This article provides a concise description of common complications of rhinoplasty, recommendations for avoidance, and corrective techniques. The surgeon must have a comprehensive understanding of nasal anatomy and effects of surgical maneuvers to help avoid complications. Meticulous history, physical examination, and standardized photographic documentation are central to preoperative evaluation and surgical planning for rhinoplasty. Photographic documentation is useful to illustrate preexisting preoperative asymmetries. Appropriate preoperative counseling regarding appropriate postoperative expectations as well as all risks, benefits, and alternatives is critical. Any complications should be openly discussed with the patient.
Key points
- •
Meticulous history, physical examination, and standardized photographic documentation are central to preoperative evaluation and surgical planning for rhinoplasty.
- •
Photographic documentation is very useful to help illustrate preexisting preoperative asymmetries, and the surgeon must document these in the physical examination and discuss them with the patient.
- •
As with any surgery, any complications should be openly discussed with the patient.
- •
Appropriate preoperative counseling regarding all risks, benefits, and alternatives is critical.
- •
The surgeon must have a comprehensive understanding of nasal anatomy and effects of surgical maneuvers to help avoid complications.
Overview
Rhinoplasty is a very common surgical procedure among facial and general plastic surgeons. It may be performed for functional and aesthetic reasons. It is a highly technically challenging procedure, because the surgeon must pay careful attention to both form and function. An aesthetically pleasing nose without the ability to breathe is a surgical failure. Some complications may occur intraoperatively, whereas others may occur postoperatively during wound healing and contracture. Therefore, some complications may not become evident until months to years after surgery.
Overview
Rhinoplasty is a very common surgical procedure among facial and general plastic surgeons. It may be performed for functional and aesthetic reasons. It is a highly technically challenging procedure, because the surgeon must pay careful attention to both form and function. An aesthetically pleasing nose without the ability to breathe is a surgical failure. Some complications may occur intraoperatively, whereas others may occur postoperatively during wound healing and contracture. Therefore, some complications may not become evident until months to years after surgery.
Asymmetries
Asymmetries of the bony pyramid can occur for multiple reasons, including discrepancies in osteotomies between sides, asymmetric dorsal reduction, and persistence of preoperative asymmetries. A greenstick fracture, with failure to fully osteotomize, may result in either failure to fully mobilize the nasal bone or the nasal bone lateralizing from memory.
Asymmetries of the middle third are also often multifactorial. A septal deviation that was not causing asymmetry before dorsal reduction may become “unmasked” after dorsal reduction, and thereby cause asymmetries of the middle vault. Asymmetric dorsal reduction of the middle third can also occur. Palpation of the dorsum with moistened gloves allows careful assessment of the underlying anatomy after dorsal reduction.
Establishing symmetry at the tip is highly dynamic and requires an understanding of all major and minor tip support elements, as shown in Table 1 . Careful attention to tip suture technique and proper suture placement will help minimize tip asymmetries. Preexisting asymmetries of the medial and lateral crura may not be evident until other tip dynamics are altered. Similar to the middle third, a septal deviation that was not causing any asymmetry preoperatively may become “unmasked” as a result of surgical maneuvers, with resultant tip asymmetry or deviation. Contracture of the skin soft tissue envelope can also result in asymmetry of the tip over time.
| Complication | Cause | Avoidance | Correction |
|---|---|---|---|
| Asymmetry of the bony vault | Asymmetric osteotomies | Meticulous attention to osteotomies | Percutaneous osteotomies |
| Asymmetry of the middle vault | Unmasked dorsal septal deviation after dorsal reduction | Recognition of septal deviation | Crushed cartilage camouflage grafts |
| Tip asymmetry | Asymmetric tip sutures | Meticulous attention to suture technique | Revision |
| Unmasked caudal septal deviation | Meticulous inspection | Possible placement of septal extension graft Possible repositioning of caudal septum with swinging door, secure to nasal spine with suture | |
| Overresection of nasal bones | Overaggressive resection | Judicious bony dorsal reduction | Placement of dorsal onlay graft |
| Open roof deformity | Bony dorsal reduction | Judicious bony dorsal reduction when no osteotomies are planned, but unavoidable when narrowing of the bony base is planned | Lateral osteotomies to close open roof |
| Rocker deformity | Continuation of osteotomies into frontal bone | Meticulous planning of osteotomies and continuous palpation/inspection | Percutaneous osteotomies |
| Stair step deformity | Improper placement of lateral osteotomy anterior to the ascending process of the maxilla | Meticulous planning of osteotomies and continuous palpation/inspection | Percutaneous osteotomies |
| Pollybeak deformity | Overresection of nasal bones | Meticulous planning of dorsal reduction, both bony and cartilaginous dorsum | Dorsal onlay camouflage graft |
| Underresection of dorsal septum (anterior septal angle) | Appropriately match cartilaginous dorsal reduction to that of bony dorsal reduction May require revision | ||
| Postoperative soft tissue scar formation | Avoid overaggressive dorsal reduction in thick-skinned patients | Kenalog injections postoperatively | |
| Inverted V deformity | Upper lateral cartilages drop inferior and posterior, causing show of the nasal bones and dorsal septum This results from failure to repair the upper laterals to the dorsal septum after dorsal reduction | Repair upper lateral cartilages to dorsal septum after dorsal reduction Use of spreader grafts or autospreader grafts | Revision with use of spreader grafts (if upper lateral cartilage present), possible onlay crushed cartilage camouflage grafts, consider osteotomies to narrow the bony base if this is a contributing factor |
| Saddle nose deformity | Overaggressive dorsal reduction with septoplasty, resulting in a dorsal strut that is inadequate to support cartilaginous dorsum | Maintain 1.5-cm dorsal strut | Revision with dorsal onlay camouflage graft (minor cosmetic deformity) and rib cartilage graft reconstruction (severe cases) |
| Bossae | Overaggressive cephalic trim of lateral crura | Note predisposing factors for bossae formation (see below), avoid overaggressive resection | Revision with structural grafting of lateral crura (strut grafts), crushed cartilage, and/or temporalis fascia camouflage grafts |
| Visible grafts | Thin skin | Note thin skin preoperatively and place temporalis fascia overlay grafts to camouflage | Revision with possible graft removal and/or placement of temporalis fascia for contour smoothing and camouflage |
| Pinched tip | Overresection of lateral crura during cephalic trim | Spare 6- to 7-mm rim strip | Lateral crural strut grafts, possible crushed cartilage grafts for camouflage |
| Malpositioning of lateral crura | Ensure appropriate orientation and positioning of lateral crura | Removal/revision of any offending tip sutures, possible lateral crural strut grafting, possible repositioning of lateral crura | |
| Contracture from wound healing | Unavoidable, must preoperatively counsel patient about this risk and document having done so | Revision surgery with one or more of the above maneuvers | |
| Poorly defined tip | Overaggressive tip deprojection in thick-skinned patient | Avoid overaggressive deprojection | Judicious superficial nasalis aponeurotic system (SNAS) excision intraoperatively, Kenalog injections postoperatively |
| Nostril asymmetry | Altered caudal septum, medial, intermediate, and lateral crura dynamics from intraoperative suture technique or alteration | Meticulous attention to symmetric placement of sutures, such as tip and tongue in groove sutures | Revision, with correction of underlying offending cause |
| Alar retraction | Overly tight closure of marginal incision | Remove/revise offending sutures | |
| Overresection of lateral crura during cephalic trim | Lateral crural strut grafts, possible alar rim grafts (minor cases), auricular composite grafts (severe cases) | ||
| Malpositioning of the lateral crura | Repositioning of the lateral crura, lateral crural strut grafts, possible alar rime grafts (minor cases), auricular composite grafts (severe cases) | ||
| Overly tight lateral crural spanning sutures | Removal/revision of any offending tip sutures | ||
| Contracture from wound healing | Revision surgery with one or more of the above maneuvers | ||
| Columellar retraction | Overresection of the caudal septum | Avoid overresection | Caudal septal extension graft, columellar strut graft, columellar plumping graft |
| Excessive setback of the medial crura during tongue-in-groove | Avoid excessive setback | Revise tongue-in-groove, consider columellar plumping graft Septocolumellar suture can be used to help prevent contracture during wound healing | |
| Columellar and alar base scar formation | Wound healing | Meticulous wound closure | Kenalog injections with revision reserved for severe cases |
| Nasal obstruction | External nasal valve collapse | Maintain integrity and appropriate position of lateral crura, avoid overaggressive narrowing of the alar base | Lateral crural strut grafts, possible alar rim grafts |
| Internal nasal valve collapse | Avoid overaggressive narrowing of the bony base, use spreader grafts or autospreader grafts to maintain patency | Spreader or autospreader grafts | |
| Septal deviation | Appropriately address any septal deviation | Septoplasty | |
| Intranasal synechia | Careful soft tissue handling and fastidious wound closure | Lysis of synechia | |
| Recurvature of the lateral crura | Recognize contribution to the patency of the nasal airway | Lateral crural strut grafts | |
| Septal perforation | Opposing mucoperichondrial lacerations | Meticulous elevation of mucoperichondrial flaps to prevent opposing lacerations | Place fascia or crushed cartilage graft interposed between lacerations |
| Septal hematoma | Placement of septal whip sutures and use of removable soft silastic intranasal splints, prophylactic mucoperichondrial flap incision to allow drainage of any accumulated blood | Incision and drainage | |
| Costal cartilage (autograft and homograft) warping | Intrinsic property of cartilage | Concentric carving | Revision |
| Pneumothorax after costal cartilage harvest | Injury to the pleura | Harvest cartilage in subperichondrial plane | Close wound under water seal with positive pressure ventilation |
Edema of the soft tissue envelope can make asymmetries and irregularities difficult to discern intraoperatively. Thus, careful marking before injection is paramount. Asymmetries can be minimized through judicious inspection from the top of the patient’s head and through careful palpation using sterile saline-moistened gloves.
The bony pyramid
Overresection of the Nasal Bones
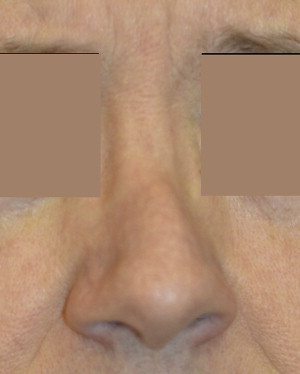
Overresection of the nasal bones can be avoided through judicious dorsal reduction, as seen in Fig. 1 . Notice that this patient also has a pollybeak deformity, which is discussed later. More bone may easily be removed, whereas replacement after overresection presents a more challenging scenario.

Open Roof Deformity
An open roof is a normal consequence of dorsal reduction. Failure to close an open roof with appropriate osteotomies will result in a “flat top” appearance to the bony pyramid, as seen in Fig. 2 . Edema of the soft tissue envelope can mask an open roof deformity on visual inspection. Again, careful palpation will make this readily apparent to the surgeon. Medial and lateral osteotomies are used to close an open roof deformity, narrowing the bony pyramid.
Rocker Deformity
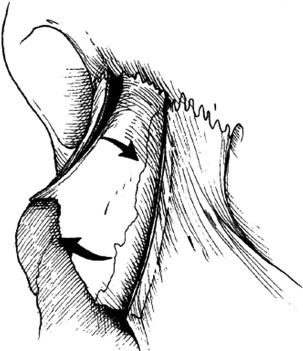
Rocker deformity results from carrying osteotomies too far superiorly up into the frontal bone without appropriate back fracture. On medialization of the nasal bones, the superior portion is cantilevered, or “rocked,” laterally, as shown in Fig. 3 . This deformity can be avoided through careful planning of one’s osteotomies. When performing an endonasal lateral osteotomy, the guarded portion of the osteotome is oriented laterally and the surgeon continually palpates during the osteotomization process. Should this complication be encountered, transverse percutaneous osteotomies may be performed to create the appropriate controlled back fracture.
Stair Step Deformity
Stair step deformity is caused by placement of the lateral osteotomy anterior to the ascending process of the maxilla, resulting in a palpable step-off. The lateral osteotomy should be placed along the ascending process (also known as the frontal process) of the maxilla in the standard high-low-high fashion, which is illustrated Fig. 4 . Careful planning of the lateral osteotomies will help the surgeon avoid this complication. The guarded portion of the osteotome is oriented laterally, and the surgeon continually palpates during the osteotomization process. In addition to careful palpation, the surgeon must listen for the distinct sound made when the osteotomy is being placed in the correct location along the ascending process of the maxilla. Percutaneous perforating lateral osteotomies also lend a degree of safety. This problem is difficult to correct, and therefore stair step deformity must be avoided.
The middle third
Pollybeak Deformity
Pollybeak deformity results when the lower third of the dorsum is more projected than the tip. This is seen in Fig. 1 . Overresection of the bony pyramid, underresection of the cartilaginous middle third (specifically the anterior septal angle), and supratip fibrosis deep to the soft tissue envelope can all result in pollybeak. The first 2 are preventable, whereas the third occurs postoperatively in the setting of wound healing. Additionally, loss of tip support with subsequent tip ptosis can result in a relative pollybeak. Palpation allows the surgeon to assess the dorsum and to determine if additional resection is necessary. Soft tissue pollybeak can be addressed with Kenalog injections to the affected area. The senior author prefers to use a very conservative Kenalog 10 mixed 1:10 or 1:5 with 1% lidocaine with 1:100,000 epinephrine. It is critical that all Kenalog be injected deep to the dermis to avoid dermal thinning. Overaggressive injection can itself cause divots from dermal or cartilaginous injury.
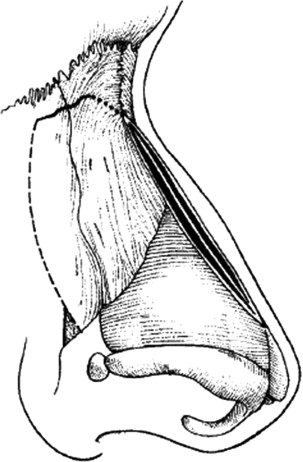
Inverted V Deformity
The inverted V deformity results from accentuated visibility of the caudal margins of the nasal bones after dorsal reduction, as seen in Fig. 5 . As illustrated in Fig. 6 , dorsal reduction causes narrowing of the cartilaginous dorsal width. As a result, the upper lateral cartilages become displaced inferiorly and posteriorly, thereby accentuating the caudal margin of the nasal bones. This deformity is further exaggerated if the bony base is not appropriately narrowed after dorsal reduction. Repair of the upper lateral cartilages to the dorsal septum and use of spreader grafts will help prevent this. The senior author routinely uses the autospreader upper lateral turn-in flaps, which are shown in Fig. 7 .







