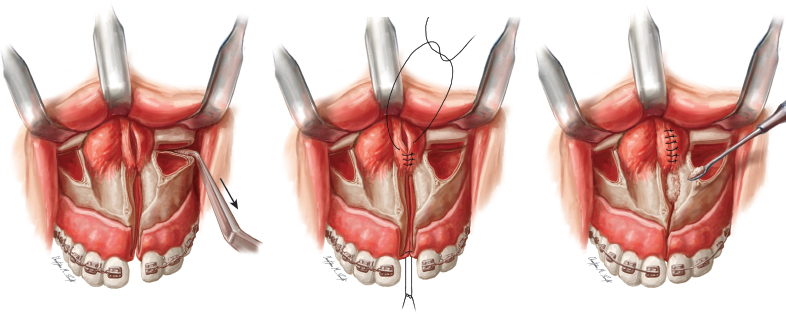
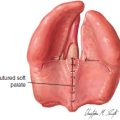
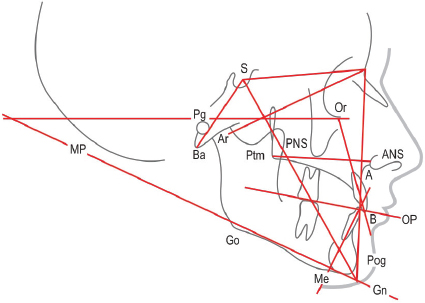
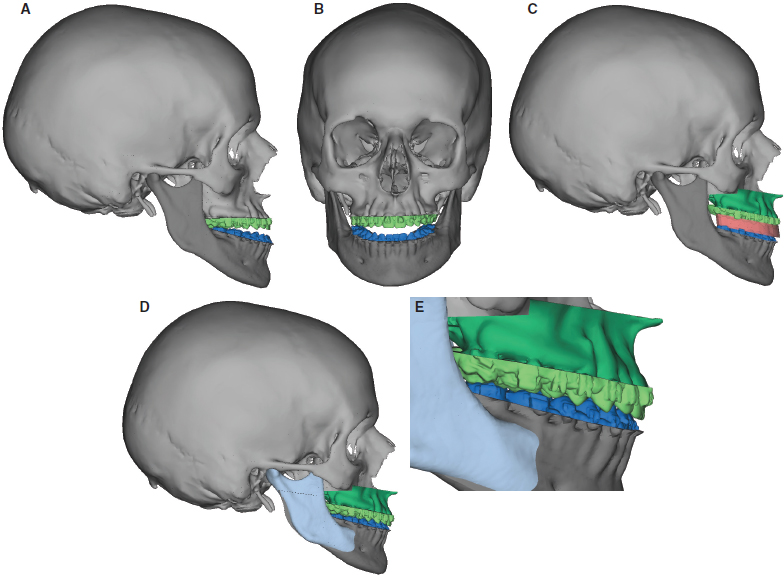
72 ○ Dentofacial deformities, specifically maxillary hypoplasia resulting in class III malocclusion, are typical in the cleft lip and palate population. Of patients in this group, 25% to 30% will require orthognathic surgery. ○ The cause of maxillary hypoplasia remains unclear. Some evidence supports the theory that inelasticity of scar tissue restricts facial growth and suggests an intrinsic growth deficiency that is unrelated to surgery. ○ Team management of patients with cleft lip and palate is essential to ensure that all cleft-related issues are addressed when planning surgery and that procedures are optimally timed. ○ Because maxillary advancement may affect both velopharyngeal function and articulation, a complete speech evaluation before surgery helps to prepare both the surgeon and the patient for possible postoperative changes. ○ Although orthognathic surgery may improve articulation, it may come at the expense of velopharyngeal function. ○ The maxilla is typically deficient in all three cardinal directions. Transverse deficiency is addressed with earlier maxillary expansion or with a two-piece LeFort I segment, whereas vertical and anteroposterior deficiency is addressed with orthognathic surgery. The mandible is rarely prognathic. ○ A surgical splint, fashioned during the preoperative planning, is essential to orient the new position of the maxilla to the mandible. ○ Ensuring that the condyles are seated as the maxillomandibular complex is rotated to its new vertical position is extremely important. Orthognathic surgery is the term used to describe surgical movement of the maxilla, mandible, or both jaws. The goal of orthognathic surgery is to establish ideal dental occlusion with the jaws in a position that optimizes facial form and function. Patients who undergo surgical correction of cleft lip and palate in infancy commonly develop dentofacial deformities, and 25% to 30% will have severe enough midface retrusion to require orthognathic surgery. Maxillary hypoplasia resulting in class III malocclusion is typical in this patient population. The etiology behind maxillary hypoplasia remains unclear. Some evidence supports the theory that the inelasticity of scar tissue from surgical procedures restricts facial growth.1,2 However, Weinzweig et al3 have demonstrated midface retrusion in an unoperated caprine model of palatal clefting, suggesting that an intrinsic mechanism may play a role in the midface deficiency associated with cleft palate. Although mild class III malocclusions may be camouflaged with orthodontics alone, orthognathic surgery is needed to ideally correct the class III dentofacial deformity. The chance of a favorable surgical outcome is optimized if presurgical planning is performed with a cleft and craniofacial team. Speech pathologists play an integral role in the evaluation of the velopharyngeal mechanism and the potential effects that maxillary advancement may have on nasalance, nasality, and articulation. A preoperative perceptual speech evaluation may yield information that can aid in predicting postoperative hypernasality. The orthodontist’s role in the preoperative evaluation and management is critical. Before surgery, the potential surgical candidate requires a comprehensive workup that includes an analysis of the occlusion and the age of the facial skeleton. If orthognathic surgery is attempted before the facial skeleton reaches maturity, the need for revision surgery will be increased because of unpredictable postoperative growth. Skeletal growth is usually complete between the ages of 14 and 16 years in females and between the ages of 16 and 18 years in males. The maturity of the facial skeleton and the cessation of growth can be assessed by serial cephalometric radiographs or by looking for epiphyseal closure in hand radiographs. A thorough medical and dental history is important for every patient. Systemic diseases such as juvenile rheumatoid arthritis, diabetes, and scleroderma may affect the treatment planning. Each patient should be questioned regarding symptoms of temporomandibular joint (TMJ) disease or myofascial pain syndrome. Motivation and realistic expectations are extremely important to ensure an optimal outcome. Several factors make this surgery more difficult in patients with cleft lip and palate. The patient must understand that some revision surgery and bone grafting may be needed to complete dental rehabilitation. Bone grafts are commonly necessary if edentulous spaces are to be restored with osseointegrated implants. Because implants cannot be moved orthodontically, they are placed after jaw surgery and postoperative orthodontics. The patient must have a clear understanding of the procedure, the recovery, and the anticipated result before surgery. Orthognathic surgery is a major undertaking, and the patient should be appropriately motivated to undergo all necessary perioperative orthodontic treatment and rehabilitation to achieve the desired result. A complete physical examination should be performed on every patient before surgery. The frontal facial evaluation begins with the assessment of the vertical facial thirds: trichion to glabella, glabella to subnasale, and subnasale to menton. Each of these facial thirds should be about equal. If the lower two thirds of the face is short, as is often seen in patients with clefts, it can be increased by inferiorly positioning the maxilla, resulting in an increased distance from the glabella to the pogonion. In contrast, a long lower face may benefit from a maxillary impaction, which would have the opposite effect. The most important factor in assessing the vertical height of the maxilla is the degree of incisor showing while the patient’s lips are in repose. A man should show at least 2 to 3 mm, whereas as much as 5 to 6 mm is considered attractive in a woman. If the patient shows the correct degree of incisor in repose but shows excessive gingiva in full smile, the maxilla should not be impacted. Correct incisor show in repose is more important than in full smile. The surgeon would not want to bury the incisors in repose just to reduce the degree of gingival show in full smile. Lip incompetence or mentalis strain are usually indicators of vertical maxillary excess. The intercanthal distance should be approximately equal to the distance between the medial and lateral canthi of each eye. The soft tissue envelope of the upper face also should be evaluated for descent of the malar fat pads and the severity of the nasolabial creases. These changes are associated with aging; however, skeletal movements of the maxilla will also affect these areas. The surgeon must realize that skeletal expansion (anterior or inferior repositioning) will improve the creases and folds, resulting in a more youthful appearance, whereas skeletal contraction (posterior or superior repositioning) will accentuate these problems.4 The surgeon must avoid prematurely aging the patient. However, the surgeon can typically take advantage of skeletal expansion to reduce some of these soft tissue creases, giving the patient a youthful appearance and reducing the signs of aging. In evaluating the chin, the clinician should assess the labiomental angle. An acute angle may indicate a short or prominent chin, whereas an obtuse angle and effacement of the labiomental crease typically indicates excessive vertical length or insufficient anterior projection. The inferior orbital rims, malar eminence, and piriform areas are evaluated for the degree of projection. These regions often appear deficient in patients with clefts, which is an indication for maxillary advancement; if they are prominent, posterior repositioning may be necessary. The alar base width should also be assessed before surgery, because orthognathic surgery may alter this width and thus accentuate any asymmetries associated with a cleft nasal deformity. Asymmetries of the maxilla and mandible should be documented on physical examination, and the degree of deviation from the facial midline noted. The profile evaluation focuses on the projection of the forehead, malar region, maxilla and mandible, nose, chin, and neck. An experienced clinician can usually determine whether the deformity is caused by the maxilla, the mandible, or both simply by looking at the patient. This assessment is made clinically and verified at the time of cephalometric analysis. The intraoral exam should begin with an assessment of oral hygiene and periodontal health. These factors are critical for successful orthodontic treatment and surgery. Any retained deciduous teeth or unerupted adult teeth are noted. The occlusal classification is determined, and the degrees of incisor overlap and overjet are quantified. The surgeon should assess the transverse dimension of the maxilla, because prior cleft palate repair will often result in transverse growth restriction. If the mandibular third molars are present, they must be extracted 6 months before sagittal split osteotomy. Any missing teeth or periapical pathology should be noted, as should any signs or symptoms of TMJ dysfunction. These issues should be addressed before proceeding with orthognathic surgery. The term dental compensation is used to describe the tendency of teeth to tilt in a direction that minimizes dental malocclusion. For example, in a patient with an overbite (angle class II malocclusion), lingual retroclination of the upper incisors and labial proclination of the lower incisors minimize the malocclusion. The opposite occurs in a patient who has dental compensation for an underbite (angle class III malocclusion). Thus dental compensation, which is often the result of orthodontic treatment, will mask the true degree of skeletal discrepancy. Precise analysis of the dental compensation is done on the lateral cephalometric radiographs. The patient who presents with a cleft lip or palatal anomaly will have several anatomic differences when compared with an unaffected patient. The maxilla is typically deficient in both the anteroposterior and vertical dimensions. Because the midface retrusion can be significant, the mandible commonly appears to be prognathic, but the mandible rarely demonstrates a true prognathia. It is a relative prognathia secondary to the maxillary deficiency. Finally, because of lesser segment collapse, the dental midline is often deviated toward the cleft side. If the patient desires surgical correction of the deformity, presurgical orthodontics will straighten the teeth to a more upright position and decompensate the occlusion, thereby reversing the compensation that has occurred. This has the effect of exaggerating the malocclusion, but it also allows the surgeon to maximize skeletal movements. If the patient is ambivalent or not interested in surgery, mild cases of malocclusion may be treated by further dental compensation, which will camouflage the deformity and restore proper overjet and overlap. A commitment to surgery must be made before orthodontic therapy, because the dental movements necessary for decompensation and compensation are in opposite directions.5 A cephalometric analysis and comparison to normative values can help the surgeon plan the degree of skeletal movement necessary to achieve both an optimal occlusion and an optimal aesthetic result. A lateral cephalometric radiograph is performed under reproducible conditions so that serial images can be compared. This film is usually taken at the orthodontist’s office using a cephalostat, an apparatus specifically designed for this purpose, and a head frame to maintain consistent head position. The surgeon must be able to visualize bony and soft tissue features on the image to facilitate tracing all the landmarks: the sella, inferior orbital rim, nasion, frontal bone, nasal bones, maxilla, maxillary first molar and central incisor, external auditory meatus, condylar head and mandible, and mandibular first molar and incisor. The soft tissue of the forehead, nose, lips, and chin are also traced. After the normal structures are traced, several planes and angles are determined (Fig. 72-1). The maxillary plane is a line drawn between the anterior nasal spine (ANS) and posterior nasal spine (PNS). The occlusal plane is drawn between the occlusal surfaces of the teeth. The mandibular plane is drawn between the menton and gonion, and the Frankfort horizontal plane is delineated between the superior portion of the external auditory meatus (porion) and the inferior orbital rim (orbitale). Analysis of these planes aids in establishing an accurate diagnosis. The SNA and SNB are the two most important angles in determining the relative positions of the maxilla and mandible to each other as well as to the cranial base. These angles are determined by drawing lines from the sella to the nasion to the A point or B point, respectively. By forming an angle with the sella and nasion, this position is related to the cranial base. The maxilla will be considered first. The A point represents the anteroposterior position of the maxilla. If the SNA angle is excessive, the maxilla exhibits an abnormal anterior position relative to the cranium. If the SNA angle is smaller than normal, the maxilla is posteriorly positioned relative to the cranial base, typical in patients with a cleft who require surgery. The same principle applies to the mandible; the only difference is that the B point is used to relate mandibular position to the cranial base. The importance of the cranial base as a reference is that it allows the clinician to determine whether one or both jaws contribute to the deformity. For example, a patient’s class III malocclusion (underbite) could have several different causes: a retrognathic maxilla and normal mandible, a normal maxilla and a prognathic mandible, a retrognathic mandible and a more severely retrognathic maxilla, or a prognathic maxilla and a more severely prognathic mandible. All of these conditions yield a class III malocclusion, but each requires a different treatment approach. The surgeon can delineate the true cause of the deformity by independently quantifying the maxilla and mandible to a stable reference point, the cranial base. Next, cephalometric tracings are performed. Fig. 72-1 The cephalometric radiograph is used to identify skeletal landmarks used in determining the lines and angles that reflect facial development. These measurements aid in determining the extent to which each jaw contributes to the dentofacial deformity. (A, A point, the innermost point in the depth of the concavity of the maxillary alveolar process; ANS, anterior nasal spine; B, B point, the innermost point on the contour of the mandible between the incisor tooth and the bony chin; Gn, gnathion, the center of the inferior contour of the chin; Go, gonion, the most inferior and posterior point at the angle formed by the ramus and body of the mandible; Me, menton, the most inferior point on the mandibular symphysis; MP, mandibular plane, a line tangential to the gonion and menton; Or, orbitale, the lowest point on the inferior margin of the orbit; Pg, pogonion, the most anterior point on the contour of the chin; PNS, posterior nasal spine; S, sella turcica, the midpoint of the sella turcica.) Cephalometric tracings give the surgeon an idea of how skeletal movements will affect one another and the soft tissue profile. They also allow the surgeon to determine the distances the bones will be moved to achieve the goals of the specific procedure. Different tracing methods using acetate paper are used for isolated maxillary, isolated mandibular, or two-jaw surgeries. Much of the traditional hand cephalometric tracing, however, has been replaced by computer-aided cephalometric analysis, which allows the surgeon to electronically position the maxilla and mandible on the cephalogram while recording the soft tissue changes and measuring the degree of repositioning. Complete dental records, including mounted dental casts, are needed to execute preoperative model surgery and fabricate surgical splints. Casts allow the surgeon to evaluate the occlusion both before and after articulation into proper positions. Analysis of new occlusion gives the clinician an idea of how intensive the presurgical orthodontic treatment plan will be. Casts also allow the clinician to distinguish between absolute and relative transverse maxillary deficiency. Absolute transverse maxillary deficiency presents as a posterior crossbite with the jaws in class I relationship. A relative maxillary transverse deficiency is commonly seen in a patient with a class III malocclusion. A posterior crossbite is observed in this type of patient, raising suspicions of inadequate maxillary width. However, as the maxilla is advanced or the mandible retruded, the crossbite is eliminated. Articulation of the casts into a class I occlusion allows the surgeon to easily distinguish between relative and absolute maxillary constriction. Fig. 72-2 Three-dimensional CT reconstruction of a patient with class III malocclusion and an anterior open bite. A and B, Preoperative views. C, After simulation of a LeFort I osteotomy with placement of an intermediate splint. D, After simulation of LeFort I and bilateral sagittal split osteotomies with correction of class III malocclusion and anterior open bite. E, Predicted postoperative occlusion. Several commercially available computer-assisted design (CAD) programs can assist the surgeon with some or all of the preoperative patient preparation. A conventional CT scan can be obtained; however, cone beam CT scans offer a comparable image quality with considerably less cost and radiation exposure (50 uSv compared with 2000 uSv). A cephalometric analysis can then be performed, as can simulated movements of the jaws and chin in any dimension. Once the osteotomy movements are verified by the surgeon, CAD/computer-aided manufacturing (CAM) technology is used to fabricate surgical splints for the patient.6 If necessary, three-dimensional models can be made of the patient that show the exact proposed movement (Fig. 72-2). Some systems can actually “wrap” a two-dimensional digital image around the soft tissue envelope of the three-dimensional CT image, thus replicating a three-dimensional image of the patient’s actual face in color. The patient will have multiple visits at the surgeon’s office and undergo a thorough discussion of the surgical options before agreeing on a proposed plan. Good oral health must be achieved. Preoperative orthodontics are used to level, align, and decompensate the occlusion. Based on the physical and radiographic exams, a treatment plan is developed that will achieve a class I occlusion and optimize form and function. Cephalometric tracings are used to determine the distances the jaws will have to move to achieve the desired result, and model surgery is performed to develop surgical splints that will intraoperatively position the jaws into the position determined by the cephalometric tracing.7 If a sagittal split osteotomy is going to be performed, the lower third molars should be removed 6 months before surgery to reduce the chance of an unfavorable split. Similarly, if a segmental osteotomy is planned, the orthodontist will diverge the root apices on either side of the proposed osteotomy to minimize the chance of damage to tooth roots. The surgeon should verify the splints fit and that good surgical lugs have been applied to the arch wire. Soldered lugs work the best. If the lugs break in surgery, the proper application of the splint can be compromised, making an ideal result much more difficult to obtain. Autodonation of packed red blood cells is useful for two-jaw surgery. Despite previous alveolar bone grafting, many patients have deficient or missing bone in the region of the alveolus. Palatal fistulas may persist as well. The lateral incisor is commonly missing in these patients, and closure of this space must be taken into consideration at the time of treatment planning. If a large fistula is present in the alveolus, modifications of the LeFort I procedure can be performed to facilitate a tension-free alveolar closure. These are discussed in the next section. Several principles have broad application to jaw surgery. Blood loss can be substantial in maxillofacial surgery, and even small volumes can have significant clinical implications in the pediatric population. Standard techniques of head elevation, hypotensive anesthesia, blood donation, and administration of erythropoietin are useful adjuncts to reduce blood loss, especially in the younger population. Before incisions are made, an antimicrobial rinse is helpful to minimize the intraoral bacterial count. A topical steroid is applied to the lips to reduce pain and swelling associated with prolonged retraction. Intravenous steroids may also be useful to reduce postoperative edema. The occlusion desired may not be the same as maximum intercuspal position. The splint is useful in maintaining the occlusion in the desired location in this case. Closing a posterior open bite is easy, but closing an anterior open bite with orthodontic treatment is very difficult. Ending with the anterior teeth and the canines in a class I relationship without an open bite is important. Guiding elastics are useful postoperatively to control the bite. Class II elastics are placed in a vector to correct a class II relationship (the maxillary lug is anterior to the mandibular lug). Class III elastics are applied to correct a class III discrepancy. With rigid fixation, elastics will not correct malpositioned jaws; they serve only to help the patient adapt to the new occlusion. Minor malocclusions can be corrected with postoperative orthodontic treatment. Certain skeletal movements are inherently more stable than others. Stable movements include mandibular advancement and superior positioning of the maxilla. Movements with intermediate stability include maxillary impaction combined with mandibular advancement, maxillary advancement combined with mandibular setback, and correction of mandibular asymmetry. The unstable movements include posterior positioning of the mandible and inferior positioning of the maxilla. The least stable movement is transverse expansion of the maxilla. Long-term relapse with rigid fixation has not been demonstrated to be clearly superior to nonrigid fixation in single-jaw surgery. However, in two-jaw surgery, rigid fixation results in less relapse. The judgment of the surgeon will dictate the extent to which the facial skeleton can be expanded without resulting in unacceptable relapse. The maxilla is associated with the descending palatine artery, the infraorbital nerve, the tooth roots, and the internal maxillary artery. The internal maxillary artery runs about 25 mm from the pterygomaxillary junction, and the descending palatal artery descends into the posteromedial maxillary sinus. The infraorbital nerve exits the infraorbital foramen below the infraorbital rim along the midpupillary line. The maxillary tooth roots extend within the maxilla in a superior direction. The canine has the longest root and is usually visible through the maxillary cortical bone. The important structures in the mandible that may be injured in the mandibular osteotomy are the mental nerve, the inferior alveolar nerve, and the tooth apices. The third branch of the trigeminal nerve enters the mandibular foramen to become the inferior alveolar nerve. It runs below the tooth roots and exits at the level of the first and second premolars through the mental foramen. The region where it is most medial to the outer cortex is located near the external oblique ridge. This is where the vertical portion of the bilateral sagittal split osteotomy is made, because it affords the largest margin of error. The preoperative vertical position of the maxilla is recorded by using a large caliper to measure the distance between the medial canthus of the right eye and the right central incisal edge. In a patient with a unilateral cleft lip, the standard incision can be made with little jeopardy to the premaxillary blood supply. Each side of the cleft has an incision made similar to that of the alveolar bone graft incision, facilitating a two-layer closure of the palatal and nasal mucosa. If bone needs to be grafted at this time, it can be placed into the alveolar gap after fixation has been applied. If a wide fistula is present, the surgeon can compress the maxillary segments to reduce the size of the alveolar space, ensuring the soft tissue closure is under minimal tension and the chance of fistula closure is optimized (Fig. 72-3). The canine may now be adjacent to the central incisor, but the restorative dentist can fabricate a prosthetic crown for the canine to make it look like a lateral incisor. In a patient with a bilateral cleft, care must be taken not to make the vestibular incision across the premaxilla. The premaxillary blood supply will be from the vomer and the buccal mucosa. Because the vomer will be split, the majority of blood flow to the premaxilla will be from the premaxillary buccal mucosa. A circumvestibular incision that violates this mucosa will severely jeopardize the blood supply of the premaxillary segment. To minimize the risk of complications, the incision is stopped just lateral to the alveolar cleft on each side. The reflection of the mucosa from the premaxilla is minimized to preserve the blood supply. The osteotomy of the premaxillary segment is made from a posterior approach just anterior to the incisive foramen. This allows mobilization of the segment without violation of the buccal mucosa. Similar to the unilateral cleft maxilla, residual fistulas and inadequate alveolar bone may be present. If either is identified, they can be corrected by a two-layer mucosal closure and bone grafting into the alveolar defect. If large gaps are present that may jeopardize fistula closure, the segments can be compressed at the alveolar gaps to reduce tension of the repair (Fig. 72-4). Postoperative orthodontics and prosthetic restorations of the teeth can correct almost any postoperative dental aesthetic irregularities.
Cleft and Craniofacial Orthognathic Surgery
Jesse A. Goldstein, Stephen B. Baker
KEY POINTS
PREPARATION FOR SURGERY
Physical Examination
Cephalometric Analysis and Models
Preoperative Treatment
SURGICAL TECHNIQUE
General Principles
LeFort I Osteotomy
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine