This article reviews published data on the effects of surgery and compression in the treatment of venous ulcers and the best options for compression therapy. Randomized controlled studies reveal that surgery and compression have similar effectiveness in healing ulcers but surgery is more effective in preventing recurrence. Most leg ulcers have a venous pathophysiology and occur because of venous ambulatory hypertension caused by venous reflux and impairment of the venous pumping function. Proposed surgical interventions range from crossectomy and stripping to perforator vein interruption and endovascular procedures (laser, radiofrequency). More conservative procedures (foam sclerotherapy, conservative hemodynamic treatment) have also been proposed.
- •
Randomized controlled studies comparing surgery and compression point out that surgery and compression have similar effectiveness in producing ulcer healing but surgery is more effective in preventing recurrence.
- •
There is evidence that compression is better than no compression, compression with strong pressure is better than compression with mild to moderate pressure, and compression exerted by multi-component devices is better than compression by mono-component devices.
- •
Elastic stockings exerting the highest pressure that can be tolerated by the patient must be used after ulcer healing to prevent recurrence.
Introduction
In more than 70% of patients, leg ulcers are caused by venous diseases, such as superficial or deep venous insufficiency and deep vein obstruction ( Fig. 1 ). Venous reflux and reduced venous pumping function result in ambulatory venous hypertension (AVH).

The hydrostatic venous pressure in the lower leg in the standing position is about 70 to 80 mm Hg both in healthy individuals and in patients with venous disease, because it depends on the pressure exerted by the column of blood from the right heart to the ankle.
In the normal individual this pressure decreases significantly during active movement (eg, walking) because of venous pumping and the valvular function that fragments the blood column and reduces hydrostatic venous pressure. In patients with venous insufficiency or obstruction, pressure decreases much less or may even increase because of reduced pumping function and valvular incompetence, and this condition is termed AVH.
The pathophysiological mechanisms leading from venous hypertension to skin changes and ulcer formation are still unclear and could be caused by varied mechanisms. Fibrin cuff formation around the microvessels, impaired exchange of gases (O 2 , CO 2 ), the entrapment of white cells in the microvessels causing skin necrosis, and the inhibition of growth factors causing stagnation of the healing process are responsible for skin breakdown and delayed healing.
In the treatment of venous ulcers, the main aim is to counteract AVH, the most important cause of the skin damage. This is done by compression therapy, by elevating the leg, by walking, by the abolition of reflux by means of surgery (including ablation of superficial incompetent veins or perforator veins, catheter dilatation, and stenting or valve reconstruction of deep veins), or by more conservative methods, (endovascular procedures, such as laser therapy, radiofrequency ablation, foam sclerotherapy, or hemodynamic correction of venous insufficiency).
Compression therapy is able to narrow or occlude the leg veins by applying appropriate external pressure to induce a valvular mechanism that reduces venous reflux and increases the calf pumping function.
The appropriate timing for compression and venous surgery and the choice of the compression most useful for the healing of ulcers, remain unclear ( Box 1 ).
- •
Leg ulcers are frequently (in more than 70% of cases) caused by venous disease causing AVH.
- •
The first step to promote ulcer healing is to counteract AVH.
- •
This is done conservatively by compression therapy, by elevating the leg, by walking, or by ablating the vein by means of surgery, endovascular procedures, and foam sclerotherapy.
Compression or vein surgery for ulcer healing
Several uncontrolled and nonrandomized studies have shown the beneficial effect of surgical procedures on venous ulcer healing.
Great saphenous vein crossectomy and stripping are claimed to improve venous function and heal leg venous ulcers without compression bandaging, if the deep veins are normal. Compression is always necessary when a deep venous insufficiency coexists.
Perforating vein interruption, sometimes associated with great saphenous vein stripping, has been performed to promote ulcer healing. This procedure is reported to result in rapid ulcer healing, improvement in quality of life, and significant reduction of ulcer recurrence. Studies conclude that “nihilism has no place in the management of venous disease in the 21st century”, that “surgery is indicated before an ulcer is intractable to treatment,” and that “standard surgical methods can be applied for the therapy of venous leg ulcers at any stage.”
However, 2 different meta-analyses on compression therapy demonstrated significant effectiveness in ulcer healing.
A prospective but not randomized study showed that, compared with compression, great saphenous vein surgery did not deliver better results in the ulcer healing rate; although a lower recurrence rate at 1–, 2–, and 3 years was reported.
In controlled and randomized studies the conclusions were similar :
- •
Chronic venous leg ulceration was managed by compression treatment, elevation of the leg, and exercise
- •
Addition of ablative superficial venous surgery did not affect ulcer healing, but reduced ulcer recurrence.
In one study, the treatment of venous insufficiency by hemodynamic surgery was more effective than compression, both in healing and lowering the recurrence rate.
In conclusion, there is almost general agreement that compression and surgery are equally effective in producing ulcer healing and improving quality of life; surgery is more effective than compression only in preventing ulcer recurrence.
Endovascular procedures showed a beneficial effect in the ulcer healing process, in uncontrolled nonrandomized studies. However, no comparison with traditional surgery or compression proved the greater effectiveness of these procedures.
Foam sclerotherapy was also used to speed the healing process in venous leg ulcers. Foam in adjunct to compression, proved to be effective and demonstrated outcomes similar to surgery. It seemed to accelerate the healing process. Because foam sclerotherapy is almost always associated with compression therapy, studies comparing these 2 methods in ulcer healing do not exist ( Box 2 ).
- •
Several uncontrolled and nonrandomized studies showed the beneficial effect of surgical procedures, such as great saphenous vein crossectomy and stripping and/or perforating vein interruption, on venous ulcer healing.
- •
Compared with compression, venous surgery did not reveal better results in the ulcer healing rate, but did reveal a lower recurrence rate at 1–, 2–, and 3 years.
- •
Uncontrolled, nonrandomized studies showed beneficial effect for endovascular procedures (laser and radiofrequency) and foam sclerotherapy in the ulcer healing process. Controlled randomized studies comparing these techniques with compression do not exist.
- •
There is an almost general agreement that compression and surgery are equally effective in ulcer healing and improving the quality of life; surgery is more effective than compression only in preventing ulcer recurrence.
Compression or vein surgery for ulcer healing
Several uncontrolled and nonrandomized studies have shown the beneficial effect of surgical procedures on venous ulcer healing.
Great saphenous vein crossectomy and stripping are claimed to improve venous function and heal leg venous ulcers without compression bandaging, if the deep veins are normal. Compression is always necessary when a deep venous insufficiency coexists.
Perforating vein interruption, sometimes associated with great saphenous vein stripping, has been performed to promote ulcer healing. This procedure is reported to result in rapid ulcer healing, improvement in quality of life, and significant reduction of ulcer recurrence. Studies conclude that “nihilism has no place in the management of venous disease in the 21st century”, that “surgery is indicated before an ulcer is intractable to treatment,” and that “standard surgical methods can be applied for the therapy of venous leg ulcers at any stage.”
However, 2 different meta-analyses on compression therapy demonstrated significant effectiveness in ulcer healing.
A prospective but not randomized study showed that, compared with compression, great saphenous vein surgery did not deliver better results in the ulcer healing rate; although a lower recurrence rate at 1–, 2–, and 3 years was reported.
In controlled and randomized studies the conclusions were similar :
- •
Chronic venous leg ulceration was managed by compression treatment, elevation of the leg, and exercise
- •
Addition of ablative superficial venous surgery did not affect ulcer healing, but reduced ulcer recurrence.
In one study, the treatment of venous insufficiency by hemodynamic surgery was more effective than compression, both in healing and lowering the recurrence rate.
In conclusion, there is almost general agreement that compression and surgery are equally effective in producing ulcer healing and improving quality of life; surgery is more effective than compression only in preventing ulcer recurrence.
Endovascular procedures showed a beneficial effect in the ulcer healing process, in uncontrolled nonrandomized studies. However, no comparison with traditional surgery or compression proved the greater effectiveness of these procedures.
Foam sclerotherapy was also used to speed the healing process in venous leg ulcers. Foam in adjunct to compression, proved to be effective and demonstrated outcomes similar to surgery. It seemed to accelerate the healing process. Because foam sclerotherapy is almost always associated with compression therapy, studies comparing these 2 methods in ulcer healing do not exist ( Box 2 ).
- •
Several uncontrolled and nonrandomized studies showed the beneficial effect of surgical procedures, such as great saphenous vein crossectomy and stripping and/or perforating vein interruption, on venous ulcer healing.
- •
Compared with compression, venous surgery did not reveal better results in the ulcer healing rate, but did reveal a lower recurrence rate at 1–, 2–, and 3 years.
- •
Uncontrolled, nonrandomized studies showed beneficial effect for endovascular procedures (laser and radiofrequency) and foam sclerotherapy in the ulcer healing process. Controlled randomized studies comparing these techniques with compression do not exist.
- •
There is an almost general agreement that compression and surgery are equally effective in ulcer healing and improving the quality of life; surgery is more effective than compression only in preventing ulcer recurrence.
Choice of compression in the treatment of ulcers
The prerequisite for the effectiveness of compression on venous hemodynamics is a significant narrowing of the veins with short phases of intermittent occlusion during walking to prevent venous reflux, increase the venous ejection fraction and reduce AVH.
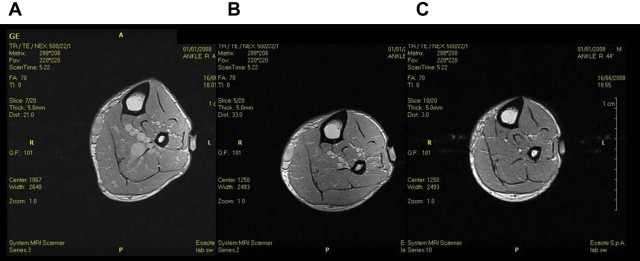
To narrow or occlude the venous system, the compression pressure must be higher than the intravenous pressure. This depends on the body position because venous pressure varies in different body positions. It has been shown that it is possible to narrow or occlude the veins with an external pressure of 20 mm Hg in the supine position, 50 mm Hg in the sitting position, and 70 mm Hg in the standing position. It was also demonstrated that in the sitting position a pressure of 40 mm Hg was enough to narrow (but not occlude) the calf veins; but when the patient was asked to do foot dorsiflexions with an inelastic cuff, the pressure increased to 60 mm Hg, resulting in vein occlusion. These data were confirmed by magnetic resonance imaging studies, which showed that in the standing position, a pressure of 40 mm Hg was not able to occlude the veins, that were only completely occluded with a pressure of 80 mm Hg ( Fig. 2 ).
In conclusion standing venous pressure can be modified by an external compression pressure higher than 60 mm Hg (defined as very strong in a recent consensus paper).
Compression materials are classified into elastic and inelastic categories. Both categories exert pressure on the leg that depends on the stretch applied to the bandage, the number of turns in the bandage, and the radius of the leg segment (Laplace law).
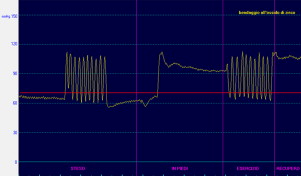
An intelligent compression system should exert a very strong pressure in the standing position and a low and comfortable resting pressure in the supine position. It should have a large difference between standing and resting pressure. This difference has been termed Static Stiffness Index (SSI) and it is one of the most important indicators of the stiffness of the bandage. Elastic material gives way to muscle expansion that results in a very low difference between the resting pressure and the pressure in standing position or during functional activities. For elastic material, the SSI is usually less than 10 mm Hg. During muscular activity, the difference between systolic and diastolic pressure termed walking pressure amplitude (WPA), another indicator of the stiffness of the bandage, is very low.
In addition elastic material tends to return to its original length when extended and its return power is directly related to the stretch applied to the bandage (squeezing effect). As a consequence, in order to produce the strong standing pressure necessary to counteract AVH, an elastic bandage must be applied at full stretch. This application method exerts a very strong pressure also in the supine position ( Fig. 3 ). The resulting bandage will be painful and intolerable to the patient and should be avoided in the clinical setting.
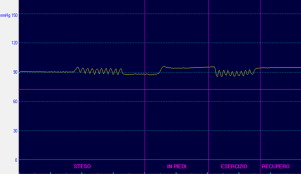
An elastic bandage should be applied at 50% of its total extensibility to avoid being painful. In this condition the supine pressure is not higher than 40 to 45 mm Hg, resulting in a standing pressure not higher than 45 to 50 mm Hg, which is not enough to occlude the veins ( Fig. 4 ).
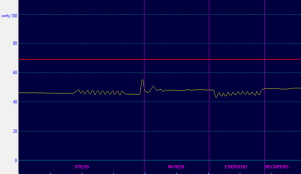
An inelastic bandage, made up of a short stretch of inextensible material, exerts its effect by resisting the increase of muscle volume during muscular contraction in the upright position and during functional activities (the leg gives way) and it does not exert any elastic return effect.
Inelastic bandages are well tolerated at rest even when applied with strong initial pressure, because the leg volume reduces immediately due to the reduction of physiological oedema, resulting in a very fast pressure loss into a tolerable range. At the same time, it exerts a much higher pressure during standing (SSI always >10) and strong or very strong pressure peaks during muscular exercise, higher than 70 mm Hg, enough to intermittently occlude the veins and restore a kind of valvular mechanism starting from a fairly low and tolerable resting pressure. For these reasons the inelastic bandage system comes close to the criteria for an ideal compression system ( Box 3 , Fig. 5 ).
- •
The pre-requisite for the effectiveness of compression on venous hemodynamics is a significant narrowing or occlusion of the vein lumen. An external pressure higher than 60 mm Hg is necessary in the standing position to occlude the veins.
- •
Compression materials are classified into elastic and inelastic materials.
- •
Elastic material is not able to achieve strong pressure in the standing position when properly applied.
- •
Inelastic material exerts a very high standing pressure and strong or very strong pressure peaks during muscular exercise. This pressure is able to intermittently occlude the venous lumen.
- •
For these reasons the inelastic bandage has a hemodynamic effect, is able to reduce AVH and should be preferred in ulcer treatment.
The practical consequences of different compression pressure profiles on venous reflux and impaired venous pumping function
Effect on Venous Reflux
Inelastic material is more effective than elastic material in reducing venous reflux in venous insufficiency. In a previous study, in patients with deep venous insufficiency, the air plethysmographic parameters venous volume (VV) and venous filling index (VFI) were reduced by increasing external pressure; the reduction was significantly greater with inelastic than with elastic compression materials because the former achieved a much higher standing pressure starting from the same supine pressure. The investigators concluded that, “using the same bandage pressure, inelastic compression material is more effective at reducing deep venous refluxes than elastic bandages, in patients with venous ulcers.”
In a more recent work we came to the same conclusion in patients affected by superficial venous insufficiency, by measuring the reflux volume automatically calculated by the Duplex scanner.
Twelve patients were examined in the standing position by means of the Duplex scanner Esaote Mylab 60 (Esaote, Florence, Italy) with a specially designed finger-like probe (Esaote IOE323 Intraoperative, Linear Array 4–13 MHz) without any compression and after the application of different compression devices from the base of the toes to the knee. This probe finger-like 12 MHz probe was fixed with tapes at the mid-thigh, on the incompetent GSV along the longitudinal axis and its position was never changed during the experiments. The reflux was elicited by tip-toe maneuvers and measured when the patient returned to the upright relaxed position after tip-toeing. After recording the baseline measurements without any compression, the authors applied elastic and inelastic devices at the same supine pressure of 20–, 40–, and 60 mm Hg. The resulting standing pressures were significantly higher with inelastic material compared with elastic and inelastic material resulted in significantly higher reduction of venous reflux. Only when the authors applied elastic bandages with 60 mm Hg pressure, the reflux was reduced to an extent similar to inelastic compression, but this high pressure was intolerable to the patient and was used only for the short duration of the laboratory test and not in daily practice.
Effect on Venous Pumping Function
Inelastic material is more effective than elastic material in improving venous pumping function that is severely reduced in venous insufficiency. In different experiments conducted on 68 patients affected by major reflux in the great saphenous vein (CEAP C3-C5 classification), the authors measured the ejection fraction (EF) of the venous calf pump by means of strain gauge plethysmography according to a previously described protocol (Poelkens and colleagues). The investigation started with leg elevation to empty the veins. The minimal volume of the leg segment proximal to the bandage was registered by the strain gauge. Then the patient stood up and the volume increase of the calf segment that reflected venous filling, was measured continuously. Venous volume (VV) is defined as the difference between empty and filled veins. During a standardized exercise (20 steps on a 20 cm high stair in 20 seconds) the volume of blood that is expelled toward the heart (EV) reflects the quality of the venous pump. The proportion of EV in relation to VV expressed as a percentage, is the EF ( Box 4 ).







