As a critical part of overall facial esthetics, the chin must be considered when patients present with complaints of facial asymmetries or aging, such as jowls or an aging neck, in particular. Chin height, width, and anterior projection should be carefully evaluated, as certain augmentation modalities may be better suited to address specific anatomic deficits. Although there are rare adverse events, dermal fillers offer a minimal down-time option, often at a more affordable cost relative to invasive surgeries and have proven to be both safe and highly effective in addressing deficits in any dimension.
Key points
- •
The appearance of the chin plays a key role in overall facial balance.
- •
Traditional procedures, such as chin implants, osseous genioplasties, and autologous grafting, may augment the appearance of the chin; however, they are invasive and associated with risks and down-time.
- •
Hyaluronic acid fillers are a safe and well-studied treatment to optimize chin dimensions and alignment.
- •
While injection techniques vary, most injectors target the pogonion, menton, and prejowl sulci for an overall positive augmented effect.
Introduction
The chin is one of the key features for overall facial appearance and symmetry [ ]. Appearance of the chin, and its relationship to and proportionality with surrounding facial structures and to the neck are paramount to overall aesthetic balance [ ]. Patients may present with concerns, for example, of a large nose, sagging neck, or jowls, failing to recognize the deficiency is lack of proportionality and alignment of the chin [ , ]. Herein, we will review the considerations and current practices for chin augmentation. We include a brief overview of surgical techniques such as alloplastic implants, autologous grafts, and osseous genioplasty and have focused on less invasive approaches, namely dermal fillers, for a more in-depth discussion of procedural technique.

Anatomic Considerations
The bony anatomy of the chin is defined by the underlying mandibular structure [ ]. This provides the backbone for the anatomic planes of the chin, including projection, height, and width. The pogonion is the most anterior-projecting portion of the chin [ , ]. The height of the chin is defined by the menton, the most inferiorly projecting skeletal portion of the chin [ , ]. The midpoint between the pogonion and the menton is the gnathion [ ]. The paragonion protrudes on the lateral sides of the pogonion and defines chin width [ ]. These surface landmarks that define the chin compartment demarcate it from the jowl and submental compartments [ ]. The muscles of the chin include the depressor anguli oris, depressor labii inferioris, and the centrally paired mentalis. The mental arteries serve as the primary blood supply to the chin, exiting via the mental foramina on the lateral chin at the second bicuspid [ ]. The inferior labial artery, labiomental artery, and submental artery also provide anastomotic arterial supply [ ]. Finally, the inferior alveolar nerve which travels through the mandible and exits as the mental nerve provides the primary innervation to the chin and lower lip [ , ].
Options for Chin Augmentation
Alloplastic implant
Alloplastic surgical chin implantation has been cited as the most studied technique of chin augmentation [ ]. It is well-suited for addressing inadequate chin projection; however, it is a suboptimal option for patients without adequate chin height or with chin asymmetry [ , ]. The procedure is safe and offers a permanent surgical option for chin augmentation [ , ]. Various materials may be used, available in different sizes and readily customizable to fit patient characteristics. For example, customized 3-dimensional (3D) printed implants are options to address mandibular asymmetries, though they may come at a higher financial burden. It is, nonetheless, an invasive surgical procedure, carrying risks of surgical intervention including hematomas, scar, hypergranulation for oral incisions, dehiscence, and infection [ , ]. Silicone implants, which are frequently used, can be associated with bone resorption, as well as dental erosion depending on its placement [ ]. This may be obviated through fixation to the bone with a screw to prevent motion at the interface of the bone and implant. Over time, there is a low risk of malpositioning and displacement of the implant. Overall, however, when executed and secured properly, there is a very low complication rate for solid silicone implants.
Osseous genioplasty
Osseous genioplasty is a surgical technique that can address complex deformities of the chin, with the ability to augment all planes including projection, height, and width [ ]. It affords a permanent solution to microgenia [ ]. This procedure involves an osteotomy with intraoperative chin advancement and fixation with metal hardware in order to reapproximate the chin [ ]. When compared with the alloplastic implant, an osseous genioplasty is a more invasive, complex technique with longer recovery time [ , ]. In addition to the invasiveness of this approach, the complexity of the procedure lends itself to being less commonly performed [ , , ].
Autologous grafts
Autologous grafts may also be used in the correction of chin deformities. Bone grafts may be obtained for augmentation purposes if patients are undergoing an additional procedure. Fat grafting may be performed as a single intervention or adjunctive to an alloplastic implant or osseous genioplasty [ ]. Fat grafting offers the ability to augment the chin in all 3 planes, however, patients with significant retrognathia are not good candidates. This is because excessive volume correction, for example, a projection change greater than 3 to 5 mm, can lead to chin ptosis [ ]. The less invasive nature has increased attractiveness to patients; however, the procedure can fail to produce reliable outcomes due to variable graft survival [ , , ]. In addition, a prospective study reported a 17.7% mean fat resorption rate at 6 months, regardless of what fat volume was injected [ , ]. Therefore, it is not a permanent solution and if used alone, will require patients to undergo repeated treatments over time.
Dermal fillers
According to the American Society for Plastic Surgery, surgical chin augmentations are down 38% compared with the year 2000 [ ]. Although the reasons for this decline are multifaceted, in part, it is likely attributable to the increasing popularity of less invasive modalities, such as dermal fillers [ , , , ]. Dermal fillers are able to shape the chin in all 3 planes thus treating chin retraction, horizontal and height deficiencies, and asymmetry. While various dermal fillers are available, hyaluronic acid (HA) fillers are especially popular, as they offer the benefit of being a simple outpatient procedure, and reversibility in the event of complications or patient dissatisfaction. Furthermore, an added benefit of fillers is the ability to trial augmentation of the chin in a nonpermanent fashion to preliminarily assess the esthetic effect prior to a permanent implantation. Dermal fillers also often come at a lower financial burden to patients as compared with surgical interventions. While fillers are designed to last up to 2 years, in our experience chin filler often lasts much longer [ ]. Filler injections are generally safe and well-tolerated, with adverse effects mainly limited to pain, redness, bruising, and swelling which subside within several days of the injections [ , ]. Severe reactions are rare and will be elaborated on further below.
Treatment selection
Advantages and disadvantages exist for each of the options for chin augmentation. Ultimately, treatment selection is influenced by both the practitioner’s evaluation of the patient, comfort with various procedures, and the patient’s individual desire. Facial and plastic surgeons, for example, may be more accustomed to alloplastic chin implants, whereas dermatologists are more apt to recommend soft tissue fillers [ ]. This, combined with a patient’s tolerance for down-time and/or willingness to undergo a surgical procedure requiring general anesthesia, should be considered alongside the anatomic considerations and specific chin deformity when electing the appropriate augmentation technique [ ].
Procedural technique: injectable fillers
Preoperative Planning
A full evaluation of the chin includes its relation to the nose, lips, teeth, and neck, as well as all components of skin and supporting skeletal, muscular, and soft-tissue structures [ , ]. Physical examination should include facial evaluation both at rest and in motion [ , , ]. Photographs of at least 3 views should be obtained, including the profile bilaterally, oblique views bilaterally, and a frontal view [ , ]. The chin itself should be evaluated in all anatomic dimensions of projection, height, and width. There are several guidelines that can be used to evaluate ideal chin projection. The Gonzalez-Ulloa line, for example, is a vertical line that extends from the nasion downward, perpendicular to the Frankfurt plane (a line from the inferior orbital rim to the superior margin of the external auditory meatus) [ ]. The ideal chin projection according to this evaluation should meet or fall just short of this line [ , ]. A simpler method describes that for men, the chin pogonion projection should be in line with the lower lip vermillion border, whereas in women, it should be 1 to 2 mm behind the lower lip vermillion border [ , ]. With regard to width, the ideal proportions for women are in line with the width of the medial canthi, and for men are in line with the oral commissures [ ]. Regarding chin height, the ideal facial alignment should be divided into equal thirds: hairline to nasion, nasion to subnasale, and subnasale to menton [ , ].
In addition to anatomic considerations, a detailed history, including clinical history, past trauma, orthodontic treatment, or oral surgery is essential. History of any prior injectable treatments and response to treatments should also be elicited [ , ]. Clinicians should also inquire about any upcoming dental procedures or procedures that may have occurred in the preceding week, as some recommend postponing injections to minimum 1 week, and sometimes 2 weeks, from any dental procedures.
Prep and Patient Positioning
Prior to injection, any makeup should be removed. Topical anesthetic cream may be applied, if the patient desires, 30 to 40 minutes prior to injection; however, is not a necessity for all patients. A semirecumbent position may be comfortable for patients, as well as provide a posterior support for the head throughout the procedure, in order to minimize movement. The areas to be injected should then be carefully cleansed with an antiseptic solution (such as chlorhexidine or isopropyl alcohol).
Procedural Approach
The selection of the filler used should allow for both structural support but also appear natural with muscular contraction [ ]. An ideal filler for the chin has a high G prime (G′) to improve shape in 3D proportions but also flexibility to conform to facial movement [ , ]. G refers to the firmness or elasticity of the filler, and products with higher G′ tend to recoil to their original shape, which allows for structural integrity in this location [ ]. Currently, the Food and Drug Administation (FDA) has approved 2 dermal fillers for use in the chin—Juvederm Voluma XC (Allergan plc, Dublin, Ireland) and Restylane Defyne (Galderma, Uppsala, Sweden) [ ].
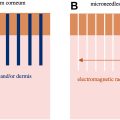
There are many different approaches to chin augmentation with filler, and ultimately, the injector’s preference and practices will influence product selection, as well as injection technique. Centrally, filler injections into the chin are performed in a layer deep to the mentalis muscle, usually with a bolus technique using a needle, as opposed to a cannula. Several smaller supraperiosteal depots injected lateral to the midline to both round out the chin, as well as create a smooth transition are also commonly performed [ , ]. The prejowl sulcus can be addressed with subdermal fanning of the filler, either with a needle and massage, or with cannula [ , , , , ]. Manual molding frequently throughout the procedure for further shaping of the area being treated is often recommended [ , ]. Care should be taken to avoid the mental foramen, through which the mental nerve, artery, and vein traverse, which can be found approximately 1.5 cm superior to the mandibular border in line with the first and second premolar [ ]. In addition, when injecting in the peri-jowl region or on the mandibular body, care should be taken to avoid the facial artery [ , ]. One must be mindful that the facial artery crosses the inferior border of the mandible anterior to the insertion of the masseter, running deep and branching into the superior and inferior labial arteries [ , , ]. In the area of the lateral jawline, it can be avoided by injecting in a subdermal plane [ ].
Immediate Postprocedural Care
While injecting and immediately afterward, it is important to observe the color of the skin. Indications of an abnormal reaction might include sudden pain, local blanching, or livedo. In any of these instances, injections should be stopped for rapid reassessment and intervention. Otherwise, firm pressure, with a folded gauze and flat palm, may be applied to the injection area to control any mild local, pinpoint bleeding. Cold compresses may be applied for pain relief and to minimize bruising [ ]. Patients should be made aware that bruising and swelling may occur, in addition to a sensation of soreness in the area, sometimes pronounced with mastication when injecting on or near the jawline. This will typically resolve within several days to 1 week.
Clinical results in the literature
There is a relative paucity of comparative evidence between the various modalities of chin augmentation, and among the different injectable fillers. A recent systematic literature review examining studies of HA filler for chin augmentation found overall high patient satisfaction among 917 patients included across all studies, with a relatively low complication rate [ ].
Vanaman and colleagues described their experience with high-viscosity HA dermal fillers (Restylane Lyft; Galderma SA, Lausanne, Switzerland; Juvederm Voluma XC, Allergan, Inc, Parsippany-Troy Hills, NJ, USA), in addition to calcium hydroxyapatite fillers (Radiesse (+), Merz North America, Inc, Raleigh, NC, USA) in a review of chin augmentation [ ]. Their techniques employed no more than 1 to 2 mL of filler total with supraperiosteal injections performed with a needle in the midline, several smaller supraperiosteal depots lateral to the midline to round out the chin. Cannula was employed if softening of the prejowl sulcus was necessary [ ].
One study aimed to assess the use of a chin and jawline grid as a guide to nonsurgical treatment with a high G′, high cohesivity filler. In addition to the grid guideline, this study employed cannula technique among 30 patients, injecting 0.1 to 1.5 mL of filler in the chin apex, 0.3 to 0.7 mL to the labiodental sulcus, and 0.1 to 1.5 mL along the jawline. Ninety-six percent of patients rated their appearance after treatment as “much improved” or “very much improved” [ ].
In another international study, Chen and colleagues employed a stepwise specified injection technique using a high elasticity HA injectable for chin augmentation. In this retrospective study among 326 patients, HA filler was first injected supraperiostially at the paragonion close to the inferior border of the mandible and roughly perpendicular to the nasal alar or medial canthus with a 27-gauge needle [ ]. This was followed by needle bolus at the pogonion. Finally, a 25-gauge, 3-cm cannula, and fanning technique were used at the junction of the pogonion, menton, and paragonion to increase volume and smoothen [ ]. Similarly, for individuals with a prejowl sulcus, a cannula was used to inject filler for softening. In this study, with a mean injection volume of 1.85 mL of HA filler, the shape and contour of the chin was significantly improved in all patients with durable improvement at 6-month follow-up by the authors.
Beer and colleagues aimed to assess the effectiveness and safety of VYC 20-L (Juvederm Voluma XC; Allergan plc, Dublin, Ireland) to address volume deficit and retrusion in the chin and prejowl sulci using an evaluator-blinded delayed treatment-controlled study design [ ]. Assessments were performed at 6 months and 12 months, including both treatment-blinded investigator and participant assessments and self-assessments. 27G one-half -inch needles were used for supraperiosteal and/or subcutaneous injections into the pogonion, menton, and prejowl sulci, along with 25G 1.5 inch cannulas in the menton and prejowl sulci. Almost all patients (99.3%) were treated at the pogonion, 77.8% at the menton, and 87.5% at the prejowl sulci, with an average treatment volume of 2.6 mL for initial treatment, and 1.4 mL for follow-up treatment. Injection volumes were similar among treatment and nontreatment participants. Participants were deemed responders if they had at least a 1-point improvement in their Allergan Chin Retrusion Scale (ACRS) score, which was observed in 56.3% of the treatment group at 6 months ( P =.0019). The evaluating investigators rated 91.2% of participants as “improved” or “much improved” in the treatment group at 6 months with durable results at 12 months. Approximately 87% of participants in the treatment group rated themselves as “improved” or “much improved” at 6 months [ ].
Marcus and colleagues employed similar methods to assess Restylane Defyne (Galderma, Uppsala, Sweden) for augmentation and correction of chin retrusion [ ]. In this randomized, evaluator-blinded, parallel group, nontreatment-controlled study across 11 centers, 107 patients with mild to moderate chin retrusion were treated, with 33 nontreatment controls. Follow-ups were performed at 3 days, 12, 24, 36, and 48 weeks after treatment. Injections were performed using a 27G one-half inch needle with the investigator’s chosen technique. Responders were participants with a greater than 1-point improvement from baseline on the Galderma Chin Retrusion Scale and esthetic improvement was also assessed using the Global Aesthetic Improvement Scale by evaluators and patients alike. The mean total volume injected was 3.6 mL including initial treatment and 4-week touch up. Injections at both the pogonion and the surrounding areas were performed using both serial puncture and/or linear retrograde, and specifically at the pogonion, supraperiosteal depot technique was used, with a mean treatment volume of 1.67 mL. Eighty-one percent of the treatment group were rated responders at 12 weeks ( P <.001), with high patient satisfaction rates. Ninety-six percent of treatment participants remained improved at 48 weeks. [ ].
A prospective, single-blinded, randomized controlled study across 10 international sites was performed to assess the safety and effectiveness of VYC-25L (Juvederm Volux; Allergan plc, Dublin, Ireland) in restoring and creating facial volume in subjects with chin retrusion [ ]. Treatments were performed using a 27G 13 mm needle according to investigator’s evaluation and technique. Subjects were seen at 1, 3, 6, 9, and 12 months for safety and effectiveness visits and 3 and 14 days for safety visits. Here, the primary effectiveness was determined through computer-facilitated programmed image analysis comparing the mean change from baseline between treatment and controls in the glabella-subnasale-pogonion angle. Secondary effectiveness was esthetic improvement as rated by investigators and subjects using the Global Aesthetic Improvement Scale (GAIS) as well as 3 Facial Appearance, Quality of Life, and Adverse Events (FACE-Q) scales. Among 90 subjects in the treatment group and 29 subjects in the control group, treatment characteristics were similar with nearly all receiving initial treatment at the pogonion, mentum, and prejowl sulci and 76% receiving treatment at the sublabial crease. Treatment volumes were also similar in both groups with 2.28 mL in the treatment group on average at initial treatment, and 1 mL at 1-month touch-up on average. The mean change in the glabella-subnasale-pogonion angle was 2.12° in the treatment group compared with −0.38° in the control group at month 3, and this gradually declined over time in both groups but remained 1.28° at 12 months for the treatment group. Over 90% of subjects had improved/much improved GAIS scores and responses on FACE-Q Satisfaction and Psychological Well-Being Scales [ ].
Overall, while comparative studies are lacking, published data show safety and efficacy of high G′ filler targeting the pogonion, menton, and pre-jowl sulci to smoothen the chin and improve retrusion. Further large-scale and comparative trials are needed to help further guide technique and product selection.
Potential complications and management
Common complications encountered with dermal fillers include injection site reactions such as bruising, swelling, pain, and erythema [ , , ]. Across these studies in the literature, the majority of patients experienced mild to moderate injection site reactions immediately following the injection, such as some tenderness at the site, and less frequently erythema or swelling [ , , ]. A minority of patients experienced asymmetry following filler injections, which can be addressed through filler correction of asymmetry and/or neurotoxin injections into the mentalis. This may improve the esthetic appearance and also the longevity of the filler [ ]. Treatment-related adverse events, such as delayed nodules, and more rarely infection, have been cited in a handful of patients [ , ]. When present, hyaluronidase can be used for delayed-onset nodules and as shown improvement [ ].
Serious complications are rare; however, the most severe potential risk of injections is vascular compromise either secondary to intra-arterial injection, injection-related edema, or arterial compression [ ]. Although exceedingly rare, it has been reported to occur on several occasions [ , ]. Risk of vascular compromise can be mitigated by periosteal injections and careful consideration of the anatomy, particularly near the mental foramen, while the chin is not considered a high risk area traditionally, there can be considerable variation and anastomoses in this region and prompt recognition and management of occlusion are essential [ ]. This should be addressed with the injection of the area with ample hyaluronidase, and simultaneous massage, warm compresses, and possibly topical nitroglycerin [ , ]. The patient should be continuously assessed until the color and pain improves in the region, as repeat cycles of hyaluronidase injections, massage, and topical therapies may be necessary. It may be beneficial to have the patient remain in the office for at least 30 minutes to be re-evaluated and confirmed safe by the physician before they leave [ ].
Summary
Chin augmentation can be accomplished by a variety of surgical and minimally invasive techniques. HA fillers are a safe and well-studied treatment to optimize chin dimensions and alignment. Providers should select a high G′ and high cohesivity filler to provide appropriate structural support to the region. While injection techniques can vary, most injectors target the pogonion, menton, and prejowl sulci to create shape and balance and inject more deeply centrally and more superficially in the subcutaneous region moving more laterally. Chin filler injections can be performed safely with careful consideration of the location and depth of vessels, but swift recognition and management of potential vascular occlusion is also critical. Future research can help elucidate optimal filler choice and injection strategies to minimize occlusion risk.
Clinics care points
- •
Optimizing chin shape and structure plays a key role in facial balance, symmetry, and youthfulness. While several invasive techniques can help to augment the chin, hyaluronic acid fillers are a minimally invasive and low risk treatment option.
- •
Proper anatomic evaluation and assessment of chin position is crucial for procedural planning. High G′ and high cohesivity fillers such as Restylane Lyft, Defyne or Contour, and Juvederm Voluma or Volux offer the necessary firmness and structure needed to support the chin.
- •
Chin filler treatments are tolerated well overall, with swelling and bruising being the most common adverse events. While rare, vascular occlusion must be promptly identified and managed.
- •
While clinical studies evaluating filler overall show efficacy and high treatment satisfaction, further large-scale comparative studies are needed to elucidate product choice and ideal treatment techniques to enhance esthetic outcome and minimize risks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree