CHAPTER 29 Conventional upper and lower blepharoplasty
History
An ever-improving understanding of the dynamic nature of facial anatomy accompanied with a more holistic approach to facial aging has altered the surgical treatment of age-related periorbital changes. Conceptually, trends point towards decreasing tissue removal in favor of tissue rearrangement and repositioning. Standard blepharoplastic incisions now allow for effective treatment of all of the aforementioned age-related changes. Increasingly limited upper eyelid fat excision and minimal lower lid orbicularis occuli violation has helped avoid exacerbation of orbital hollowing and minimized ectropion, respectively. Moreover, precise soft tissue augmentation (autologous and non-autologous) of the upper lid can help recreate a more youthful appearance.1 Similarly, these techniques can be quite useful in blunting the tear trough deformity. Complementing these trends is the use of botulinum toxin (Botox, Allergan) to help decrease rhytids that characterize aging.
Physical examination
Eye exam
A detailed medical and ophthalmologic history and a standard eye exam including visual acuity in each eye is required. Dry eyes, which can be exacerbated by blepharoplasty, are best identified through careful history taking and Schirmer’s testing (less than 10 millimeters of moisture on a piece of filter paper in the conjunctival sac after five minutes is considered abnormal).2 Evaluation includes the assessment of a Bell’s phenomenon which can be protective, particularly if an ectropion develops. Agents which promote bleeding and inhibit clotting must be eliminated and adequate time for reversal of their effects must elapse prior to surgery. Perioperative blood pressure control is vital and should be managed pharmacologically if indicated. A low threshold for ophthalmologic consultation in the event of positive findings on history and physical is advocated.
Excess skin
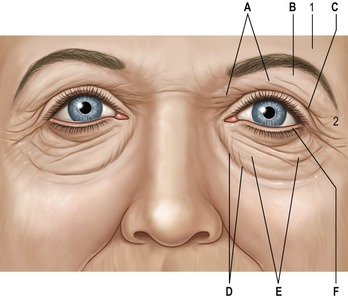
See Fig. 29.1. A common presenting complaint of patients, excess eyelid skin, or dermatochalasis, should be noted on physical evaluation and precisely assessed especially regarding extent and location. Occasionally, the upper eyelid skin redundancy is excessive enough to impact the visual axis and/or result in pseutoptosis. Asymmetry, the correction of which is a central goal of blepharoplasty, must be also identified. Excess skin resulting from blepharochalasis may, ultimately, be treated similarly to age-related skin excess but the risk of ptosis and other disease-specific conditions require recognition of this entity. Lower lid skin excess is less common than lower lid wrinkling which invites a more conservative surgical approach particularly in light of the possibility of ectropion. Pre-tarsal skin fullness is more often due to the underlying orbicularis occuli than to skin excess.
Fat pseudoherniation
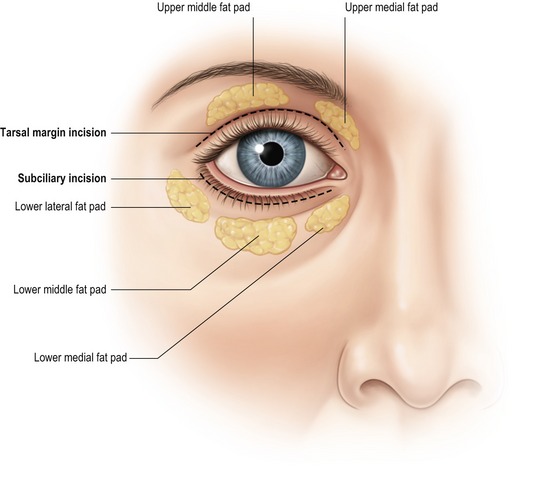
Frequently found in conjunction with skin excess, orbital fat pseudoherniation contributes significantly to the “tired look” of age-related periorbital changes (Fig. 29.2). The size and shape of the medial and middle fat pads of the upper lid and the three lower lid fat pads should be noted. Upward and downward gaze in an upright patient will accentuate the fat pads. The configuration of the lower lateral fat pads, should be documented, since they are easily underappreciated, particularly in the sedated, supine patient.
Negative vector
The position of the cornea anterior to the infraorbital rim entails an increased potential for untoward sequelae after lower lid surgery including lid retraction and ectropion.3