When evaluating the face in thirds, the upper face, midface, and lower face, one may assume the lateral the temple, midface, and lateral mandible as the pillars of these subdivisions. Many of our facial aesthetic procedures address these regions, including the lateral brow lift, midface lift, and lateral face lift. As the use of facial fillers has advanced, more emphasis is placed on the correction of the temples, midlateral face, and lateral jaw line. This article is dedicated to these facial aesthetic pillars.
Key points
- •
Volumization of the temples is a safe and effective use of dermal fillers to decrease hollowness. This article describes injection technique and outcomes.
- •
Volumization and enhancement of the midface can restore a youthful look and achieve symmetry. This article addresses placement of the device and injection technique.
- •
Jawline augmentation can be effective with the correct placement and product or combination of products.
Temporal augmentation and rejuvenation
Treatment Goals and Planned Outcomes
In rejuvenation of the temples, the goal is to obtain a youthful and aesthetic result that is appropriate for each individual, in a safe and effective manner. For example, the temples of an individual with bony structures of the face and thin skin should have more of a concavity than an individual with a rounder face and thicker skin. The challenges that face the injector in this area include vascular structures, muscles of mastication, and emissary and diploic veins of the skull. The skin in this area could be thin in individuals needing treatment; thus, the product used could become visible if not placed appropriately.
Preoperative Planning and Preparation
Selection of an appropriate candidate is based on the trained eye of the injecting physician. Many patients may not be aware of the presence of hollowness in this area and it has to be brought up to them by the treating physician by the use of a mirror or photographs. At times, the treatment of this aesthetic unit is essential for a more balanced and youthful result. Photographs are essential using a superior oblique view ( Fig. 1 ). The patient needs to be prepped with an antiseptic solution. This preparation has become more important with observed infection that can occur in the face at times, often months later. One may consider decreasing the viscosity of the filler by using lidocaine. If there are any concerns about causing irregularities in thin-skinned individuals, this dilution is optimal. During the injection, one must plan on transitioning into the surrounding structures. For example, the temporal region transitions into the forehead at the temporal line and, if there is loss of volume medial to this, an optimal aesthetic outcome may necessitate gradual injection medially beyond the temporal line for a smooth transition.

Patient Positioning
The temporal area is fairly fixed and does not change or move significantly with head position; thus, proper position depends on comfort and ease of injection. This is in contrast with the midface and jawline, because these units shift depending on head position from vertical to supine.
Procedural Approach
There are several described techniques for injection in this region. The authors prefer subcutaneous injections owing to safety and ease of augmentation. Patients can be graded using the temporal hollowness grading system ( Table 1 ). After delineation of the area to be treated, anesthetic cream is applied and the skin is prepped with an antiseptic solution. The injections are placed in the immediate subcutaneous tissue, between the skin and superficial temporal fascia ( Fig. 2 ). The volume per injection is kept at small aliquots of 0.1 mL or less per injection ( Fig. 3 ). The skin is massaged after each injection.
| Score | Description |
|---|---|
| 4 | Severe: very hollow temples. Significant improvement is expected from injectable implant. |
| 3 | Moderate: moderately hollow temples. Excellent correction is expected from injectable implant. |
| 2 | Mild: shallow hollow temples; minor facial feature. Implant is expected to produce a slight improvement in appearance. |
| 1 | Absent: no hollowness. |


Potential Complications and Their Management
Although the first author has never had any significant complications administering this procedure, there are reports of complications, mostly owing to vascular occlusions as a result of injections in this area. Based on a study at one of the first authors practice, the complications or adverse events were defined as any unfavorable or unintended sign, symptom, reaction, or disease associated in time with the use of an investigational drug or device. Safety was assessed by evaluating all local and systemic adverse events at all visits as well as in the patient diaries. All adverse events documented by the evaluator and through patient diaries were mild or moderate and resolved by the 2-week follow-up ( Table 2 ). One patient noted “hyperpigmentation” in her diary; however, within 2 weeks the mark was completely invisible, and upon questioning the patient, the investigator determined that the adverse event was ecchymosis.
| Adverse Event | n (%) |
|---|---|
| Bruising | 14 (70) |
| Redness | 13 (65) |
| Tenderness | 20 (100) |
| Pain | 16 (80) |
| Swelling | 20 (100) |
| Hyperpigmentation | 1 (5) |
| Skin irregularities | 11 (55) |
| Headache | 15 (75) |
| Chewing | 2 (10) |
| Jaw ache | 1 (5) |
There were 2 instances where a community practitioner contacted one of the authors regarding vascular necrosis in the temporal area. In both cases, the filler was reportedly injected into deep tissues. In both cases, the cardinal signs included transient blanching of the lateral forehead progressing to a reticular pattern, significant pain that was delayed in onset and intensified after several hours of injection, and the appearance of vesicles that were interpreted as an herpetic outbreak. These patients went on to develop necrosis of the superficial dermis with scarring. Both practitioners reported massaging the area once they saw the blanching until the skin turned pink. In the first author’s opinion, once a large bolus of the product is infused intraarterially and massaged, it is forced to move distally into the end arterioles. Depending on the particle size, lodging at the corresponding vessel diameter could explain the immediate transient revascularization, followed by the reticular pattern of blanched and purplish skin.
Postprocedural Care
Immediately after the procedure, the patient was asked to apply light pressure for about 5 minutes and then followed with application of ice packs. All subjects are counseled regarding temporary bumps, bruising, swelling, headaches, and tenderness on mastication.
Rehabilitation and Recovery
All patients are advised to return to their normal daily activities as soon as the injection session is completed. However, patients should be advised to refrain from strenuous exercises for 24 hours to avoid potential swelling and bruising.
Outcomes
In a clinical study, all patients were satisfied with the aesthetic outcome of the procedure. In the first author’s treatment of more than 1000 patients with this technique, the rate of dissatisfaction is extremely low ( Figs. 4 and 5 ).


Midface and malar augmentation
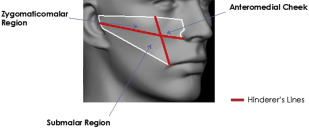
Many surgical approaches have been described in the rejuvenation of the midface. As the use of facial fillers has progressed, more physicians use fillers to rejuvenate the midface by volumization and restructuring of this facial aesthetic area. It is the authors’ belief that the midface is one of the focal points when using facial fillers in aesthetic rejuvenation. In contrast with the temples, where the limits of augmentation are fairly clear owing to its structural boundaries, the midface does not have those clear boundaries. At the Food and Drug Administration’s (FDA) request, the facial subregions that could be used to capture treatment, safety, and effectiveness data were defined. Three midface subregions were defined—the zygomaticomalar region, the anteromedial cheek, and the submalar region. Because all outcomes were similar across facial subregions, this paper focuses on results for overall midface volume deficit. Depending on the placement of the filler, the midface prominence and focal point can change as follows:
- 1.
Lateral zygoma (lateral to a line drawn from lateral cantus to oral commissure), increase width of the midface and shift the focal point laterally
- 2.
Midcheek (medial to a line from lateral cantus to oral commissure, above Hinderer’s line ; anterior projection of the midface, may shift the focal point medially)
- 3.
Submalar (lateral to and a line from lateral cantus to oral commissure and below the Hinderer’s line), shift the focal point.
Treatment Goals and Planned Outcomes
The goal in midface augmentation may range from simply restoring the loss of volume to dramatically changing the shape of the midface through placement of the fillers in noninherent locations. Ample time has to be spent interviewing the patient and evaluating his or her facial structures. In the authors’ experience, most faces are asymmetrical and usually 1 side of the face appears more youthful than the other. Any such findings must be communicated to the patient. Furthermore, the authors believe that the first step in facial filler augmentation is to use the more youthful side as the template while injecting the contralateral side for symmetry. Once close symmetry is reached, then further injections can be made on both sides to further enhance bilateral facial structures.
Preoperative Planning and Preparation
Once the patient and the physician have decided mutually on a desired outcome, facial photographs must be taken at least in 3 views. These views should include the frontal and bilateral oblique. The authors have often evaluated printed photographs to look for details such as variations in the height and width of the zygoma and subtle asymmetries in the malar prominence. Differences in the transition from the midface to the surrounding aesthetic units can also be observed photographically. Furthermore, these photographs can help to communicate to the patient subtle findings that may have been missed when viewed in the mirror ( Fig. 6 ).