Sub-Saharan Africa is the epicenter of the HIV pandemic and HIV-infected people are more susceptible to inflammatory dermatoses, infections, and drug eruptions. Many of the drugs used for HIV-associated opportunistic infections are associated with a higher incidence of drug-related toxicities and drug interactions. This article discusses the epidemiology, pharmacogenetics, and clinical features of idiosyncratic drug reactions in HIV-infected Africans. Special considerations in this population, including immune reconstitution inflammatory syndrome, multiple drug hypersensitivity syndrome, drug reactions in pregnancy, drug rechallenge in lichenoid drug eruptions, and anxiety/depression after cutaneous adverse drug reactions, are also briefly discussed.
Key points
- •
The incidence of cutaneous adverse drug reactions (CADRs) is high in HIV-infected persons; however, there are large gaps in knowledge about several aspects of HIV-associated CADRs in Africa, which carries the biggest burden of the disease.
- •
Gaps include epidemiology, pathomechanisms, pharmacogenetics, and management strategies.
- •
Population studies are needed to better inform policymakers and clinicians on the optimal management of HIV-associated CADRs.
- •
Some of these studies can be extrapolated from data arising elsewhere with reasonable accuracy whereas others, like pharmacogenetics, have to be done in African populations in Africa.
Introduction
Sub-Saharan Africa is the epicenter of the HIV pandemic, accounting for 68% of the global burden of the disease. The disease has changed the epidemiology and the profile of dermatology practice in Africa, with higher incidences of inflammatory dermatoses, infections, and drug eruptions compared to the general population. Although highly active antiretroviral therapy (HAART) and effective treatments for HIV-associated opportunistic infections have had a dramatic impact on reducing HIV-related morbidity and mortality, they are associated with many complications, including drug-related toxicities, drug interactions, and immune reconstitution inflammatory syndrome (IRIS). It is estimated that drug hypersensitivity reactions, related to a wide spectrum of drugs, are 2 to 100 times more common in HIV-infected persons, with the actual figure probably somewhere in-between the 2 extremes.
There are many classifications used for adverse drug reactions, and the simplest divides them into 2 types, depending on whether they are predictable and dose dependent (type A) or unpredictable and dose independent (type B). This review focuses on the latter, which accounts for 15% to 20% of all adverse drug reactions. The epidemiology and the clinical spectrum of HIV-associated type B CADRs in African populations, excluding IgE-mediated reactions, are discussed.
Introduction
Sub-Saharan Africa is the epicenter of the HIV pandemic, accounting for 68% of the global burden of the disease. The disease has changed the epidemiology and the profile of dermatology practice in Africa, with higher incidences of inflammatory dermatoses, infections, and drug eruptions compared to the general population. Although highly active antiretroviral therapy (HAART) and effective treatments for HIV-associated opportunistic infections have had a dramatic impact on reducing HIV-related morbidity and mortality, they are associated with many complications, including drug-related toxicities, drug interactions, and immune reconstitution inflammatory syndrome (IRIS). It is estimated that drug hypersensitivity reactions, related to a wide spectrum of drugs, are 2 to 100 times more common in HIV-infected persons, with the actual figure probably somewhere in-between the 2 extremes.
There are many classifications used for adverse drug reactions, and the simplest divides them into 2 types, depending on whether they are predictable and dose dependent (type A) or unpredictable and dose independent (type B). This review focuses on the latter, which accounts for 15% to 20% of all adverse drug reactions. The epidemiology and the clinical spectrum of HIV-associated type B CADRs in African populations, excluding IgE-mediated reactions, are discussed.
Epidemiology of HIV-associated CADRs in Africa
Accurate data on the incidence of HIV-associated CADRs worldwide, particularly in Africa, are limited by lack of population-based studies, inconsistency in the design of published studies, inaccurate reporting, and limitations in case definitions and disease severity grading. This applies to both CADRs in general and the individual phenotypes of drug reactions. As such, patient-related outcomes and the overall impact on the health care system of HIV-associated CADRs are largely unknown.
The limited available data from Africa in hospitalized patients and outpatient clinics suggest that the incidence is significantly higher than in the general population. Drug-induced erythroderma in HIV-infected patients ranged from 20% of all erythrodermas in a Nigerian study to 41% at a teaching hospital in Durban, South Africa. Up to 80% of the cases presenting with Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) at 2 tertiary hospitals in Cape Town, South Africa, were HIV infected.
Pharmacogenetics of CADRs in Africa
CADRs are associated with specific HLA subtypes in some populations. Good examples are the Han Chinese and many populations in Southeast Asia where SJS and TEN secondary to carbamezapine has an association with HLA-B∗1502 in almost all cases; and in both the Han Chinese and whites there is an association between HLA-B∗5801 and allopurinol-induced SJS and TEN. Abacavir-induced hypersensitivity syndrome is strongly associated with HLA-B*5701 during treatment of HIV infection, and prospective studies have shown that HLA-B*5701 screening reduces the incidence of hypersensitivity reactions. This association seems generalizable across racial groups in Asia, Europe, and the Unites States. In the only large study to date performed in Africa, however, HLA-B*5701 was not significantly associated with clinically diagnosed abacavir hypersensitivity reaction in patients of African race from Uganda. Pharmacogenetics of CADRs are drug specific and population specific, and more studies in Africa are needed to characterize the association between genetic predisposition and HIV-associated CADRs as the world moves toward individualized medical therapies and diagnostics.
Types of CADRs
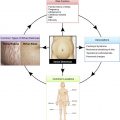
Types of HIV-associated CADRs range from mild transient eruptions to severe life-threatening forms. The clinical features can either be confined to the skin or be part of a multisystem disorder. They include morbiliform drug eruptions, SJS and TEN, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. There are other types of CADRs, however, that do not seem to be higher in HIV-infected persons compared with the general population. These include urticaria, lichenoid drug eruptions, fixed drug eruption (FDEs), acute generalized exanthematous pustulosis, photodermatitis, and cutaneous vasculitis.
A specific drug is generally not associated with a specific phenotype of CADR and a specific type of CADR can be due to any drug. A case in point is nevirapine, which is strongly associated with SJS and TEN, morbilliform eruptions, and DRESS in both adults and children. There are, however, certain drugs that are more commonly associated with some types of CADRs. A good historical example is thioacetazone, which was strongly associated with SJS and TEN in tuberculosis and HIV coinfected patients, leading to the World Health Organization recommending avoidance of the drug with subsequent decline of its use worldwide.
Morbiliform Drug Eruptions
Morbilliform (measles-like) drug eruptions, also referred to as maculopapular rash, account for 95% of all cases of CADRs. The rash presents as centrifugally spreading erythematous macules and papules that sometimes become confluent. Morbilliform drug eruptions are usually self-limiting and treatment interruption is not necessary. They are differentiated from DRESS by a lack of systemic involvement and from SJS and TEN by absence of epidermal necrosis and mucositis. At the initial presentation, however, these differences may not be obvious and attending clinicians should be aware of the possibility of progression to more severe disease Fig. 1 .
Drug Rash with Eosinophilia and Systemic Symptoms
DRESS syndrome or drug hypersensitivity syndrome is characterized by prodromal symptoms of pruritus and pyrexia followed by fever, edema, lymphadenopathy, leukocyte abnormalities (leucocytosis, eosinophilia, and/or atypical lymphocytosis), hepatitis, and a long latency period (>3 weeks). Rarely nephritis, pancreatitis, pneumonitis, and myocarditis are the other systemic features. The rash presents as a ubiquitous exanthema that may be urticarial, maculopapular, vesicular, pustular, purpuric, targetoid, or erythrodermic. Visceral involvement differentiates DRESS syndrome from the other eruptions that are not drug related, including viral exanthemata, inflammatory conditions, and HIV-associated atypical cutaneous lymphoproliferative disorders. Because the clinical features can be identical, irrespective of the cause, these have to be excluded Fig. 2 . There are few data suggesting that DRESS syndrome is more common in persons with African ancestry and it is well established that in Africa the incidence is higher in HIV-infected persons.
As in all types of CADRs, early withdrawal of the offending drug(s) improves outcomes in DRESS. In mild disease, characterized amongst others by transaminitis less than 5 times the upper limit of normal, absence of pneumonitis, hemophagocytosis or pancreatitis, topical steroids with emmolients, and antihistamines are usually effective. In severe disease, systemic steroids are warranted. Based on the authors’ experience, in most cases, the rash is mild and responds to topical steroids. The severity of the rash, however, is not always proportional to the severity of the systemic involvement and the abnormal laboratory parameters may persist for several days to several months after withdrawal of the offending drug.
The most common causes of death in DRESS syndrome are liver failure and sepsis. DRESS syndrome–associated mortality in HIV is unknown, but in the general population it is estimated to be between 3.7% and 10%. DRESS syndrome is associated with long-term sequelae and in darker skin these include persistent postinflammatory hyperpigmentation, chronic exfoliative dermatitis, cutaneous scarring, and nail changes. There are emerging reports of patients developing autoimmune diseases after DRESS syndrome. These reports need further validation in larger prospective studies.
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis
SJS and TEN are considered on the spectrum of the same disease. They are delineated by percentage body surface area of epidermal necrosis and stripping. In SJS there is less than 10% of epidermal detachment and in TEN there is greater than 30%. SJS/TEN overlap lies between these 2 extremes. Rarely, systemic features are present. The early clinical features, often confused with upper respiratory tract infection, include fever, malaise, cough, stinging eyes, and a sore throat. This is followed by rapid progression to epidermal necrosis and detachment, mucositis, and painful blistering of the palms and soles Fig. 3 . The incidence of SJS and TEN is as high as 1 to 2 per 1000 individuals in HIV-infected cohorts, much higher than in the general population. Of all CADRs, TEN has the highest mortality, of up to 35%, as reported in a South African population. In most cases, mortality is due to skin and mucosal failure, resulting in bacterial systemic infections. It is controversial whether systemic steroids and intravenous immunoglobulins are beneficial in SJS and TEN but there is a general consensus that antibiotics should only be used in the presence of clinical and/or microbiological features of an infection. Supportive therapy is the mainstay of treatment paired with a multidisciplinary approach.
SJS and TEN are debilitating diseases with long-term sequelae of varying severity. These range from moderate dry eye syndrome to blindness; esophageal strictures; hematocolpos, vulvovaginal synechiae, and fibrosis; heterotrophic calcifications; dyspigmentation; and hypertrophic scars Fig. 4 . The authors have recently shown a higher incidence of depression and anxiety in a predominantly HIV-infected cohort of SJS and TEN cases 6 weeks after the resolution of acute symptoms. Considering the high incidence of SJS and TEN in HIV-infected people, there are few studies documenting and advising on the management of long-term sequelae in this population.
Lichenoid Drug Reactions
Lichenoid drug reactions (LDRs) are characterized by violaceous macules and plaques on the skin and are characteristic white lace pattern, called Wickham striae, in the mucosae. The authors have encountered a few cases of LDRs in HIV-infected persons, mainly related to antituberculosis drugs. The incidence of LDRs in HIV does not seem higher than in the general population. The challenge in LDRs is the lack of acute markers, insidious onset of the rash, wide variation in the intervals between drug initiation, and a clinically detectable rash. All these make it difficult to establish a temporal relationship with the offending drug and ascribe causality. In cases of polypharmacy with limited number of effective drugs, as is the case in the treatment of AIDS and tuberculosis, this creates a major therapeutic conundrum. In tuberculosis-associated LDRs, the authors’ experience has shown that sometimes the benefits of continuing therapy outweigh the risks of ongoing CADRs and treatment is carried through to completion of the course. This results in increasing and persistent hyperpigmentation, focal areas of depigmentation, hyperkeratosis, and painful fissuring of the skin, all of which seem more severe in darker African skin Fig. 5 . Potent topical steroids and phototherapy can be used to control the eruption until the course is completed.