Deltopectoral Flap
Although this flap (see Fig. 12.1a , 5) is credited to Bakamjian (1965), it was first mentioned in the German literature during the 1900s, and in the American literature in the early 2000s. Once commonly used, the deltopectoral flap has now been largely superseded by the pectoralis major island flap and free flaps.
Flap type:
Fasciocutaneous flap of the random pattern type (see Fig. 1.2 ).
Flap components:
Skin, subcutaneous fat, muscular fascia.
Use:
As a regional transposition flap.
Vascular supply:
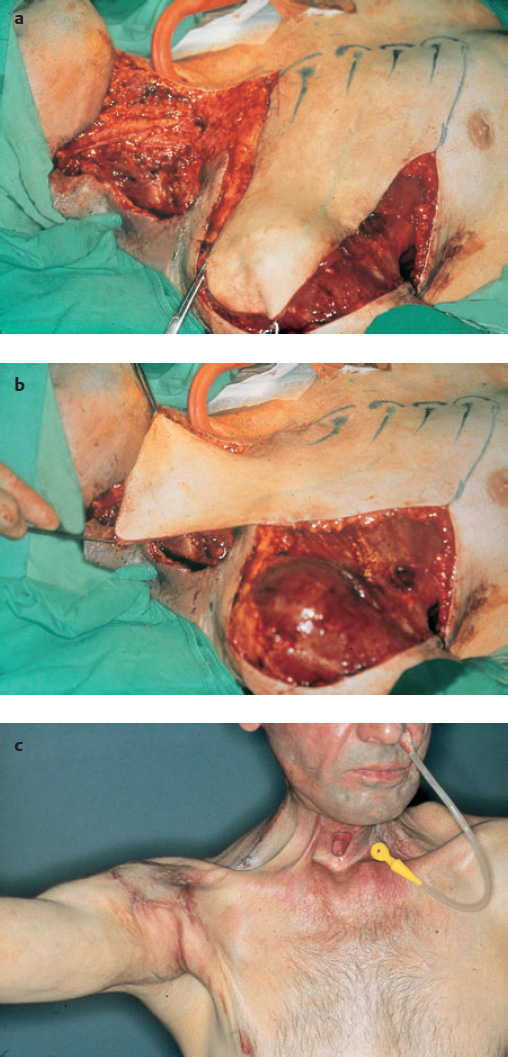
First through fourth perforating branches of the internal thoracic artery (internal mammary artery) ( Fig. 13.1a ).
Position:
Supine.
Flap size:
Width 8 to 12 cm, length 18 to 22 cm (the flap can be extended to the shoulder) ( Fig. 13.1a, b ).
Flap elevation:
The flap is designed larger than the size of the ablative defect. When the flap is raised, the fascial layers of the pectoralis major and deltoid muscles should be taken with the flap because they transmit the perforating branches. Care is taken not to kink the flap or rotate it excessively when suturing it into the defect. As much of the donor defect as possible is closed directly, and the rest is split-skin grafted. No pressure should be placed on the flap during the first few postoperative days, and the chest, shoulder, and neck should be immobilized. Adequate wound drainage should also be maintained, and any hematomas under the flap should be evacuated without delay.
Indications and advantages:
The deltopectoral flap is most commonly transferred upward to close postirradiation fistulas and resurface large cutaneous defects in the neck ( Fig. 13.1a, c ), especially in cases where the myocutaneous pectoralis major island flap is no longer available.
The vascular supply is constant.
The flap is easy to expose and dissect.
The flap provides ~250 cm2 of skin.
The flap has an arc of ~45° to 135°.
Disadvantages and complications:
When a large flap is raised, split-skin grafting of the donor site is required.
There may be an unfavorable cosmetic result, owing to exposed scars.
The flap has a significantly lower survival rate in patients who are emaciated, have undergone radiation therapy, or have severe cardiovascular problems. In these cases, there should be a delay before the transfer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree