37. Correction of the Tear Trough Deformity
Jason K. Potter, Grant Gilliland
■ Soft tissue depressions at the lid-cheek junction represent some of the most challenging, and difficult to correct, age-related deformities of the periorbital region.
■ The term “tear trough deformity” was first coined by Flowers and refers to the development of visible depression along the medial third of the lower lid.1
■ Contemporary use of the term tear trough deformity refers to a variable spectrum of soft tissue deformities across the lid-cheek junction that are a direct result of the interplay of complex, age-related changes that occur in the lower lid and midcheek.
• Correction of these deformities may therefore include procedures directed at rejuvenating both the lower lid and midcheek areas depending on their severity.
TERMINOLOGY2
■ Nasojugal groove: Natural sulcus directly overlying the medial one third of the inferior orbital rim.
• “Tear trough deformity” refers to a prominent nasojugal groove.
■ Palpebromalar groove: Prominent depression at lid-cheek junction inferolateral to nasojugal groove.
• It is confluent with nasojugal groove.
■ Midcheek: Region of cheek medial to a line extending from the frontal process of the zygoma to the oral commissure and from the lower lid to the nasolabial fold.
• Prezygomatic part: Overlies the skeleton of the midcheek.
• Infrazygomatic part: Covers the vestibule of the oral cavity.
■ Tear trough triad: Association of several anatomic characteristics giving rise to a prominent tear trough (Fig. 37-1).
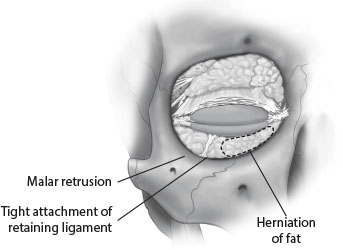
Fig. 37-1 Tear trough triad.
• Herniation of orbital fat
• Tight attachment of the orbicularis retaining ligament along the arcus marginalis
• Malar retrusion
GRADING SYSTEM (Table 37-1)
Table 37-1 Grading System for Tear Trough Deformity
| Deformity | Grade |
| No medial or lateral lines indicating the arcus marginalis or the orbital rim Contour is smooth and youthful; no transition at the orbit-cheek junction | 0 |
| Medial line or shadow is mild or subtle Lid-cheek junction has a smooth lateral transition | I |
| Lid-cheek junction shows a moderate prominence, extending from medial to lateral | II |
| Orbit-cheek junction shows a severe prominence, with an obvious step between orbit and cheek | III |
■ An objective system for grading the severity of deformity has been proposed by Barton et al.3
• More severe deformities are characterized by changes not limited to the nasojugal groove.
CLASSIFICATION OF MIDFACE MORPHOLOGY (Fig. 37-2)
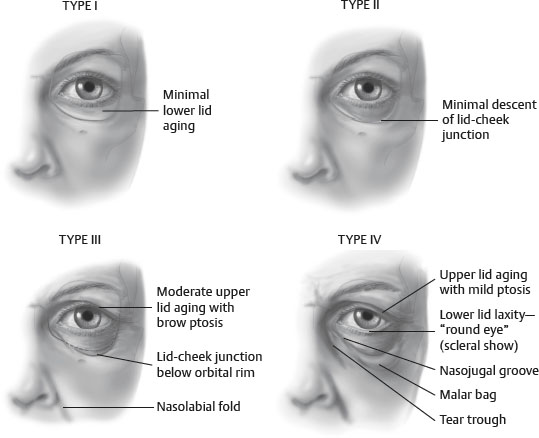
Fig. 37-2 Classification of midfacial morphology involving lid and cheek.
■ Classification system incorporating the global changes occurring at the eyelid-cheek junction and midface.4
ANATOMIC CONSIDERATIONS CONTRIBUTING TO DEFORMITIES AT THE LID-CHEEK JUNCTION5–7
Periorbital and midcheek anatomy has been reviewed in detail in Chapter 22.
MEDIAL FAT PAD
■ Bulge extends anteriorly in a position superior to the inferiomedial orbital rim.
• Visually, this creates an apparent increase in the depth of the nasojugal groove.
■ Inferior descent is limited by the tight, direct attachment of the orbicularis to the medial orbital rim.
SENIOR AUTHOR TIP: The medial fat pad can be quite vascular and care must be taken in the dissection of this fat pad to prevent vascular injury that retracts into the orbit, which can result in a retrobulbar hematoma.
CENTRAL FAT PAD
■ Inferior descent over the central orbital rim is not restricted and therefore occurs progressively.
■ Inferior descent distends the orbicularis retaining ligament (ORL) inferiorly several millimeters.
■ Inferior descent and distention of the ORL creates an apparent increase in the depth as well as the length of the nasojugal groove.
■ With increasing magnitude of descent, a sulcus develops lateral and inferior to the central fat bulge—the palpebromalar groove.
• Palpebromalar groove creates a visible demarcation of the lid-cheek junction laterally.
SENIOR AUTHOR TIP: The medial and lateral fat pads are separated by the “arcuate expanse.” This is a fibrous extension from the arcus marginalis inferolaterally extending medially to the medial canthal tendon. It is a retroseptal structure which functions to prevent overaction of the inferior oblique muscle.
FESTOONS
■ Can be multifactorial
■ Skin and skin/muscle festoons can be addressed by redraping the skin and/or skin/muscle in a more anatomic position.
■ Dermal festoons are more difficult to treat and are related to the interdigitation of the orbitomalar retaining ligament with the subdermal collagen as the direction of the collagen fibers change from circumocular in the eyelid to more vertical in the cheek.
SENIOR AUTHOR TIP: It is very important to identify festoons and their etiology prior to surgery so that they can be addressed and patient expectations for swelling in this area can be properly addressed.
INDICATIONS AND CONTRAINDICATIONS
■ Main indication is the presence of enough deformity so that surgery may make a difference.8
■ Patients who would clearly benefit from surgery are those with orbital fat herniation and significant skin laxity.4
• Patients who have these characteristics should be discouraged from injectables alone, as they are highly likely to have an undesirable result.
■ Nonsurgical management with injectables is a good option for mild to moderate tear trough deformities, but patient selection is paramount.9
NONSURGICAL AND SURGICAL TREATMENT OPTIONS
PREOPERATIVE EVALUATION FOR NONSURGICAL AND SURGICAL TREATMENT
■ Consideration of perorbital form and function, along with anatomy and patient expectation, must be balanced with protecting lid function.10
■ Evaluation of the lower eyelid should include:
• The distance from the pupil to the lower eyelid margin (MRD-2)
• The distance from the pupil to the tear trough
• The width of the tear trough
• The intercanthal angle
■ These quantitative measurements can allow for objective preoperative and postoperative assessment and allow for more predictable results.11
SENIOR AUTHOR TIP: Assessment of lower eyelid laxity via the snap test is important in assessing whether lower eyelid tightening, and/or shortening, should be performed at the time of blepharoplasty surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




