Fig. 16.1
Stab wound to the left back without intraperitoneal or retroperitoneal penetration

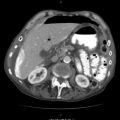
Fig. 16.2
Gunshot wound to back with evidence of intraperitoneal penetration. Patient found to have multiple enterotomies at laparotomy
While firearm injuries tend to leave a more obvious wound tract, stab wounds with their lower energy are more problematic. Given the challenge in fully delineating the exact trajectory of the wound tract, the technique of CT tractography has been developed. Simply put – prior to the imaging – the wound tracts are packed with gauze soaked in a radiopaque solution. The allowed for more accurate determination of intraperitoneal or retroperitoneal penetration, while virtually excluding penetration or significant injury in the majority of patients. While this technique is certainly not universally accepted and employed, it might prove useful in certain circumstances.
It should be noted, however, that the same potential issue regarding high-energy firearms exists in penetrating gunshot wounds to the back and flank. A clinician should have a high index of suspicion for occult injury with bowel wall contusion and potential late presentation of injury in cases where the firearm used is of an especially high energy, such as a military or large game rifle. In these cases, significant injury can occur even with the absence of direct bowel penetration and with tangential missile paths. With these injuries, it is reasonable that, at the very minimum, the patient be observed for up to 24 h and further investigation be undertaken as dictated by the patient’s clinical status.
16.3 Thorax
Penetrating injuries to the thorax represent a critical diagnostic dilemma. While certain presentations such as massive hemothorax or ongoing bleeding mandate rapid operative exploration, the large majority of injuries can be managed by simple tube thoracotomy or observation alone. In fact, only approximately 15 % of patients with penetrating chest trauma require any type of therapeutic operative procedure. However, given the potential for serious morbidity and mortality associated with injury to the heart, great vessels, or aerodigestive tract structures, rapid accurate diagnosis is essential (Figs. 16.3 and 16.4).



Fig. 16.3
Saw injury to the right anterior chest wall without evidence of intrathoracic penetration. Complicated wound care due to extensive tissue defect

Fig. 16.4
Stab wound to the right chest with intrathoracic penetration and lung injury. No evidence of mediastinal or intrathoracic vascular injury. Successfully treated with thoracotomy tube drainage
The use of chest CT and CT angiography as a tool for triage of stable patients with penetrating chest trauma has been well described in the literature. When combined with echocardiography, chest CT has been demonstrated as able to exclude injury in approximately 80 % of patients. For those patients who have CT findings concerning for significant injury, additional diagnostic procedures such as bronchoscopy or esophagostomy are useful to further evaluate the areas of concern. Chest CT and CT angiography have been shown to be a useful screening tool for patients with transmediastinal gunshot wounds. It can be used with good accuracy to evaluate for hemopericardium suggestive of penetrating cardiac injury, especially when echocardiography is not immediately available. High-resolution CT angiography is especially helpful in assessing for subclavian and axillary artery injury and has virtually supplanted conventional angiography at the initial mechanism to screen for thoracic vascular injury. In addition, it has been demonstrated that chest CT was far better than conventional chest radiography at predicting the presence of significant undrained hemothorax needing surgical evacuation. Furthermore, in patients who have injuries identified which require operative intervention, chest CT has been shown to accurately locate the injury and in some cases provides information leading to a change in the operative approach best suited for the injuries identified (Fig. 16.5).
Fig. 16.5
(a) Stab wound to the left chest with evidence of diaphragm injury adjacent to wound tract. (b) Coronal reconstruction of diaphragm injury showing herniation of abdominal fat through defect
One area where newer generation CT scans have become useful is the detection of diaphragm injuries. New multidetector CT scanners can now resolve the presence of diaphragm injuries with a sensitivity and specificity of 82–94 % and 88–95.9 % with an overall accuracy of almost 96 % and negative predictive value of 93 %. While this represents a significant improvement from the older technology scanners, a high index of suspicion remains important as significant injuries can still be missed by imaging alone.
An additional area where chest CT has been reported as extremely useful is in the initial screening of patients with minor penetrating chest trauma. In a recent study comparing the use of serial conventional chest radiographs with CT imaging, it was found that CT scan more accurately depicted the injuries present. In addition, in stable patients, a normal chest CT was shown to obviate the need for admission and follow-up chest imaging, leading to a potential cost savings, decreasing the proportion of patients signing out prior to the completion of their workup and allowing for expedited discharge directly from the emergency department.
All said, chest CT and CT angiography provide a rapid means of triage and diagnosis of injuries in stable patients with penetrating chest trauma. When used as a screening tool to allow for rapid discharge of patients without significant injury and to identify those patients either with definitive evidence of injury or for whom further workup is needed, it can provide a wealth of information. While some suggest that it is overutilized, it has the ability to rapidly detect life-threatening injuries and provides the information needed for optimal treatment. Conversely, it also provides a means to facilitate rapid discharge of patients without significant injury, freeing scarce resources for the treatment of patients more in need.
16.4 Head and Neck
In the evaluation of penetrating injuries to the neck, the availability of high-resolution CT scan and CT angiography has had a dramatic impact on the need for surgical neck exploration. In the past, penetrating injures to the neck with violation of the platysma, especially those in zone II (the cricoid cartilage to the angle of the mandible), were thought to mandate surgical exploration. This resulted, however, in a high rate of negative explorations leading many to suggest the need for more selective exploration based on diagnostic evaluation using modalities such as bronchoscopy and esophagostomy.
With the advent of newer generation CT scan technology in the late 1990s, several institutions began to question the need for invasive diagnostic procedures in the workup of stable patients with penetrating neck trauma. In two small series done by urban US level 1 trauma centers, CT scan was evaluated for its usefulness in the diagnosis of significant vascular or aerodigestive tract injuries. Mazolewski et al. evaluated CT scan results with operative findings and determined that CT had a high sensitivity and specificity (100 % and 91 %, respectively) for the detection of significant injuries in penetrating zone II neck trauma. Another study by Gracias et al. used CT scan as the sole initial diagnostic study in stable patients. They found that CT scan effectively ruled out injuries in 56 % based on a wound trajectory remote from vital structures. Based on a 3–6-month follow-up, there were no missed injuries. This early enthusiasm was not universal. Another center reported that CT scan had only a 50 % sensitivity in detecting aerodigestive tract injury from penetrating neck trauma and contributed only minimally to the results of physical exam (Figs. 16.6 and 16.7).
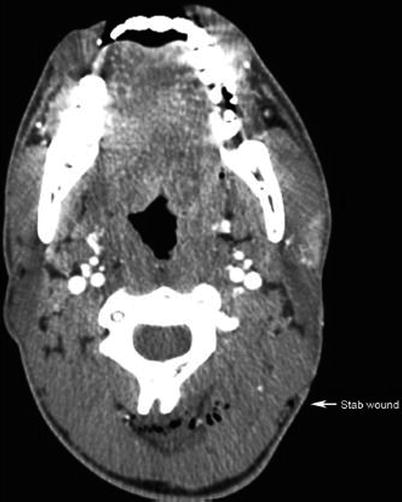

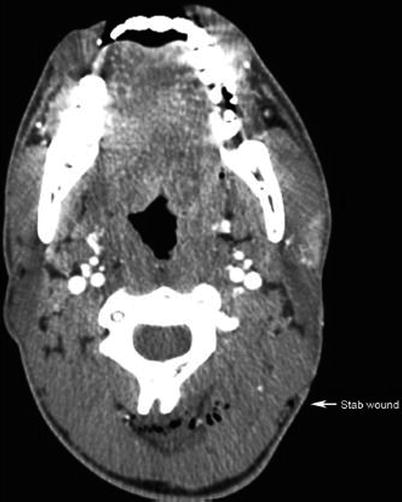
Fig. 16.6
Stab wound to the left posterior neck clearly showing wound tract without evidence of proximity to vascular structures

Fig. 16.7
Slash wound to the left neck which clearly penetrated platysma on exam. CTA neck demonstrating no evidence of proximity or injury to vascular or aerodigestive tract structures. Treated with wound washout and closure without formal neck exploration
Several large series have been reported looking specifically at the use of CT angiography to evaluate for vascular injury in penetrating neck trauma. In a patient without hard signs of vascular injury, it is reported the physical exam alone in the region has an especially poor sensitivity and specificity (57% and 53 %) for the detection of occult vascular injury. In specifically evaluating CT angiography, Munera et al. compared the results of CT angiography with conventional angiograms. They clearly demonstrated a good correlation with conventional angiography as well as a high sensitivity and specificity (90% and 100 %) for the detection of vascular injuries diagnosed by (Fig. 16.8).
Fig. 16.8
(a) Stab wound to the right neck with evidence of internal carotid artery (ICA) injury. Patient with large middle cerebral artery (MCA) territory thrombotic stroke successfully treated with neurointerventional extraction of thrombus and coiling of the right proximal and distal ICA with excellent functional recovery. (b) CTA reconstruction of the right ICA injury demonstrating abrupt cutoff of the right ICA without distal reconstitution
Another study prospectively examined the usefulness of CT angiography as the initial screening mechanism in stable patients with neck injuries penetrating the platysma. Inaba et al. demonstrated a sensitivity of 100 % and specificity of 93.5 % for the detection of vascular and aerodigestive tract injuries. The use of CT angiography has been shown to decrease the rate of formal surgical neck exploration, as well as the rate of negative neck exploration when used in stable patients not requiring emergent exploration.
In 2008, the Eastern Association for the Surgery of Trauma issued a practice management guideline regarding penetrating zone II neck trauma. After an exhaustive review of the relevant literature, it was concluded that selective operative management of penetrating zone II neck injuries is recommended to minimize unnecessary operations. High-resolution CT angiography was identified as the initial diagnostic study of choice when available.
Based on the quality of the images generated by the newest generation of CT scanners – some authors are going as far as suggesting that the classic delineation of penetrating neck trauma by anatomic zone be abandoned. In a patient without hard signs of injury or hemodynamic instability, it is suggested that CT angiography be used at the first imaging modality. It allows for rapid determination of injury trajectory and provides an excellent assessment tool for the diagnosis of both aerodigestive track and vascular injuries. With the early use of high-resolution CT angiography the workup can be simplified and use of pan endoscopy, oral contrast studies and surgical neck exploration can be limited to the subset of patients in which it is likely to be higher yield. While some advocate the limited use of imaging in the case of no significant physical exam findings, they do suggest that it be used liberally when soft signs are present.
Again, it should be obvious that patients with signs of obvious life-threatening injury including massive hemorrhage, expanding hematoma, or airway compromise require emergent surgical exploration. However, in the stable patient with a penetrating neck injury, CT and CT angiography represent excellent tools for the diagnosis of both aerodigestive tract and vascular injuries. Their liberal use, followed by the appropriate use of other diagnostic modalities and selective surgical exploration, is associated with timely intervention for injures, with the prevention of a large number of negative surgical explorations.
16.5 Extremities
When dealing with penetrating extremity trauma, the use of CT and CT angiography can enhance the clinical picture in the appropriately selected patient. Certainly in a patient with hard signs of vascular injury (including pulsatile bleeding, expanding hematoma, pulselessness, thrill/bruit) and active hemorrhage or limb-threatening ischemia, the primary intervention should be operative, with the use of on-table angiography as dictated by the operative findings. However, in the stable patient with soft signs of vascular injury including decreased pulses or Ankle Brachial Index (ABI), non-expanding hematoma, history of significant bleeding, or concerning proximity of the wound tract to major vascular structures, CT angiography can be of benefit both in confirming the injury and determining the character and location of the injury and potential appropriateness of nonoperative and less invasive interventions such as stenting or angioembolization (Fig. 16.9).
Fig. 16.9
(a) Gunshot wound to the left lower extremity. No evidence of significant bony or vascular injury. Treated with local wound care. (b) CTA reconstruction of lower extremity vasculature demonstrating no evidence of vascular injury
In the radiographic evaluation of extremities for vascular injuries, conventional angiography has long been considered the gold standard. However, over the past several years with the development of multidetector CT scanners, CT angiography has been shown by several authors to offer both a high sensitivity (95–100 %) and specificity (87–100 %) for the detection of injuries, without the potential drawbacks of conventional angiography such as access site thrombosis, groin hematoma, distal plaque embolization, or intimal dissection. When the use of CT angiography was retrospectively evaluated at an urban US level 1 trauma center, Peng et al. found that its use effectively ruled out injuries in 55 % of studies and was associated with zero false negatives or missed injuries as well as excellent correlation between CT angiography results and operative findings in patients who had injuries identified and subsequently underwent operative exploration. Furthermore, the authors noted that by the end of their study period, CT angiography had become the radiographic study of choice in the initial evaluation of extremity vascular trauma at their institution. Another review of the technique by Soto et al. at a Columbian trauma center demonstrated excellent sensitivity and specificity (95 % and 98 %, respectively) with one false-positive result over 139 patients. The authors did point out that almost 4 % of the studies performed were so degraded by scatter artifact from retained metal fragments that they were non-interpretable. Injuries were effectively ruled out by 55 % of the interpretable studies (Fig. 16.10).
Fig. 16.10
(a) Gunshot wound to the left lower extremity with evidence of contrast extravasation in the territory of superficial femoral artery (SFA). Patient required vascular repair using vein graft. (b) Vascular reconstruction demonstrating SFA injury with extravasation as well as distal reconstitution of vessel
CT angiography represents a step forward in the workup of stable patients with extremity injures concerning for vascular injury without hard signs. While it only allows for diagnosis, it does so without many of the potential hazards associated with conventional angiography. With its high sensitivity and specificity and low potential for complications compared to conventional angiography, CT angiography offers an excellent radiographic tool for the rapid diagnosis of peripheral vascular injuries. Once the presence of CT angiographic signs of arterial injury, including active extravasation, pseudoaneurysm formation, abrupt narrowing of a vessel, loss or opacification of an arterial segment, or arteriovenous fistula, has been confirmed, either operative intervention, interventional radiographic intervention, or appropriate observation can be undertaken as dictated by the injury. It is important to note that the ability to detect injury is potentially related to the resolving power of the scanner. One author notes that the lack of intimal injuries detected over a 3-year period at their institution may have been related to the limited resolution of the four-row multidetector CT scanner used at the time.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree