Introduction442
INTRODUCTION
Type
Important features
Epidermal
Epidermal keratinization; keratohyaline granules
HPV-related
Either intracytoplasmic inclusions and vacuolar keratinous changes or verrucous lining (papillated and/or digitated) with hypergranulosis
Tricholemmal
Tricholemmal keratinization; cholesterol clefts; sometimes calcification
Onycholemmal
Cysts of nail bed, no granular layer; contain onycholemmal keratin and calcification
Hybrid
Outer epidermal and inner tricholemmal keratinization; other combinations may occur
Hair matrix
Basaloid cells with luminal squamous maturation
Cystic panfolliculoma
Infundibular lining; basaloid germinative cells, bulbs, matrical, and trichohyalin differentiation
Pigmented follicular
Epidermal-like; luminal pigmented hairs
Cutaneous keratocyst
Corrugated configuration; no granular layer; may contain vellus hairs
Vellus
Multiple; epidermal-like; luminal vellus hairs
Steatocystoma
Multiple; sebaceous glands in and adjoining wall; may contain vellus hairs
Milium
Small epidermal cyst with thinner wall
Comedonal cyst
Cystic hair follicle with keratinous material; open or closed
Eccrine hidrocystoma
Two layers of cuboidal epithelium
Apocrine cystadenoma
Columnar cells with decapitation secretion; basal myoepithelial cells
Bronchogenic
Mostly midline; respiratory epithelial lining; sometimes smooth muscle and mucous glands
Branchial
Lateral neck; stratified squamous and inner respiratory epithelial lining; heavy lymphoid tissue in wall
Thymic
Respiratory and/or squamous lining; Hassall’s corpuscles in wall
Cutaneous ciliated
Lower limb of females; ciliated columnar or cuboidal lining
Median raphe
Ventral surface penis; pseudostratified columnar epithelium
Dermoid
Periorbital or midline; epidermal-like with attached pilosebaceous structures; sometimes smooth muscle in the wall
APPENDAGEAL CYSTS
EPIDERMAL (INFUNDIBULAR) CYST
Histopathology
HPV-RELATED EPIDERMAL CYSTS
Histopathology1.56.60. and 65.
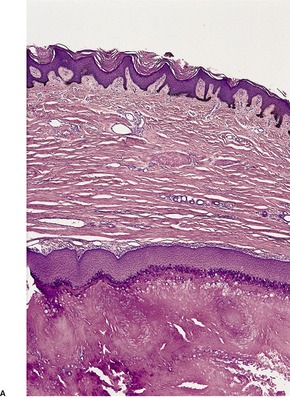
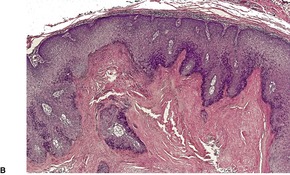
Fig. 16.1
PROLIFERATING EPIDERMAL CYST
Histopathology
TRICHOLEMMAL (SEBACEOUS, ISTHMUS-CATAGEN) CYST
Histopathology1. and 80.
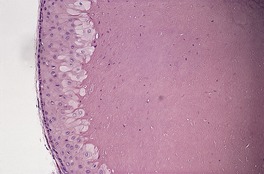
Fig. 16.2
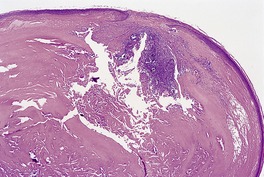
Fig. 16.3
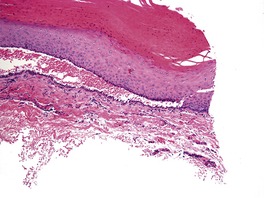
Fig. 16.4
PROLIFERATING AND MALIGNANT TRICHOLEMMAL CYST
Histopathology
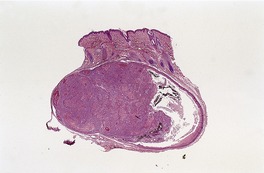
Fig. 16.5
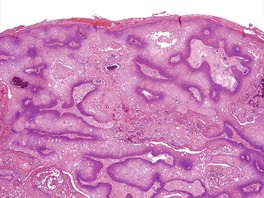
Fig. 16.6
ONYCHOLEMMAL CYST
Histopathology118
MALIGNANT ONYCHOLEMMAL CYST
Histopathology
HYBRID CYST
HAIR MATRIX CYST
Histopathology
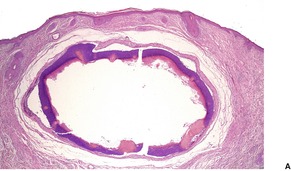
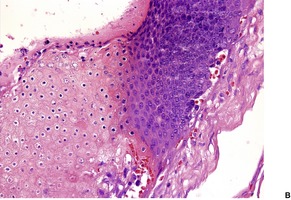
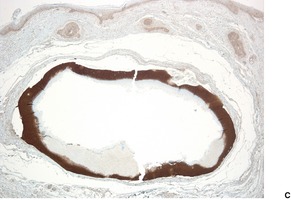
Fig. 16.7
CYSTIC PANFOLLICULOMA
Histopathology133
PIGMENTED FOLLICULAR CYST
Histopathology
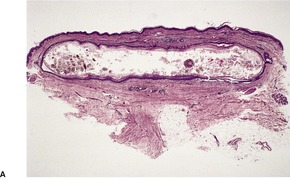
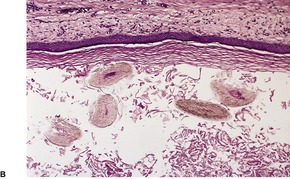
Fig. 16.8
CUTANEOUS KERATOCYST
Histopathology142
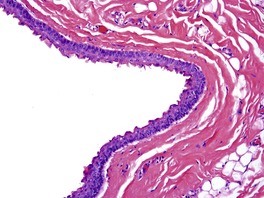
Fig. 16.9
VELLUS HAIR CYST
Histopathology147

Fig. 16.10
STEATOCYSTOMA MULTIPLEX
Histopathology
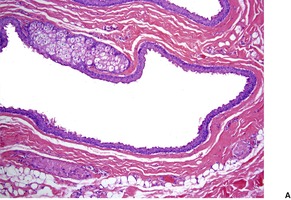
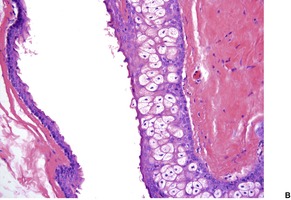
Fig. 16.11
Electron microscopy
MILIUM
Histopathology
COMEDO/COMEDONAL CYST
Histopathology
ECCRINE HIDROCYSTOMA
Histopathology
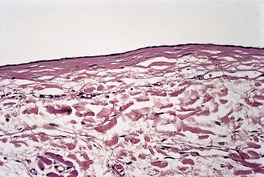
Fig. 16.12
Electron microscopy
APOCRINE HIDROCYSTOMA
Histopathology
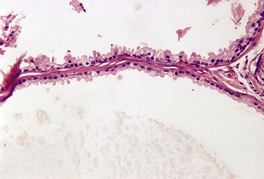
Fig. 16.13
Electron microscopy
DEVELOPMENTAL CYSTS
BRONCHOGENIC CYST
Histopathology
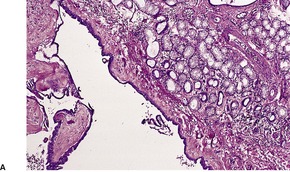
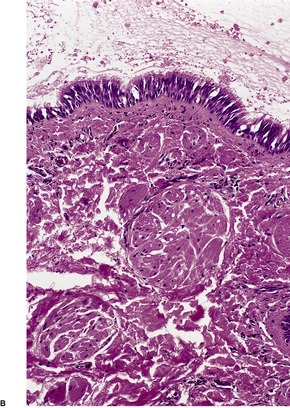
Fig. 16.14
BRANCHIAL CLEFT CYST
Histopathology
THYROGLOSSAL CYST
THYMIC CYST
Histopathology
CUTANEOUS CILIATED CYST OF THE LOWER LIMBS
Histopathology
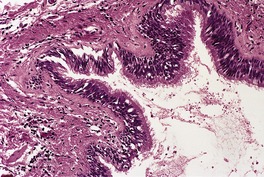
Fig. 16.15
VULVAL MUCINOUS AND CILIATED CYSTS
Histopathology
MEDIAN RAPHE CYST
Histopathology312
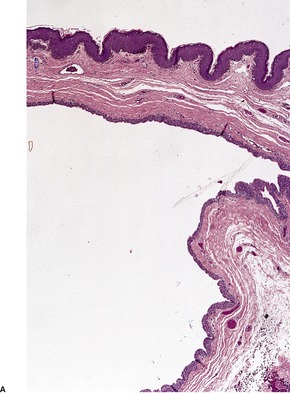
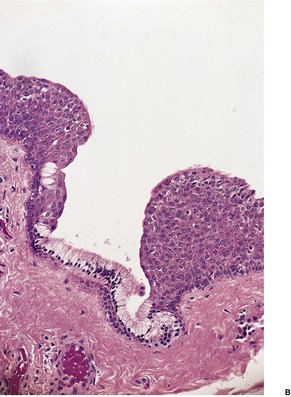
Fig. 16.16
DERMOID CYST
Histopathology325
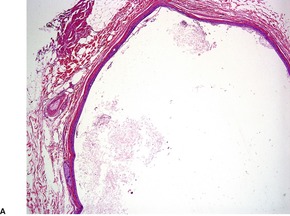
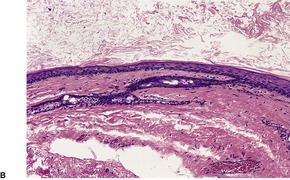
Fig. 16.17
CYSTIC TERATOMA
Histopathology
OMPHALOMESENTERIC DUCT CYST
Histopathology
MISCELLANEOUS CYSTS
PARASITIC CYSTS
PHAEOMYCOTIC CYSTS
DIGITAL MUCOUS CYST
MUCOUS CYST (MUCOCELE)
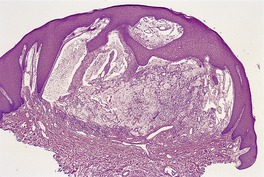
Fig. 16.18
METAPLASTIC SYNOVIAL CYST
Histopathology348. and 349.
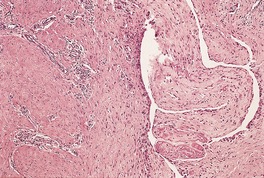
Fig. 16.19
PSEUDOCYST OF THE AURICLE
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cysts, sinuses, and pits
Appendageal cysts442
Epidermal (infundibular) cyst442
HPV-related epidermal cysts443
Proliferating epidermal cyst443
Tricholemmal (sebaceous, isthmus-catagen) cyst443
Proliferating and malignant tricholemmal cyst444
Onycholemmal cyst445
Malignant onycholemmal cyst446
Hybrid cyst446
Hair matrix cyst446
Cystic panfolliculoma446
Pigmented follicular cyst447
Cutaneous keratocyst447
Vellus hair cyst447
Steatocystoma multiplex448
Milium449
Comedo/comedonal cyst449
Eccrine hidrocystoma449
Apocrine hidrocystoma449
A cyst is an enclosed space or abnormal sac within a tissue, usually containing fluid or semisolid matter and lined by epithelium. Cysts are usually classified on the basis of their pathogenesis. In the skin, the most important cysts are derived from the dermal appendages as retention cysts. The developmental cysts, which result from the persistence of vestigial remnants, are much less common. The term ‘pseudocyst’ is sometimes applied to cyst-like structures without an epithelial lining. The important histological features of the various cutaneous cysts are shown in Table 16.1. A detailed review of dermal cysts was published in 2007. 1
A sinus is a tract or recess lined by epithelium or granulation tissue. In contrast, a cutaneous pit is a small depression in the epidermal surface.
The frontal mucocele that presented as a subcutaneous cyst on the forehead defies classification. 2
Epidermal cysts are solitary, slowly growing cysts with a predilection for the trunk, neck, and face. They measure 1–4 cm or more in diameter, although larger variants have been reported.3. and 4. A giant cyst is one over 5 cm in diameter. 5 Multilocular giant cysts also occur. 6 Epidermal cysts are usually located in the mid and lower dermis but they do not shell out like the tricholemmal cyst. There is often a surface punctum.
They are thought to be derived from the pilosebaceous follicle, but in non-hairbearing skin, they may arise from implantation of the epidermis, 7 particularly on the palms and soles8. and 9. and in the subungual region.10. and 11. Implantation of epidermis is the likely mechanism involved in the formation of the extremely rare midline cysts of the scalp, that are present at birth. 12 Eccrine ducts may rarely give rise to epidermal cysts,13. and 14. particularly on the soles, 15 in association with HPV-60 infection (see below). Epidermal cysts have also developed following chronic dermabrasion16 and photodynamic therapy, 17 and at the site of healed herpes zoster. 18 Multiple cysts may be found, sometimes in association with Gardner’s syndrome.19.20.21.22. and 23. They have been reported in mycosis fungoides. 24
Epidermal cysts may become infected and this may be followed by rupture of the cyst, usually into the dermis. Rupture can be detected by ultrasonography. 25 Cultures of infected cysts have grown Staphylococcus aureus or a mixed growth of organisms.26. and 27. However, a more recent study has shown that the microbiological milieu of inflamed and uninflamed cysts is the same, calling into question the traditional view that bacterial infection is the etiology of the inflammation in epidermal cysts. 28 There is a predominance of anaerobes in infected cysts in the genital and perineal regions. 26 Secondary infection by a dermatophyte has been reported. 29
Epidermal cysts are lined by stratified squamous epithelium showing epidermal keratinization, that is, the formation of keratohyaline granules and flattened surface epithelium. As such, they are thought to be derived from or to mimic the infundibular portion of the hair follicle. Rupture of a non-inflamed cyst will produce a localized foreign body granulomatous reaction in the adjacent dermis, while rupture of an inflamed cyst usually results in a heavy inflammatory cell infiltrate in the adjacent dermis, sometimes with destruction of the cyst wall in the process. Fibrosis usually occurs subsequently.
The rare finding of epidermal (infundibular) cysts of the ear which contained vellus hairs and with intervening severe solar elastosis (akin to Favre–Racouchot syndrome) has been proposed as a new dermatoheliosis. 30
Several histological variations in the epidermal lining have been reported. These include focal epidermal proliferation, 31 a seborrheic keratosis-like change, 32 basal hyperpigmentation and melanin incontinence (seen in black patients),33. and 34. melanophagic proliferation, 35 focal pilomatrixoma-like changes (usually in kindreds with Gardner’s syndrome),20.36. and 37. clear cell change, 38 cornoid lamellation, 31 epidermolytic hyperkeratosis,31. and 39. histological changes of Darier’s disease, 40 pyogenic granuloma formation, 41 Paget’s disease, 31 basal cell carcinoma, 31 mycosis fungoides, and Bowen’s disease. 42 Small papillary projections of follicular germinative cells emanating from the basal layer of the cyst wall are a rare occurrence. 43 Some of these projections may branch and form a reticulate pattern. The term ‘trichoblastic infundibular cyst’ has been suggested for this histological variant. 43 Melanoma in situ has been reported within the epithelial lining of a cyst, in contiguity with an adjacent malignant melanoma of epidermal origin. 44 The only variations in cyst contents that occur are the formation of spherules of keratin which are closely packed and uniform in dimensions, 45 and calcification, a common occurrence in cysts on the scrotum, where the cysts are sometimes multiple. 46 Specific histological features are usually seen in HPV-related cysts (see below). In a study of epidermal cysts of the sole, most showed foci of parakeratosis and focal lack of a granular layer, particularly in the upper portion of the cyst wall. 47 The cysts contained compact orthokeratotic material. The HPV status of these cysts was not obtained, but the histology of these cysts is remarkably similar to those described for HPV-related cysts (see below). Epidermal cysts express keratin 10 (K10), filaggrin48. and 49. and some members of the S100 protein family. 50 Cases of malignant transformation,51.52. and 53. reported in the older literature, have been questioned as some, at least, represent proliferating tricholemmal cysts (see p. 444) or proliferating epidermal cysts (see below). Cases of unequivocal squamous cell carcinoma arising in epidermal cysts have been reported. 54 Despite the low risk of malignant transformation, it is generally agreed that all suspected cysts should be submitted for histological examination. 55
Three distinctive, but rare, types of epidermal cyst have been reported in association with human papillomavirus infection. The first type, reported initially in Japan in 1986, usually involves pressure points on the plantar surface of the feet.56. and 57. Other sites are rarely involved.58. and 59. Lesions are usually solitary. HPV-60 has been demonstrated in most cases; 60 HPV-57 is rare. 59 Eccrine ductal structures are sometimes noted in the cyst wall, suggesting that HPV infection of eccrine ducts may have a pathogenetic role in some cases.60. and 61. However, immunostaining with monoclonal antibodies against various cytokeratins does not support this view.62. and 63. These conflicting findings may have been resolved. 64 It appears that these cysts express cytokeratin immunoreactivity identical to that of suprabasal layers of the epidermis resulting from epidermoid metaplasia of superficial eccrine ducts. 64 Epidermal implantation may also be involved in the pathogenesis.62. and 63.
In the second type (verrucous epidermal cysts), an HPV genome produces verrucous changes in the epithelial lining.65.66. and 67. One report demonstrated HPV-20 and HPV-34, which are epidermodysplasia verruciformis-associated strains. 68 The cysts do not usually involve the palms or soles.69. and 70.
In the third type, a cystic structure mimicking molluscum bodies, developed on the big toe. 71 It resulted from HPV-1 infection. Implantation of a fragment of HPV-infected epidermis was thought to be the mechanism involved in its formation. 71
The DNA of HPV-8 and of HPV-6 have been demonstrated within biopsy specimens of three cysts from a patient with epidermodysplasia verruciformis. 72 The patient had many other cysts which were not tested for the presence of HPV. 72
Epidermal cysts associated with HPV-60 infection are well-demarcated cysts in the dermis continuous with the overlying epidermis at the top of the cyst. Scattered keratinocytes in the upper layers of the epithelial lining contain intracytoplasmic, eosinophilic inclusions.73. and 74. In addition, vacuolar structures are present in the keratinous (horny) material within the cyst. Parakeratotic nuclei are often present in this keratinous material. Ductal structures expressing carcinoembryonic antigen (CEA) may be found in the cyst walls. 61 In HPV-related cysts arising away from palmoplantar surfaces, no histopathological feature has been shown to be predictive for the presence of HPV-60. 59
In the HPV-related verrucous cysts, there is an epidermal cyst lined by a papillated and/or digitated epithelium with focal, prominent hypergranulosis and irregular keratohyaline granules (Fig. 16.1). 65 Squamous eddies, reminiscent of those seen in inverted follicular keratosis, are often present in the epithelial lining. Vacuolated keratinocytes, resembling koilocytes, have been present in some cases. 67
(A) HPV-related epidermal cyst. (B) The lining has a papillated appearance. (H & E)
In a series of 96 cases of proliferating epithelial cysts published in 1995, 63 were of tricholemmal type and 33 of epidermal type. 75 The tricholemmal variants had a predilection for females (71% of cases) and the scalp (78% of cases), while the proliferating epidermal cysts had a male preponderance (64%) and a more widespread distribution involving the pelvic and anogenital region as well as the scalp, upper extremities, and trunk. 75 Carcinomatous change developed in 20% of the proliferating epidermal cysts.
Proliferating epidermal cysts are subepidermal cystic tumors that often connect with the overlying epidermis by a narrow opening or through a dilated hair follicle. 75 An underlying epidermal cyst is often present, although this constitutes only a small part of the lesion. The lesion consists of multilocular cystic spaces containing keratinous material or proteinaceous fluid. The proliferating epithelium, which may show squamous eddies, extends into the adjacent stroma but there is usually still some circumscription. The squamous cells may have copious pale cytoplasm. Epidermal-type keratinization is a prerequisite for the diagnosis. The degree of cellularity and atypia is variable. 75 Carcinomatous change is characterized by infiltration into the surrounding dermis and subcutis, marked nuclear atypia, pleomorphism, and frequent mitoses.
Tricholemmal (trichilemmal) cysts are also known as isthmus-catagen cysts in some parts of the world, reflecting the similarity of the cyst lining to the isthmic portion of the follicle and the epithelium of the lower segment of a follicle in late catagen. 76 Clinicians have been slow to embrace this term and it is likely to be decades, or longer, before it attains worldwide acceptance. Pilar cyst has also been used to describe this cyst. They are found as solitary or multiple intradermal or subcutaneous lesions with a predilection for the scalp. They are mostly asymptomatic. 77 There is a female preponderance. There is no punctum and the cysts easily shell out at removal. Familial cases, often with multiple cysts, occur and some of these have an autosomal dominant inheritance. 78
The term ‘trichilemmal cyst nevus’ has been used for the occurrence of multiple cysts arranged in a band-like pattern associated with multiple filiform hyperkeratoses and comedo-like plugs. 79 This may be yet another variant of organoid nevus (nevus sebaceus). 79
The cysts are smooth with a cream to white wall and similarly colored, semisolid, cheesy contents.
The cysts are lined by stratified squamous epithelium showing tricholemmal keratinization in which the individual cells increase in bulk and vertical diameter towards the lumen (Fig. 16.2). This usually occurs without the formation of keratohyaline granules and resembles that seen in the external root sheath in the region of the follicular isthmus. 81 There is an abrupt change into the eosinophilic-staining keratin within the lumen. Cholesterol clefts are common in this keratinous material and about one-quarter will show focal calcification of the contents. Tricholemmal cysts express both keratin 10 (K10) and 17 (K17). 48About 10% have focal inflammation but this differs from that seen in epidermal cysts. In tricholemmal cysts, there is a break in the wall with entry into the cysts of inflammatory cells and fibroblasts with subsequent organization (Fig. 16.3). Irregular hyperplasia of the epithelial lining may be a consequence of this. Sebaceous and apocrine differentiation have been reported in the wall. 82 In one case Merkel cell carcinoma in situ developed in the wall of a tricholemmal cyst. 83
Tricholemmal cyst (sebaceous cyst). It is lined by stratified squamous epithelium exhibiting tricholemmal keratinization. (H & E)
Tricholemmal cyst with ‘rupture’ and ingrowth of inflammatory cells and granulation tissue. (H & E)
A verrucous variant of tricholemmal cyst has been reported. 84 HPV common antigens were demonstrated in the nuclei of the lining cells in this case. 84
Sometimes, the outermost epithelial portion of the cyst wall separates from the remainder of the cyst. 76 Focal separation is more common than complete splitting (Fig. 16.4). The retained basal epithelium may mimic an apocrine hidrocystoma or even a vascular malformation. 76
Tricholemmal cyst with splitting of the outer part of the wall. In some areas only a thin layer of cells was present, mimicking a hidrocystoma. (H & E)
Under polarized light, the perpendicularly oriented bundles of tonofibrils can be seen in the lining epithelial cells, a feature of tricholemmal keratinization. 85 This mirrors the electron microscopic findings of an increase of filaments in the maturing cells which aggregate to form larger fibrillary bundles. Keratohyaline granules are not usually seen.
Although usually solid or only partly cystic, proliferating and malignant tricholemmal cyst is considered here because a spectrum of cases is observed, ranging from a tricholemmal cyst with minimal epithelial proliferation to a lesion with gross epithelial hyperplasia which is only minimally cystic and which may simulate a squamous cell carcinoma.75. and 86. Ackerman and colleagues believe that a proliferating tricholemmal cyst (pilar tumor) is a variant of squamous cell carcinoma. They use the term ‘proliferating tricholemmal cystic squamous-cell carcinoma’ for such cases.87. and 88. This view has not yet received wide acceptance, 89 and, indeed, the cytokeratin profile of these tumors differs from that of control squamous cell carcinomas. 90 This entity was first described by Wilson Jones as a proliferating epidermoid cyst. 91 Subsequent reports have not always made a distinction between proliferating tricholemmal cyst and proliferating epidermal cyst (see above).
The tumors are large, measuring 2–10 cm or more in diameter. They are sometimes exophytic and even ulcerated. 92 They are most commonly found on the scalp of middle-aged or elderly females. 75 The extremities are rarely involved.75. and 93. Recurrence after excision and malignant transformation are both uncommon;94.95. and 96. metastatic spread is very rare.95.97.98.99.100. and 101. They may develop in organoid nevi, 102 but most arise de novo or in a pre-existing tricholemmal cyst.92. and 103. HPV-21 was present in one malignant tumor in a patient with epidermodysplasia verruciformis. 104
Complete surgical excision is the treatment of choice. Mohs surgery has also been used to treat this lesion. 105
There is a lobular proliferation of squamous cells, often with some peripheral palisading and sometimes showing focal areas of vitreous membrane formation. There may be focal cystic areas or remnants of a more obvious tricholemmal cyst at one margin (Fig. 16.5). The lesions are usually well circumscribed. Nests of squamous cells may extend into the adjacent connective tissue, simulating squamous cell carcinoma, but the proliferation of nests is mostly inwards into the cyst (Fig. 16.6). This contrasts with the outward extension of nests seen in proliferating epidermal cysts.
Proliferating tricholemmal cyst. An early lesion with evidence of a pre-existing cyst at one edge. (H & E)
Proliferating tricholemmal cyst. This is part of a large tumor in which nests of squamous epithelium extend into the adjacent dermis. (H & E)
There are typical areas of tricholemmal keratinization and, in some cases, focal epidermal keratinization as well. There may also be vacuolated cells, variable cellular atypia, 106 focal necrosis, squamous eddies, individual cell keratinization, and scattered mitoses. Sebaceous and acrosyringeal differentiation were noted in one case. 107 A spindle cell component has also been described.108. and 109. Features favoring the diagnosis of proliferating tricholemmal cyst over squamous cell carcinoma include the presence of tricholemmal keratinization, cyst formation, calcification and the absence of a premalignant epidermal lesion. 110 Aneuploidy does not always assist in the assessment of malignancy as this feature can be present in proliferating tricholemmal cysts.111.112. and 113. The diagnosis of a malignant proliferating tricholemmal tumor usually requires the identification in some areas of an underlying benign component. 94 It also requires the presence of extensive cellular atypia and invasion, sometimes focal, of adjacent structures.95. and 114. Other criteria that have been suggested as markers of malignancy include non-scalp location and size greater than 5 cm. 101 Uncommonly, a spindle cell carcinoma forms the malignant component. 115 In one case the spindle cells were positive for vimentin, but not for keratin, epithelial membrane antigen, or S100 protein. 116 Stromal desmoplasia may be present in areas of malignant transformation. There is loss of CD34 immunostaining in some malignant lesions, 113 but it is retained in others. 90
Electron microscopy has confirmed the presence of areas of tricholemmal keratinization. 117
Subungual onycholemmal cysts, also known as subungual epidermoid inclusions, are an uncommon lesion occurring in the dermis of the nail bed. 118 There may be associated onychodystrophy, clubbing, ridging, thickening, pigmentation, or no change in the nail plate. 118
There are free-lying cysts within the dermis of the nail bed although they appear to form by elongation of the rete ridges with cyst formation and the subsequent pinching off of the connection to the nail bed epithelium. The cysts contain onycholemmal keratin and calcification. There is no granular layer.
Two cases of malignant onycholemmal cysts have been reported. The terms used have been ‘malignant proliferating onycholemmal cyst’ and ‘onycholemmal carcinoma’.119. and 120. They presented as a slowly growing tumor of the nail unit. 119 It was thought to have arisen from a pre-existing subungual keratinous cyst. The lesion penetrated the underlying phalangeal bone.
The tumor is composed of small keratinous cysts with abrupt central keratinization and of solid nests and strands of atypical keratinocytes. 119
A hybrid cyst is one in which the lining of the upper portion shows epidermoid keratinization similar to an epidermal cyst, while the lower portion shows tricholemmal keratinization similar to that seen in a tricholemmal cyst. 121 There is a sharp transition between the two types of lining. A hybrid cyst should not be confused with a tricholemmal cyst showing very focal formation of a granular layer, which may be found in 10% of cases. 122
The term ‘hybrid cyst’ has been expanded to include any follicular cyst with two different types of epithelial lining. 123 In addition to those just described with epidermal (infundibular) and tricholemmal differentiation, cysts may be found with epidermal and pilomatrical features (particularly in Gardner’s syndrome), tricholemmal and pilomatrical differentiation, 124 pilomatrical and steatocystoma features, 125 epidermal and apocrine changes,126. and 127. and also eruptive vellus hair cyst features with either steatocystoma, epidermal or tricholemmal change.123. and 128. A hybrid follicular cyst with some features of those seen in Gardner’s syndrome has now been seen in a patient with myotonic dystrophy. 129 A vellus hair cyst combined with an epidermal cyst and a benign melanocytic nevus has been reported. 130
In a series of 15 cases of hybrid cysts reported from Japan nearly half the cases occurred on the scalp and face. The most frequent histological type (60%) was the combination of epidermal (infundibular) and tricholemmal cysts. 131 A hybrid cyst of the parietal scalp has been associated with perforation of the skull, presumably from long-term pressure on the bone. 132
The hair matrix variant of epidermal cyst is seen more often in children and young adults. There is some resemblance to the pattern of differentiation seen in pilomatrixomas.
The cyst wall is composed of several layers of basaloid cells that mature to squamoid cells near the lumen (Fig. 16.7). This pattern recapitulates that seen in the normal hair matrix and cortex. Small cystic spaces are often present within the cyst wall. The lumen contains amorphous, keratinous material. If rupture occurs, a florid granulomatous reaction develops in the surrounding dermis.
(A) Hair matrix (matrical) cyst. (B) Matrical differentiation is present in the cyst wall. (H & E) (C) There is strong staining for β-catenin. (Immunoperoxidase stain for β-catenin)
Panfolliculoma is an exceedingly rare follicular neoplasm with differentiation towards both the upper and lower segments of the hair follicle (see p. 763). 133 There is infundibular, isthmic, matrical, and papillae-like differentiation. There are some overlap features between a trichoblastoma and matricoma. Some lesions present clinically as cysts. Grossly, they may be cysts measuring 3–4 cm in diameter.
The cystic variant has a thin wall about 0.1 cm in thickness. It is lined by infundibular epithelium having a granular layer. Solid aggregates of dark follicular germinative cells are present. Bulbs and papillae form in these areas. Matrical differentiation and shadow cells, as well as trichohyalin granules, are seen. Cytokeratin 903 and CK5/6 stain the tumor cells, while Ber-EP4 labels the germinative cells but not the follicular papillae.
A rare, clinically pigmented cyst was first described in 1982.134.135.136. and 137. There are reports of a patient with multiple pigmented cysts.138. and 139. This entity should be distinguished from a pigmented epidermal cyst, in which melanin pigment is present in the wall of an epidermal cyst or in melanophages in the surrounding stroma. 34
The cyst is located in the dermis and has a narrow, pore-like opening to the surface. It contains laminated keratin as well as multiple, pigmented hair shafts (Fig. 16.8). Degenerating hair shafts may be present. 140 The cyst is lined by stratified squamous epithelium showing epidermal keratinization, but in addition the lining may show rete ridges and dermal papillae, features not seen in epidermal cysts. Both epidermal and tricholemmal keratinization were present in the cysts removed from one of the patients with multiple lesions. 138
(A) Pigmented follicular cyst. (B) The lumen of the cyst contains a number of pigmented hair shafts. (H & E)
Closely related is the occurrence of a small follicular cyst containing pigmented hair shafts arising in a melanocytic nevus. 141
Cutaneous cysts are a feature of the nevoid basal cell carcinoma syndrome (see p. 691). Usually these cysts are of epidermal type, but there are rare reports of patients with this syndrome in whom the cutaneous cysts resembled keratocysts of the jaw.142. and 143. They contained a thick brown fluid. There are reports of a cutaneous keratocyst arising independently of the nevoid basal cell carcinoma syndrome.144. and 145. It has been suggested that ‘isthmic-anagen cyst’ would be a more appropriate designation. 146
The cysts have a corrugated or festooned configuration with a lining of several layers of squamous epithelium, but with no granular layer. Lanugo hairs were present in one cyst. There is a superficial resemblance to steatocystoma multiplex (see below), but there are no sebaceous lobules in the wall.
The author uses the term sebaceous duct cyst for cysts with a corrugated lining but no sebaceous lobules of steatocystoma on routine sectioning (Fig. 16.9). They are not as rare as the paucity of reports would suggest. There is a possibility that rare sebaceous lobules would be found on complete sectioning of the cyst. Keratocyst is an acceptable alternative term but this term is usually associated with the cysts of the nevoid basal cell carcinoma syndrome.
Sebaceous duct cyst (keratocyst). There is a lining that resembles the sebaceous duct. (H & E)
Eruptive vellus hair cysts, first reported in 1977, 147 occur as multiple, small (1–4 mm), asymptomatic papules with a predilection for the chest and axillae of children or young adults.148. and 149. The number of cysts varies from 20 to 200. 150 They are also found on the face,151.152. and 153. neck, and extremities. Unilateral involvement of the face has been reported. 154 They may have an autosomal dominant inheritance or occur sporadically.155. and 156. Ectodermal dysplasia and oculocerebrorenal syndrome (Lowe’s syndrome – OMIM 309000) are rare associations.157.158. and 159. Spontaneous regression of the cysts has been reported, probably following the transepidermal elimination of the cyst contents. 160
Eruptive vellus hair cysts have been reported in patients with steatocystoma, suggesting that these two entities are in some way related;161.162.163. and 164. both may be derived from the sebaceous duct. 165 However, their pattern of keratin expression is different: vellus hair cysts express keratin 17 (K17), while steatocystomas express both keratins 17 (K17) and 10 (K10). 48 Milia can also occur in association with these two entities. 166 Trichostasis spinulosa may rarely coexist with eruptive vellus hair cysts. 167
An extraction technique, similar to that proposed for steatocystoma multiplex (see below), has been proposed. 168 Lasers have also been used in the management. 169
These small dermal cysts are lined by stratified squamous epithelium which may show focal tricholemmal as well as epidermoid keratinization. The lumen contains keratin and numerous transversely and obliquely sectioned vellus hair shafts (Fig. 16.10). These shafts are doubly refractile with polarized light. A rudimentary hair follicle may be attached to the wall. Hybrid cysts with features of both vellus hair cysts and steatocystoma are sometimes seen.123. and 163. There may be focal rupture of the cyst wall with a foreign body granulomatous reaction and associated dermal fibrosis and mild chronic inflammation.
Vellus hair cyst. The lumen of the cyst contains multiple small vellus hairs. (H & E)
Some cysts may show a connecting pore at the skin surface, the likely mechanism of the spontaneous regression mentioned above.
If the cyst contents are expelled through a small incision, and then placed in potassium hydroxide, the vellus hairs can be identified in a typical serpentine array. 150
Steatocystoma multiplex is characterized by multiple yellowish to skin-colored papules or cysts measuring from less than 3 mm in diameter to 3 cm or more. They may be found on the face,170.171.172.173.174. and 175. scalp,176.177. and 178. trunk, vulva, 179 axillae, and the extremities, 180 but they have a predilection for the chest. Rarely, they have a linear distribution. 181 They are mostly sporadic, but familial cases with autosomal dominant inheritance are well documented. Other abnormalities may be present in the inherited cases. 171 The occurrence of steatocystoma multiplex in Alagille syndrome may be fortuitous, 182 but not their occurrence in association with trichoblastomas and trichoepitheliomas. 183 Patients with only a solitary lesion (steatocystoma simplex) are seen rarely.179. and 184. The cysts usually present in adolescents as asymptomatic lesions, but infected cysts (steatocystoma multiplex suppurativum) may be painful.185. and 186. Steatocystoma is thought to represent a nevoid malformation of the pilosebaceous duct. Mutations in keratin 17, similar to those found in pachyonychia congenita, have been found in some patients with steatocystoma multiplex.187.188. and 189.
A modified surgical technique involving puncture of the cyst, evacuation of cyst contents, and extraction of the sacs through a small incision has been proposed as the method of choice for their removal. 190
The lining of the dermal cysts is usually undulating due to collapse of the cyst. It is composed of stratified squamous epithelium, only a few cells thick and without a granular layer. The characteristic feature is the presence of sebaceous glands of varying size in or adjacent to the wall (Fig. 16.11). A ribbon-like cord of epithelial cells connects the cyst with the epidermis, but this may not be seen in the plane of section. One pilar unit is associated with each cyst, and the cyst may contain one or more lanugo hairs. Large polygonal cells with abundant granular cytoplasm form part of the lining of the cyst on rare occasions. Such cells have the immunohistochemical characteristics of the macrophage/monocyte lineage. 178 Spherules (‘myospherulosis’), formed by masses of erythrocytes in the presence of oil-containing substances, have been reported in the lumen. 191 Smooth muscle has been noted in the wall. 192
(A) Steatocystoma multiplex. (B) Sebaceous glands are present within the cyst wall. (H & E)
Hybrid cysts with features of both steatocystoma and vellus hair cysts are sometimes seen;123.163.193. and 194. epidermal cysts may form a third component. 128 Cysts without sebaceous lobules in the wall resemble keratocysts. The author uses the term sebaceous duct cyst for these solitary lesions (see above). The presence of a sebaceous adenoma in the wall of a steatocystoma has been called a ‘steatosebocystadenoma’. 195
The keratinization takes place without the formation of keratohyaline granules, a feature which is characteristic of the sebaceous duct. 170
A milium is a small (1 or 2 mm in diameter) dermal cyst which may arise from the pilosebaceous apparatus or eccrine sweat ducts. 196 Milia may be seen in the newborn as congenital lesions or they may develop later in life secondary to dermabrasion, to the topical application of corticosteroids196 and to radiotherapy, and as a consequence of subepidermal blistering disorders such as porphyria cutanea tarda, epidermolysis bullosa dystrophica, polymorphic light eruption, 197 and second-degree burns. They have also been reported in association with discoid lupus erythematosus, 198 pseudoxanthoma elasticum, 199 healed leishmaniasis,200. and 201. regressing plaques of mycosis fungoides, 202 a congenital hemangioma, 203 and some inherited disorders. 204 One such syndrome is the Bazex–Dupré–Christol syndrome (follicular atrophoderma and basal cell carcinoma – OMIM 301845) which maps to Xq24–q27. The UBE2A gene has been proposed as a candidate gene. 205
Milia most commonly occur as multiple lesions on the cheeks and forehead, but they may involve the genitalia or other sites, depending on the predisposing lesion.206. and 207. A rare eruptive form208. and 209. and an erythematous plaque variant (milia en plaque) have been reported.204.210.211.212.213.214.215.216.217.218.219. and 220. Milia en plaque usually occurs in a periauricular distribution. 221 It has arisen in association with lupus erythematosus222 and in a renal transplant patient. 223
Treatment options for milia en plaque are limited, although spontaneous regression occurs occasionally. 220 Simple extraction or topical tretinoin are the most frequently tried options. 220 Oral etretinate has also been used successfully to treat milia en plaque. 224 Retinoids suppress the expression of involucrin and cytokeratins 6 and 16. Topical tretinoin has been used to treat eruptive milia. 225
The small cysts are lined by several layers of stratified squamous epithelium with central keratinous material, resembling a small epidermal cyst. They may be connected to a vellus hair follicle or eccrine sweat duct, usually the latter. 226 Milia differ from comedones, which are keratinous plugs in dilated pilosebaceous orifices. Closed comedones, which may be particularly prominent in the condition known as nodular elastoidosis with cysts and comedones (Favre–Racouchot disease),227. and 228. may superficially resemble milia. However, comedones are more likely to contain old hair shafts and laminated keratinous material containing numerous bacteria. 229 The term comedonal cyst has been used for comedones with cystic dilatation (see below). Some ruptured milia produce an unusually florid granulomatous reaction of foreign body type that has a distinctive appearance, even though the milium has been destroyed.
A comedo is an impaction of horny cells in the lumen of a sebaceous follicle. They may be open (‘blackhead’) with a wide patulous orifice, or closed (‘whitehead’) with a small orifice, not always seen in a random H & E section. They have been discussed earlier as a component of acne vulgaris (see. p. 401). Comedones are common in chloracne (see p. 402) and in the Favre–Racouchot syndrome (see p. 342), a rare variant of which appears to have been described on the ears. 30 Flexural comedones have been described recently in children. They were most common in the axillae (88%), but they were also found in the groin and antecubital fossa. 230 Most cases were unilateral. The term childhood flexural comedones was applied to the 40 reported cases; the number of cases in the report suggests that this entity is not uncommon. 230 The term idiopathic disseminated comedones refers to the occurrence of multiple comedones in a widespread distribution. Only one case appears to have been reported. 231
Comedones may be familial. 232 A familial form with dyskeratosis in the wall of the cysts has been called familial dyskeratotic comedones (see p. 670).
Comedones are follicular retention cysts. Although usually small, some deserve the appellation comedonal cyst.
A comedo is a cystically dilated hair follicle containing abundant keratinous material. As discussed above, they may have a patulous orifice (open comedones) or a narrow orifice, not always seen in plane of section (closed comedones). Severe solar elastosis accompanies those seen in the Favre–Racouchot syndrome. No criteria have been proposed for the designation ‘comedonal cyst’ as opposed to ‘comedo’.
Eccrine hidrocystomas are usually solitary lesions of the face, trunk or popliteal fossa, with a strong predilection for the periorbital area.233. and 234. Cases with multiple (up to 200 or more) lesions are well documented.235.236.237. and 238. There is a slight preponderance of adult females. Clinically, the lesions are usually translucent, pale blue, dome-shaped, cystic papules. The development of a squamous cell carcinoma in an eccrine hidrocystoma is a very rare complication. 239
The existence of this entity has been challenged; many, if not all of these lesions are now regarded as being of apocrine type, but cases continue to be reported. 240
The cysts are unilocular and situated in the dermis, often in close proximity to eccrine glands. The wall is composed of two layers of cuboidal epithelium with eosinophilic cytoplasm (Fig. 16.12). Sometimes the lumen contains small amounts of pale eosinophilic secretions. There is no evidence of decapitation secretion but this may simply be a consequence of marked flattening of the lining cells by the intraluminal contents.
Eccrine hidrocystoma. It has been suggested that such lesions are really of apocrine type. Attenuation of the lining may be responsible for loss of the ‘decapitation’ secretion. (H & E)
There are two cell layers with a peripheral basement membrane and extensive microvilli along the luminal border. 241 These findings are similar to those of the eccrine duct.
Apocrine hidrocystoma (apocrine gland cyst, apocrine cystadenoma) is regarded by some as an adenomatous cystic proliferation of apocrine glands and by others as a simple retention cyst. 242 Apocrine hidrocystomas are almost invariably solitary lesions, a few millimeters in diameter, on the head or neck of middle-aged to older adults. 243 A large variant has been described244 and patients with multiple lesions have been observed.245.246.247. and 248. Multiple cysts may be a marker of two rare inherited disorders, the Schöpf–Schulz–Passarge syndrome and a form of focal dermal hypoplasia. 247 Clinically, the lesions resemble eccrine hidrocystomas with a translucent or bluish hue. 249 Their contents are colorless or brown to black. Interestingly, they do not occur in the usual sites in which apocrine glands are found. 250 Examples of this include the tip of the finger, 251 and the extremities. 252 They may arise in an organoid nevus. 242 Cysts may also develop from the duct and secretory segment of Moll’s gland, a modified apocrine gland of the eyelid.247.253. and 254.
The cysts may be unilocular or multilocular with a lining of columnar epithelium with basal nuclei and an underlying flattened layer of elongated, basal myoepithelial cells. Characteristically, there is ‘pinching off’ (‘decapitation’) of the cytoplasm of the luminal border of the lining cells, typical of apocrine secretory activity (Fig. 16.13). Sometimes the epithelium is flattened, making distinction from eccrine hidrocystoma difficult.255. and 256. It is now thought that most eccrine hidrocystomas are of apocrine origin. In nearly half the cases there are local areas of hyperplastic epithelium with microcysts in the lining and intracystic papillary projections with a core of vascularized connective tissue. The presence of keratinizing squamous epithelium adjacent to apocrine epithelium occurs in one variant of hybrid cyst (see p. 446).
Apocrine cystadenoma. This bilocular cyst is lined by apocrine epithelium showing ‘decapitation’ secretion. (H & E)
The secretory cells may contain PAS-positive diastase-resistant granules. Carcinoembryonic antigen (CEA) may also be present in both apocrine and eccrine cystadenomas.
The basal myoepithelial cells and the secretory cells show abundant secretory granules, decapitation secretion, and usually annulate lamellae. 257
Included in this group are cysts derived from embryological vestiges such as the branchial cleft, thyroglossal duct, tracheobronchial bud, urogenital sinus, and müllerian structures. 258 Others arise along lines of embryological closure. The term ‘cutaneous ciliated cyst’ has been applied to those which have in common a ciliated columnar epithelial lining, but which have been given different names according to their topographical localization. 259 Included in this concept are bronchogenic cysts, cutaneous ciliated cyst of the lower limbs, branchial and thyroglossal cysts, and cutaneous endosalpingiosis. 260 The term is best restricted to the cutaneous ciliated cyst of the lower limbs (see p. 451).
Cystic lesions devoid of an epithelial lining may occur in association with heterotopic brain tissue (see p. 881). 261
A bronchogenic cyst is present at or soon after birth, most often in the midline near the manubrium sterni.259.262.263.264. and 265. It has been reported on the chin,266. and 267. the neck, and even the shoulder and scapular region;268. and 269. these latter examples are presumed to be derived from sequestrated cells of the tracheobronchial bud, although an equally valid argument can be made for a branchial origin for many of these cysts.270. and 271. They present as a cyst or as a draining sinus. Bronchogenic cysts are four times more common in males than in females. 272
The cysts are unilocular and situated in the dermis or subcutaneous tissues. They contain cloudy fluid.
The cysts are lined by ciliated and mucin-producing pseudostratified columnar or cuboidal epithelium (Fig. 16.14). Stratified squamous epithelium may be present in the outer part of the cyst in those presenting as a sinus on the skin surface. 273 Gastric mucosa of antral type has been reported in one bronchogenic cyst. 274 Smooth muscle and even mucous glands are found commonly in the wall, but cartilage is present only occasionally. There may be some inflammation and fibrosis adjacent to the cyst, but lymphoid follicles, common in the wall of branchial cleft cysts (see below), are very rare in bronchogenic cysts.275.276. and 277.Ectopic respiratory mucosa, without an associated cyst, is a rare finding in the skin.278. and 279.
(A) Bronchogenic cyst with a collection of mucous glands in the wall. (B) The lining is pseudostratified columnar with occasional goblet cells. There are smooth muscle bundles in the wall. (H & E)
Branchial cleft remnants present clinically as cysts, sinus tracts, skin tags, or combinations of these lesions.271.280. and 281. Those derived from the second branchial pouch are usually found along the anterior border of the sternomastoid muscle of children or young adults, while those of first pouch origin arise near the angle of the mandible or postauricular region. 282 They may be found at any depth between the skin and pharynx. Secondary infection may cause sudden swelling of the lesions.
The cysts contain turbid fluid, rich in cholesterol crystals. Squamous cell carcinoma is a rare complication in lesions of long standing.283. and 284.
The cysts are lined mostly by stratified squamous epithelium, but deeper parts may have a lining of ciliated columnar epithelium. A heavy lymphoid infiltrate invests the cyst or sinus wall, and this includes lymphoid follicles. Mucinous glands and cartilage are occasionally present in the wall; 270 thymic tissue has also been reported. 285
Branchial cleft anomalies differ from bronchogenic cysts by their location, the common occurrence of lymphoid follicles and stratified squamous epithelium, and the rarity of smooth muscle. 276
Most examples of thyroglossal cyst are deep lesions in the midline of the neck and therefore beyond the scope of this volume.171. and 286. There is one report of a depressed lesion in the midline of the neck, present since birth, which consisted of tubular glands lined by respiratory epithelium, opening on to the skin surface. 270 Deeper branching tubules penetrated into the underlying striated muscle. The lesion was presumed to be of thyroglossal duct origin. A cyst reported in the lateral neck, attached to the thyroid gland, was most likely a foregut remnant. It resembled, in part, a bronchogenic cyst, but the wall also contained pancreatic tissue. 287
Thymic cysts are rare cysts found in the mediastinum or neck. The cervical lesions usually present as painless swellings in children or adolescents.288.289. and 290. Thymic cysts are thought to arise from remnants of the thymopharyngeal duct, a derivative of the third pouch. They are most often found posterior to a lateral lobe of the thyroid, more often on the left-hand side.
The cysts are unilocular or multilocular and measure from 1 to 15 cm in diameter. The contents are variable, ranging from yellow-brown fluid to cloudy or gelatinous material. Cholesterol crystals may be present.
Rarely, carcinomas may arise in thymic cysts. 291
Thymic cysts are lined by one or more of the following epithelia: squamous, columnar, cuboidal, or pseudostratified columnar. Occasionally, the cyst is devoid of an epithelial lining and has a fibrous tissue lining only. The wall characteristically contains Hassall’s corpuscles and in addition there may be lymphoid tissue, cholesterol granulomas, and sometimes parathyroid tissue. 288
Thymic remnants, without cyst formation, have been reported in the skin of the neck. 292
The term ‘cutaneous ciliated cyst’ is sometimes applied to several varieties of developmental cysts that, although lined by ciliated epithelium, are of quite different origin (see above). It is mostly restricted to a rare cyst which arises on the lower extremities of women in the second and third decade.293.294.295. and 296. Rarely, it may occur at other sites such as the abdominal wall and umbilicus.297.298. and 299. The cysts are less than 3 cm in diameter. They have been thought to be of müllerian origin, but the occurrence of rare cases in males has raised the possibility of an origin from an eccrine sweat gland.300.301.302. and 303. Ciliated cysts in the perineal region of males are thought to be derived from embryonic remnants of the cloacal membrane.304. and 305. A perineal lesion has also been reported in a female. 306
In a case of cutaneous ciliated cyst removed from the scalp, estrogen and progesterone receptors were demonstrated in the nuclei of the lining cells. 307
The cyst is lined by ciliated cuboidal to columnar epithelium with pseudostratified areas (Fig. 16.15). Focal squamous metaplasia is sometimes present; mucinous cells are rare. 308 The cysts may be multilocular and there are often papillary projections into the lumen. Glandular and smooth muscle elements are absent. 309 Strong dynein positivity has been observed in the apical portion of the lining cells with immunohistochemistry. 306 This pattern is similar to normal salpingeal epithelium, support for a müllerian origin.
Cutaneous ciliated cyst. The cyst is partly collapsed with some infolding of the wall. The lining is ciliated. (H & E)
The epithelial lining cells express progesterone receptor and epithelial membrane antigen but not carcinoembryonic antigen. 297
Vulval mucinous and ciliated cysts are found in the vestibule of the vulva.310. and 311. They vary in size from 0.5 to 3.0 cm or more. Included among the cases reported have been several instances of Bartholin’s cyst. Vulval mucinous and ciliated cysts are presumed to be of urogenital sinus origin.
The cysts are lined by pseudostratified ciliated columnar epithelium and/or mucinous epithelium. There may be areas of squamous metaplasia.
‘Median raphe cyst’ is the preferred term for midline developmental cysts found at any point from the external urethral meatus to the anus, including the ventral aspect of the penis, the scrotal raphe, and the perineal raphe, but most commonly near the glans penis.312.313.314. and 315. They are usually solitary but multiple small papules in a linear arrangement may occur. 316 They are thought to arise as a result of defective embryological closure of the median raphe, but some may result from the anomalous outgrowth of the entodermal urethral lining (urethroid cyst).317. and 318. They are most commonly diagnosed in the first three decades of life. Abrupt onset of a median raphe cyst may be precipitated by local trauma or secondary infection. 319 Canals coursing longitudinally in the line of the median raphe are sometimes found. 320
Most raphe cysts are less than 1 cm in diameter. The contents are usually clear, but they may be turbid if there are abundant mucous glands in the wall.
Median raphe cysts are situated in the dermis, but they do not connect with the overlying surface epithelium. They are lined by pseudostratified columnar epithelium, which may be quite attenuated in some areas. Occasionally, mucous glands are present in the wall, but ciliated cells are rare.321. and 322. Pigmented cysts, resulting from the presence of melanocytes, have been reported. 323 In cysts situated near the meatus, the lining is usually of stratified squamous epithelium (Fig. 16.16).
(A) Median raphe cyst. (B) Islands of squamous epithelium are interspersed between mucin-secreting epithelium. (H & E)
Immunohistochemistry of two cases showed strong staining of the epithelial lining cells with CK7 and CK13 but not CK20. 324
Dermoid cysts are rare subcutaneous cysts of ectodermal origin found along lines of embryonic fusion, particularly at the lateral angle of the eye or the midline of the forehead or neck. 325 Involvement of the scalp, mouth, and penis is rare.326.327. and 328. Dermoid cysts arising in the midline of the dorsum of the nose frequently have an overlying fistula communicating with the skin surface and the underlying cyst, which is sometimes quite deep.329.330.331. and 332. The terms fistula of the dorsum of the nose and nasal dermoid sinus cyst are used for this superficial component.330. and 333. A tuft of hair usually protrudes from the central pit. If numerous sebaceous glands are present, the lesion may present as a yellowish plaque. 334 A similar dermal ‘sinus’ has been reported in the occipital region of the scalp, overlying an intracranial dermoid cyst. 335 The term congenital dermoid fistula of the anterior chest region has been used for yet another variant of this same process. 336
Dermoid cysts are usually asymptomatic masses present at birth, but inflammation, often secondary to trauma, may draw attention to a pre-existing lesion in an older person.
The cysts are unilocular structures between 1 and 4 cm in diameter, containing fine hair shafts admixed with variable amounts of thick yellowish sebum.
The case reported as multiple dermoid cysts on the cheek had some unusual features, although the authors stressed that their case was different to steatocystoma. 337
The subcutaneous cyst reported as a cystic teratoma has features of both a dermoid and bronchogenic cyst (see below). 338 The sacrococcygeal teratoma reported by Dhingra et al may have been a conjoint parasitic twin. 339
Dermoid cysts are lined by keratinizing squamous epithelium with attached pilosebaceous structures (Fig. 16.17). Non-keratinizing squamous epithelium with admixed goblet cells resembling conjunctival epithelium has been reported in orbital dermoid cysts. 340 Another rare finding is the presence of basaloid proliferations of the cyst wall, possibly representing primordial hair follicles. 341 Sebaceous glands may empty directly into the cyst, the lumen of which contains hair shafts and keratinous debris. Eccrine and apocrine glands, as well as smooth muscle, may be present in the wall of up to one-quarter of the cases. Partial rupture of the cyst, resulting in a local foreign body granulomatous reaction, may be found. Focal calcification is a rare finding.
(A) Dermoid cyst. (B) A pilosebaceous structure is attached to the cyst wall. (H & E)
The fistulous tract sometimes found in association with midline dermoids of the nose is lined by the same elements as are found in the cyst wall. 330 The dermoid fistula of the anterior chest (see above) was a thin sinus tract lined by stratified squamous epithelium with hair follicles and sebaceous glands arising from the lining. 336
Several cases of cystic teratoma of the skin have been reported in the English language literature.338.342. and 343. The lesions were present at birth. They have involved the glabellar region, 342 the back, 338 and the knee. 343
A diversity of tissue types may be present. One of the reported cases was composed of respiratory epithelium, thyroid, and nervous tissue as well as striated and smooth muscle. 342 Another case was lined by gastrointestinal mucosa, 343 while another resembled a dermoid cyst with the addition of areas lined by pseudostratified, ciliated epithelium with goblet cells and occasional seromucinous glands and some surrounding smooth muscle. 338
Omphalomesenteric duct cysts arise in the periumbilical area. 344 They may be associated with a Meckel’s diverticulum.
The cysts may be connected to the skin surface, with gastrointestinal mucosa adjoining the stratified squamous epithelium of the adjacent skin. The mucosa may be of gastric, colonic, or small bowel type. Smooth muscle may be present in the wall.
Parasitic cysts are considered in Chapter 29. The most important is cysticercosis, the larval form of Taenia solium, which may present as one or more subcutaneous cysts345 (see p. 646). Sparganosis may also present as a subcutaneous ‘cyst’ (see p. 647).
A digital mucous cyst is usually found as a tense cystic nodule at the base of the nail of a finger or thumb. A second type (myxoid cyst) overlies a distal interphalangeal joint. 347 The latter type resembles a ganglion while the former resembles focal mucinosis. Digital mucous cysts are considered in detail with other mucinoses (see p. 360).
Mucous cysts, found usually on the lower lip or buccal mucosa, result from the rupture of a duct of a minor salivary gland with extravasation of mucus. Large mucinous pools are formed with a variable inflammatory and fibroblastic response (Fig. 16.18). These lesions are considered with the mucinoses (see p. 362).
Mucocele. There is a large mucinous pool. There is no epithelial lining in these cysts. (H & E)
Metaplastic synovial cysts are intradermal or subcutaneous cysts lined by a membrane that resembles hyperplastic synovium.348.349. and 350. The lesions usually arise in surgical scars or at sites of trauma, 351 unrelated to joints or other synovial structures. 349 Cutaneous fragility and anomalous scarring may be the explanation for the cases that have developed in patients with Ehlers–Danlos syndrome.352. and 353. They are usually solitary. 354
The cyst lining resembles hyperplastic synovium with partly hyalinized synovial villi. Sometimes only slit-like spaces lined by synovium are present (Fig. 16.19). The cystic cavities may communicate with the surface epidermis.
Metaplastic synovial cyst. A slit-like cavity lined by synovium is present adjacent to an area of scar tissue in the dermis. (H & E)
Pseudocyst of the auricle is an uncommon, asymptomatic, non-inflammatory, intracartilaginous lesion affecting the upper half or third of the ear, most often in young or middle-aged males.355.356.357. and 358. It appears to be more common in men of Chinese or European ancestry. 359 Bilateral involvement has been reported. 360 There is usually no clearcut history of preceding trauma.361. and 362. An association with atopic dermatitis of the face and ears has been noted, but it is quite rare. 363 Ischemia has been suggested as a possible cause of the cartilaginous degeneration which is followed by the accumulation of yellowish fluid to form a pseudocyst. 364 The term ‘seroma’ has been used for a closely related entity in which the accumulation of fluid was thought on clinical grounds to be outside the cartilage. 365 Recurrence after treatment is not uncommon.366. and 367.






