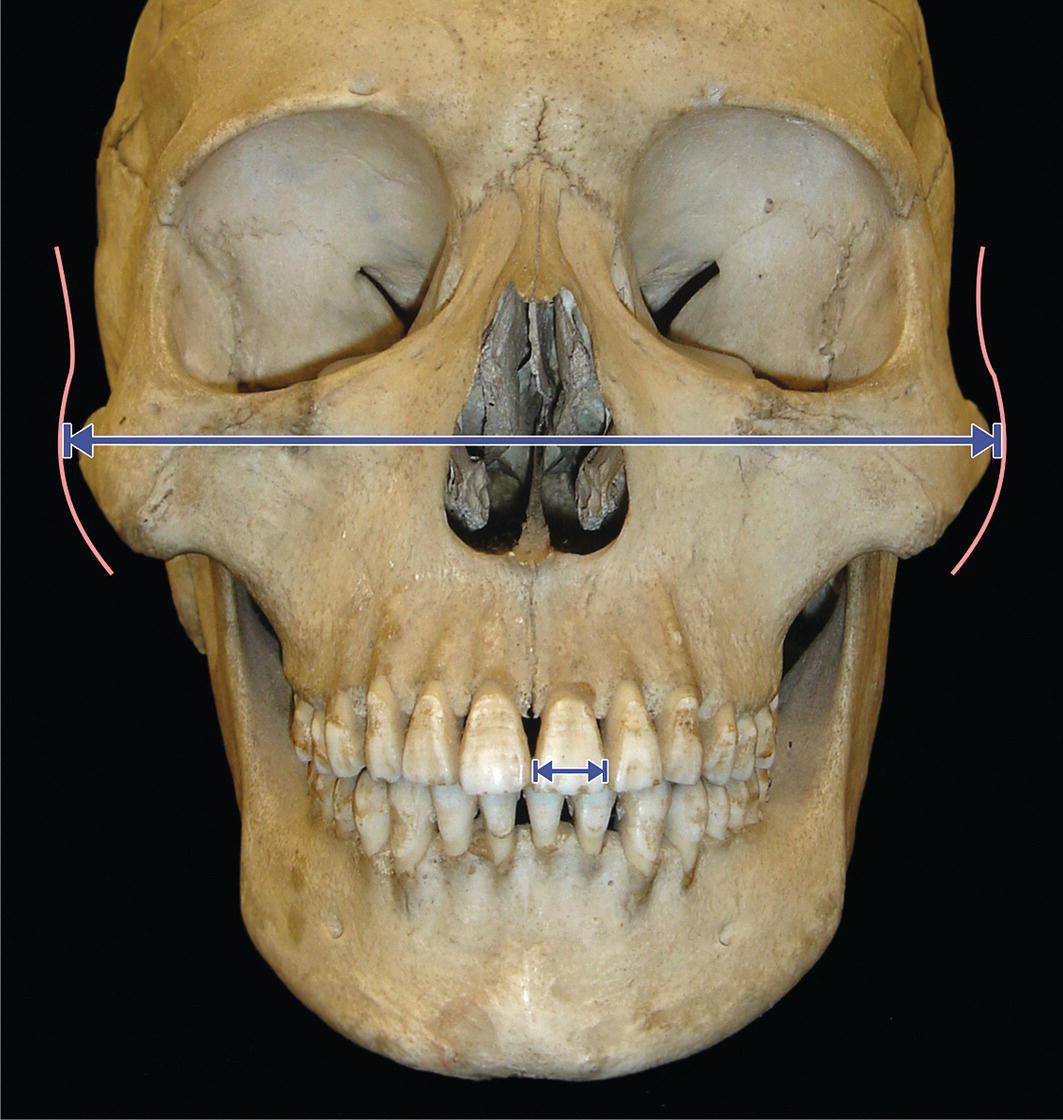
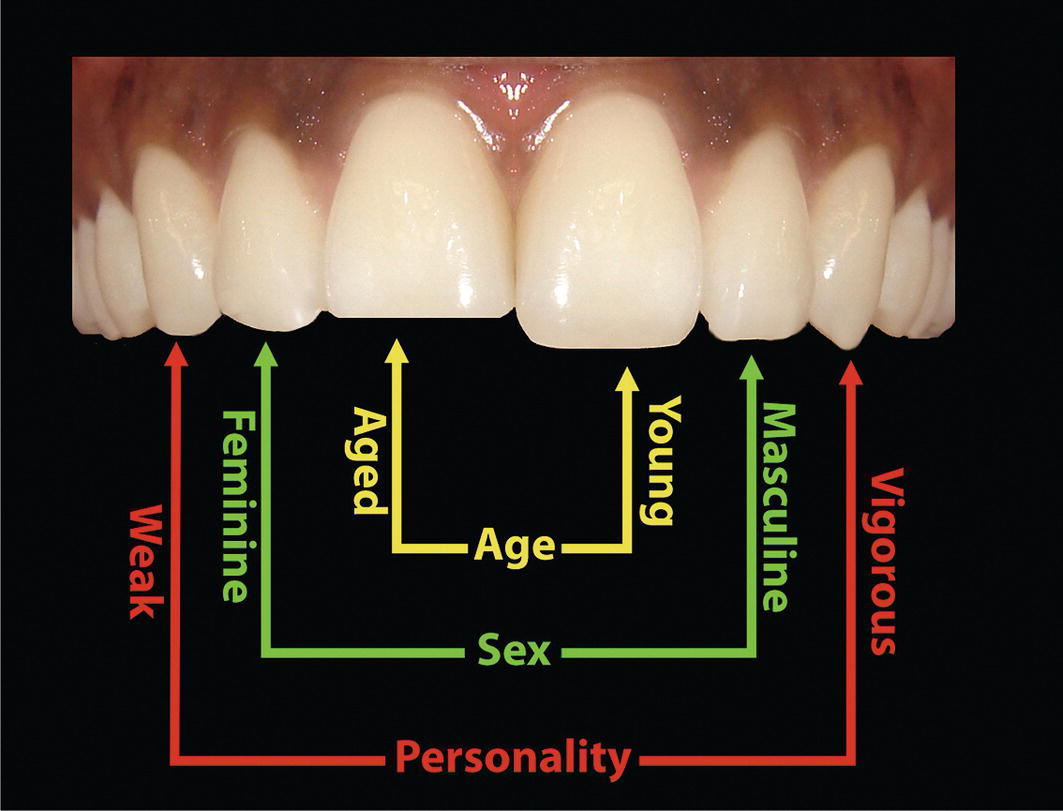
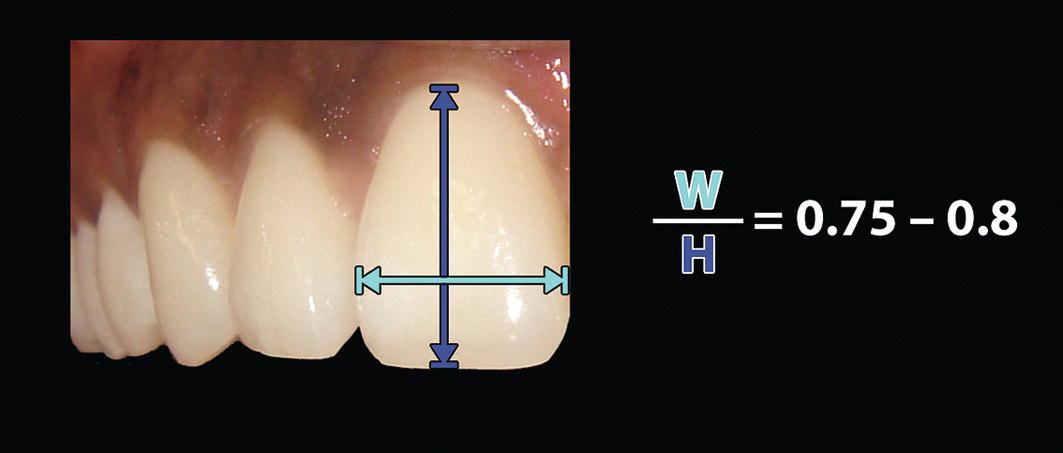
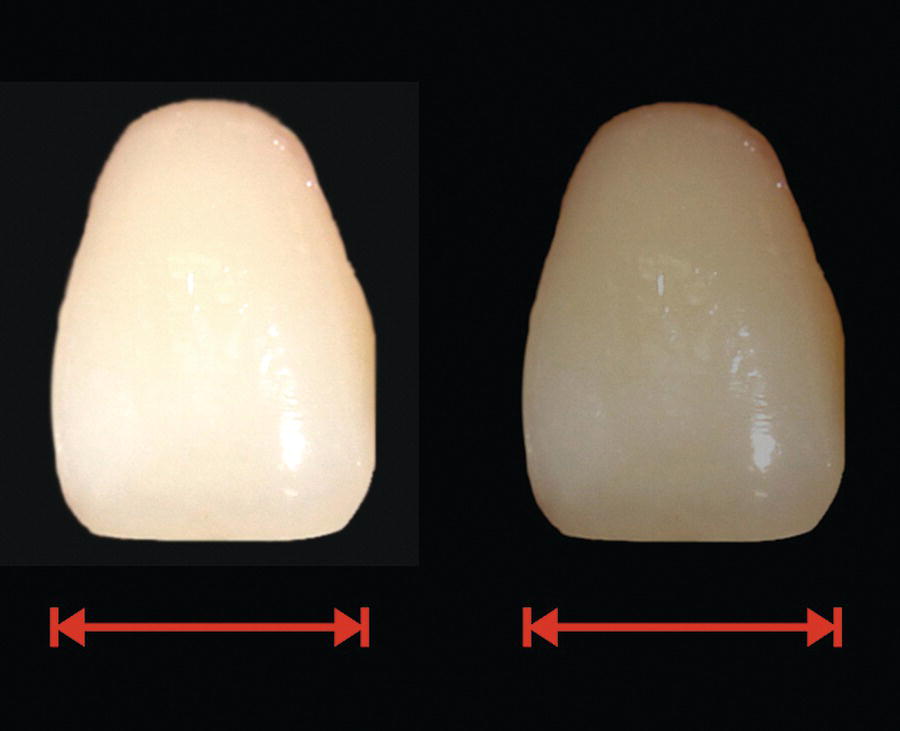
The dentogingival complex may be considered an aesthetic unit of the face, i.e. the dentogingival aesthetic unit, composed of the gingival subunit and the dental subunit. The teeth occupy approximately one‐fifth of the surface area of the oral cavity in adults. They serve the important functional role of mastication and are essential for proper speech and dentofacial aesthetics. In mammals, the teeth are attached to the supporting alveolar bone by a fibrous connective tissue, termed the periodontal ligament (PDL); the flexibility of the PDL within this structural relationship permits the teeth to withstand the considerable forces of mastication. In humans, the succession of the primary (deciduous) dentition by the larger and more numerous teeth of the secondary (permanent) dentition accommodate the substantial growth of the face and jaws.1 Anatomically, the teeth consist of a crown and a root; the junction between the two is termed the cervical margin. The term clinical crown refers to the part of the crown visible in the oral cavity. The anatomical crown is covered by enamel, which is a hard, acellular and relatively brittle tissue; it is the most highly mineralized tissue in the human body (96% mineralized). Enamel would be unable to withstand the forces of mastication without fracture was it not for its support from the resilient underlying specialized connective tissue termed dentine. Dentine is a relatively hard (70% mineralized), avascular tissue; it is yellowish‐white, which gives teeth their colour. It is sensitive and more importantly, capable of repair by the laying down of secondary dentine by cells called odontoblasts, which initially form the dentine and subsequently line the periphery of the dental pulp. The dentine encloses the central pulp chamber, which is filled with a soft connective tissue called the pulp. The oral cavity is lined by oral mucosa (oral mucous membrane), which is comprised of the following:2 The term periodontium (Greek peri‐: around; odontos: tooth) refers to the supporting tissues of the teeth. It is comprised of the following component parts: Figure 24.1 Gingival anatomy. The free gingiva extends from the free gingival margin (FGM) apically to the free gingival groove (FGG), which is positioned at a level corresponding to the cementoenamel junction. The attached gingiva (AG) extends from the free gingival groove region to the mucogingival junction (MGJ), where it becomes continuous with the lining alveolar mucosa (AM) of the oral cavity. The existence of the PDL as a functional unit together with the root cementum and alveolar bone is the reason orthodontic forces are able to move teeth through the supporting alveolar bone. It is much more difficult to modify the position of the basal bone of the maxilla and mandible. This may be achieved to an extent by attempting to modify jaw growth; otherwise altering basal bone position or morphology requires corrective jaw surgery (orthognathic surgery). A cross‐section of the dentogingival unit reveals that it is composed of three parts. Gargiulo et al.3 analysed autopsy specimens to calculate the vertical depth of each of these parts. From an occlusal to apical direction, these are (Figure 24.2): Figure 24.2 The dentogingival unit and ‘biological width’. The combination of the linear height of the epithelial and the connective tissue attachment (2.04 mm) has been termed the biological (or biologic) width.4 This may be defined as the combined width of connective tissue and junctional epithelial attachment formed adjacent to a tooth and superior to the crestal bone. The biological width has been demonstrated to be remarkably consistent; conversely, the gingival sulcus depth is highly variable. The biological width is three‐dimensional and surrounds every tooth; hence the alternative suggested term is ‘biological zone’. This zone acts as a natural barrier, protecting the periodontal ligament and the alveolar bone from the ingress of pathogens; bacterial ingress may thus lead to periodontal disease. Dental restorative procedures must also respect this ‘zone’ in order to maintain a healthy periodontium; impingement of the margins of restorations into the biological width results in inflammation, loss of epithelial attachment, apical migration of the junctional epithelium and thereby periodontal pocket formation. The position of the maxillary incisor crowns in relation to the face in the evaluation of dentofacial aesthetics has been described (see Chapter 23). The shape and size of the maxillary incisor crowns form the starting point in the clinical evaluation of dentogingival aesthetics. The morphology of the maxillary incisor crowns, as observed in frontal view, involves the amalgamation of the three basic geometrical shapes, i.e. the circle, square and triangle, from which any shape may be created. Tooth shape is genetically determined and there is considerable individual variability. The overall shape of the crowns of the maxillary incisor teeth in each individual will fit predominantly into one of the following categories (Figure 24.3): Tooth morphology is remarkably consistent.5 When aberrations in the shape of teeth do occur, most commonly in the maxillary lateral incisor crown, which may be peg‐shaped or diminutive, and the third molars, it is as a result of some effect early in the developmental history of the tooth. In fact, the crown pattern of each tooth is determined during the bell stage of dental development.1 A number of theories have been proposed regarding maxillary incisor crown morphology: Figure 24.3 Maxillary incisor crown shape: (A) ovoid (barrel‐shaped); (B) rectangular; and (C) triangular. Figure 24.4 Tooth width–face width ratio: maxillary central incisor crown width to bizygomatic facial width ratio has been described as approximately 1:16.10–12 Figure 24.5 SAP (sex, age and personality) theory. Figure 24.6 Mammelons usually appear as three small rounded prominences on unworn incisal edges. Radia et al.12 undertook a prospective clinical investigation to determine the relationship between maxillary central incisor proportions and facial height and width in adults. The ‘biometric ratio’ of 1:16 for maxillary central incisor:bizygomatic width was not reconfirmed exactly, but very closely, with a mean ratio of 1:15.6. A ratio of 1:18 was proposed for maxillary central incisor height to total face height (Tr‐Me’) and 1:12 for face height (N’‐Me’). Figure 24.7 Gingival recession has exposed the root surfaces, which show signs of abrasion. Tooth size is genetically determined. Tooth size does not necessarily correlate well with standing height or stature, i.e. a tall individual may have small teeth. However, men tend to have larger teeth than women, and black individuals tend to have larger teeth than Caucasians.18 Maxillary incisor crown size may be measured as the mesiodistal width, the inciso‐gingival height and the width‐to‐height ratio. Various authorities have provided data on maxillary incisor crown dimensions in Caucasian individuals, from which are derived the following ‘average’ dimensions: The average width‐to‐height ratio of the maxillary central incisor crown is 0.75–0.8, i.e. the crown width should be 75–80% of its height (Figure 24.8). A ratio of less than 60% creates a tall narrow crown, whereas a ratio greater than 85% results in a short wide crown appearance. This ratio is more important than the component crown width or height. Figure 24.8 The width‐to‐height ratio of the maxillary central incisor crown is more important than the component crown width or height. Figure 24.9 Optical concepts: maxillary incisors of reduced height will appear wider. Figure 24.10 Optical concepts: whiter, brighter teeth appear larger and more prominent than darker teeth. Cooper et al.20 undertook an attractiveness research investigation to determine the influence of varying the width‐to‐height ratio of maxillary central incisors on perceived smile aesthetics. They found that an 82% (+/− 4%) width‐to‐height ratio was perceived as the most attractive for normal central incisors, although there was variability in the rater responses. There is a definite trend towards the extremes of very long or very short teeth being less attractive. The very ‘long’ central incisors, and those with tooth wear were perceived as unattractive. The investigators also found significant differences between the aesthetic perceptions of dentists, dental technicians and patients and also lack of agreement within each group, in particular within the patient group. The individual variability in patient response should be considered during treatment planning. Tooth size is described as the seventh key to ‘ideal’ dental occlusion, the other six morphological characteristics of an ‘ideal’ occlusion represented as Andrew’s six keys (i.e. Class I molar relationship, correct crown angulation and inclination, no rotations, no spaces and a level curve of Spee) (see Chapter 22). The presence of a tooth size discrepancy will either result in a spaced dentition or a less than ideal dental occlusal relationship. For ‘ideal’ dental aesthetics, the anterior teeth must be proportional in size as described above. Additionally, for ‘ideal’ dental occlusion, the maxillary and mandibular teeth must have a certain proportionate relationship in terms of size. It will not be possible to achieve an ‘ideal’ occlusion if individual teeth or groups of teeth in the maxillary or mandibular arches are either too large or too small compared to their antagonists in the opposing dental arch. Such a discrepancy is termed tooth size discrepancy. Evaluation of tooth size is an important part of clinical diagnosis. Tooth size analysis (also termed a Bolton analysis after its development in 1958 by the orthodontist Wayne Bolton) may be undertaken by measuring the mesiodistal widths of either the anterior teeth (canine‐to‐canine) or the entire arch (first molar to first molar, excluding second and third molars).21 A table of standard values (Table 24.1; based on Caucasian values) lists the summed tooth width value in the opposing arch that is ideally related to the measured value, i.e. it is used to compare the summed widths of the maxillary to the mandibular anterior teeth (anterior Bolton ratio) or the summed widths of the entire maxillary to the mandibular arch (overall Bolton ratio).22 The difference between the ‘ideal’ value from the standard table and the actual measured dental width in the arch with the excess value provides an estimate in millimetres of the extent of tooth size discrepancy. It has been demonstrated that a significant number of patients have a tooth size discrepancy of greater than 2 mm, which is clinically significant as it may affect the dental occlusion. Additionally, simple visual estimation has been shown to be inaccurate at determining a tooth size discrepancy.23 Table 24.1 Tooth size analysis (Bolton analysis) standard table of values
Chapter 24
Dentogingival Aesthetics
Introduction
Anatomy
The concept of ‘biological width’
Clinical evaluation
Tooth shape
Theories of ‘ideal’ tooth shape



Tooth size
Width‐to‐height ratio of maxillary central incisor crown

Seventh key and dental occlusion
Tooth size analysis
Maxillary anterior 3–3 summed widths (mm)
Mandibular anterior 3–3 summed widths (mm)
Maxillary total 6–6 summed widths (mm)
Mandibular total 6–6 summed widths (mm)
40
30.9
86
78.5
41
31.7
88
80.3
42
32.4
90
82.1
43
33.2
92
84.0
44
34.0
94
85.8
45
34.7
96
87.6
46
35.5
98
89.5
47
36.3
100
91.3
48
37.1
102
93.1
49
37.8
104
95.0
50
38.6
106
96.8
51
39.4
108
98.6
52
40.1
110
100.4
53
40.9
54
41.7
55
42.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







