The cleft nasal deformity remains the most likely stigma of the cleft to remain plainly visible despite vigorous and repeated attempts at correction. This deformity is present at birth, but evolves over time. Certain aspects can be treated early, but some, such as the dorsal and septal deformity continue to develop as facial growth proceeds through adolescence. This article presents a conceptual mechanism and a philosophy of conservative reliable gains starting at the primary operation, with the long-term view of achieving definitive correction at maturity. Cogent planning of longitudinal care of the deformity from infancy leads to solid, predictable results.
Key points
- •
The cleft nasal deformity remains the most likely stigma of the cleft to remain plainly visible despite vigorous and repeated attempts at correction.
- •
History has witnessed a swinging pendulum in the care of this deformity, starting with ignorance and succeeded by aggressive, numerous, and radical operations.
- •
Today multiple schools of thought exist, but most recognize that an aggressive early operation does not necessarily negate the need for future operations.
- •
The cleft nasal deformity is present at birth, but evolves over time. Certain aspects can be treated early, but some, such as the dorsal and septal deformity continue to develop as facial growth proceeds through adolescence.
- •
This article presents the authors’ concept of the mechanism and philosophy of conservative reliable gains starting at the primary operation, with the long-term view of achieving a definitive correction at maturity.
- •
The diligent student of the cleft nasal deformity who cogently plans the longitudinal care of the deformity from infancy will be rewarded with solid, predictable results.
Overview
Those who routinely perform cleft rhinoplasty, in addition to cosmetic or functional rhinoplasty in the noncleft patient, readily acknowledge that cleft septorhinoplasty is the single most challenging rhinoplasty to perform. The reasons for this are emphasized in this article, but derive from the complexity of the structural deformity with attendant misconceptions, multiple sites of potential functional obstruction, and the effects of prior surgery. For this reason, those who perform cleft rhinoplasty must not only be highly skilled rhinoplasty surgeons but must also have a strong background of understanding cleft pathoanatomy.
Overview
Those who routinely perform cleft rhinoplasty, in addition to cosmetic or functional rhinoplasty in the noncleft patient, readily acknowledge that cleft septorhinoplasty is the single most challenging rhinoplasty to perform. The reasons for this are emphasized in this article, but derive from the complexity of the structural deformity with attendant misconceptions, multiple sites of potential functional obstruction, and the effects of prior surgery. For this reason, those who perform cleft rhinoplasty must not only be highly skilled rhinoplasty surgeons but must also have a strong background of understanding cleft pathoanatomy.
Historical perspective
Desmond Kernahan’s observation in 1980 that “a repaired cleft is revealed more by the associated nasal deformity than by the lip repair” continues to be true today, underscoring the historical difficulty with this complex and dynamic problem. Peter Randall put it this way: “I am reluctant to say correct the cleft lip nose deformity, because, in my experience, it is impossible to really correct the severe deformity.”
The early twentieth century saw numerous approaches often characterized by radical external incisions. A review of the myriad of approaches cataloged in Millard’s Cleft Craft demonstrates designs in many ways at odds with the standard of care in aesthetic rhinoplasty at the time. These conflicting approaches were a direct result of similarly conflicting ideas about the underlying mechanism of the deformity.
Then in 1955, counter to patterns prevalent at the time, Gustave Aufricht wrote a treatise on cleft rhinoplasty, urging surgeons to avoid nonanatomic or overly aggressive techniques, in response to the clinical observation that patients treated with these radical techniques were being left with iatrogenic deformities that were nearly impossible to correct. He emphasized the importance of treating all rhinoplasty patients with consistent standards regardless of the presence of a cleft.
However, a more positive sentiment voiced by Gillies and Kilner has become increasingly apt since that time:
optimism… is justified, for the structural defects underlying the deformity are gradually being made more clear and accurate diagnosis is becoming possible. Cure seldom anticipates diagnosis, but it is usually quick to follow it.
In 1984, Harold McComb from New Zealand addressed the question as to whether the nasal deformity was due to intrinsic abnormalities including hypoplasia or malformation versus extrinsic abnormalities including deformation or malpositioning of otherwise normal structures. By performing cadaveric dissections of unoperated clefts in infants, he demonstrated that the cleft-side lower lateral cartilages were actually of normal size and shape, though displaced and tethered posterolaterally, and that symmetric nares could be achieved with release and repositioning.
The tilted tripod model of Hogan was an influential contribution that emphasized the importance of the skeletal base in determining the changes in the cartilages and septum. It is noteworthy that significant inaccuracies were present in both of these models, demonstrating common misconceptions in the field. Contributions since that time, including those of Fisher and Mann, have substantially added to the present-day concept of the deformity and its underlying mechanism. Nowadays a wide philosophic spectrum remains regarding the timing and design of operations.
Salyer and colleagues aim at primary correction of the unilateral primary deformity. Their technique involves dissection of the lower lateral cartilage extending onto the normal side through the medial aspect of the incision below the inferior turbinate. The cartilage remains attached to the skin at the dome near the genu, but is otherwise completely freed for repositioning.
Cutting also performs a primary operation designed to allow correction of deformity. The lower lateral cartilages are dissected free at the footplates and ascending medial crura to allow differential positioning of the cartilages. Dissection proceeds to the tip, cleft-side ala, and noncleft upper lateral cartilage to facilitate a Tajima suspension suture. Complete mobilization of the lower lateral cartilages relative to one another and to the piriform enables repositioning in a corrected position. In the bilateral cleft, a retrograde dissection preserving blood supply allows access to cartilages for dissection in the cases of patients treated with nasoalveolar molding.
Guyuron’s approach to the secondary unilateral cleft nasal deformity emphasizes the use of standard aesthetic rhinoplasty techniques. Additional techniques designed to deal with specific cleft-related findings are also commonly used. Wedge osteotomy of the bony dorsum may be required to facilitate medial repositioning of the wide and flattened bones. The septoplasty includes resection of vomer and perpendicular plate of ethmoid in addition to quadrangular cartilage resulting from the cleft septal deformity. Direct excision of soft triangle is also noted to be a necessary means of achieving a more elongated, vertically oriented nostril.
The approach of Burget is similar, and he describes significant limitations to primary cleft rhinoplasty attributable to the insubstantial quality of the nascent cartilages of infancy.
The cleft lip nasal deformity
An understanding of the underlying mechanisms responsible for the cleft lip nasal deformity (CLND) is critical if the surgeon wishes to ever reverse the deformity. Although it is often stated that every cleft is different, any individual cleft nasal deformity occurs along a spectrum of potential deformities. It is helpful to look at a series of photographs of patients, from mild through severe. Imagine making a flip-card movie of these photographs. The alterations in the morphology can then be visualized. It is a reversal of this deformation of morphology that must be borne in mind at every step of care.
In 1998, Fisher and Mann presented a model to describe the mechanisms responsible for the cleft lip nasal deformities, mild through severe, unilateral and bilateral. More recently, Fisher and Sommerlad developed a computer-generated animated video of this model. The model is anatomically based. The lobule of the nose is reduced to 2 pairs of arches ( Fig. 1 ). The paired cutaneous arches are formed by the nostril margins, each being based medially at the columellar base and laterally at the alar base. The paired cartilaginous arches are formed by the lower lateral cartilages, the accessory cartilages, and their investing perichondrium. Each cartilaginous arch is based anteriorly at the premaxilla and posteriorly at the piriform margin at the axial level of the inferior turbinate. The four arches are coincident in the columella. The cartilaginous arches diverge from each other as the medial crura form the middle crura and then the domes. On each side the cutaneous arch diverges from the cartilaginous arch at the soft triangle. Soft-tissue attachments between arches ensure that no single arch is able to move independently of the other arches.
Within the spectrum of the cleft deformity, typical skeletal alterations are observed to varying degrees. Even in the most minor form of cleft there is hypoplasia of the cleft-side piriform margin ( Fig. 2 ). Muscular diastasis produces separation of the cleft-side columellar base and alar base. With greater degrees of clefting, anterolateral rotation of the greater segment accompanies progressive hypoplasia of the piriform rim and skeletal alar base. In the symmetric bilateral case, the premaxilla rotates anteriorly.
As these skeletal asymmetries progress, one observes progressive and predictable changes of arch position and, thus, nasal morphology.
In the unilateral case, separation of the columellar base and alar base is observed. As the greater segment rotates anterolaterally to the noncleft side, the columellar base and caudal septum deviate away from the cleft side. With progressive anterolateral rotation of the greater segment and hypoplasia of the piriform rim, there is increasing deformity of the cleft-side cartilaginous arch that spans these separating bony parts. The footplate deviates away from the midline to the noncleft side, and the lateral crus is pulled posterolaterally. The true dome point migrates posterolaterally as a new genu forms progressively more medially. As a result, one observes shortening of the medial crus and, therefore, of the columella on the cleft side. Posterolateral traction of the lateral cartilaginous arch is transmitted through soft-tissue attachments to the cutaneous arch, and the recurvatum deformity and lateral alar flare can now be observed. The normal overlap of the caudal margin of the upper lateral cartilage by the cranial margin of the lower lateral cartilage is lost. The tension of the cartilaginous arch raises a bowstring elevation of the vestibular lining, the so-called vestibular web.
In a symmetric bilateral cleft, the premaxilla rotates anteriorly and the septum remains midline. Piriform margin hypoplasia and the effects on the lower lateral cartilages occur bilaterally. Bilaterally, the columella is short. The retrodisplaced domes are separated. The vestibular web, recurvatum deformity, and alar flare occur bilaterally.
Because the cleft nasal deformity is the result of an underlying skeletal deformity, this skeletal deformity needs to be corrected before any correction can be fully realized in the nose. Because presurgical orthopedics can only partially improve the deformity (maxillary segment malalignment but not hypoplasia) and because most surgeons do not perform primary bone grafting, it is unrealistic to completely correct the nasal deformity at the primary operation. A plea must be made for patience. There will be future opportunities to augment the skeletal base deficiencies at the time of alveolar bone grafting and orthognathic surgery if indicated; this will set the stage for definitive septorhinoplasty. At this time deformities such as a broad deviated nasal dorsum, which are only obvious after maturity, may be addressed. Definitive secondary septorhinoplasty will be successful only if the cartilages are intact and robust, and if the skin envelope is complete and free of scar.
Surgical technique
Primary Cleft Lip and Nasal Repair
Primary cheiloplasty and rhinoplasty can be performed whether or not presurgical orthopedics has occurred. If presurgical orthopedics has corrected the anterolateral rotation of the greater maxillary segment, the required movements will be less, and in all likelihood the degree of recurrence of the deformity will be reduced.
Each surgeon will have his or her own methods and timing for correction of the deformation of the components of the nose already described. Whatever the plan, all interventions should be performed with a reversal of the deformity in mind while avoiding uncorrectable iatrogenic deformities. The author’s (D.M. Fisher) plan involves a series of interventions, each improving the deformity to some extent while setting the stage for a definitive septorhinoplasty in the later teens. Presurgical infant orthopedics should narrow the cleft and bring the premaxilla to the midline ( Fig. 3 ). Primary rhinoplasty is performed with the following goals in mind:
- 1.
Balanced alar bases (from the anterior view)
- 2.
Columellar base mobilization to the midline
- 3.
Caudal septal release and repositioning
- 4.
Alar base release and repositioning
- 5.
Lateral piriform release and repositioning
- 6.
Anteromedial advancement of the cleft-side dome and lateral crus
- 7.
Creation of the scroll
- 8.
Lateralization of the cleft-side lateral vestibular lining
- 9.
Support
- 10.
No external skin incisions
- 11.
No excision(s) of skin envelope
The authors prefer the anatomic subunit approximation technique for primary lip repair ( Fig. 4 ). This technique, like the inferior triangle repair and the straight-line repairs, introduces the least scar at the base of the nose. Balancing of the alar bases should be a primary goal at the time of presurgical marking. The relative positions of the lateral and medial points of closure in the nostril sill should be planned so as to achieve nares of equal circumference and alar base symmetry from the anterior view.
Lip repair begins with incisions in the medial lip element. The cephalic insertion of the orbicularis oris muscle is divided. Dissection to the muscle deep to the columellar base will allow for mobilization of the columella to the midline and access to the anterior nasal spine. The septospinal ligament is divided, allowing for access to the caudal septum. The caudal septum is freed from the premaxilla, and a dissection plane is made between the septum and the noncleft-side mucoperichondrium. The caudal septum can now be easily mobilized to the vertical plane. Maintaining attachments of the cleft-side mucoperichondrium will allow the septum to be drawn toward the cleft side with the closure of the nostril sill.
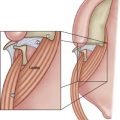
Attention is then directed to the lateral lip element. The lip incisions are made. The cephalic insertion of the orbicularis oris muscle is divided, and continuation of dissection deep to the muscle will allow for mobilization of the alar base ( Fig. 5 ). The alar base can now be mobilized anteromedially; however, this will accentuate the recurvatum deformity and the lateral alar flare because the cartilaginous arch remains attached to the piriform margin. Release of the lower lateral cartilage–accessory cartilage complex from the piriform rim relieves the tension of the cartilaginous arch on the nostril margin, and will allow the cleft-side nostril margin to become round when the alar base is advanced anteriorly and medially ( Fig. 6 ). This lateral piriform release needs to extend to an axial level above the inferior turbinate. It can be performed submucosally in incomplete cases, but with near complete and complete clefts there is also some element of deficiency of vestibular lining, and it is helpful in these cases to divide the mucosa along the piriform rim.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree