19. Chemical Peels
George Broughton II, Ahmed M. Hashem, Christopher Chase Surek, James E. Zins
PREOPERATIVE EVALUATION
■ Consultation with the patient to establish realistic goals and expectations
■ Does the patient have an indication for chemical resurfacing?
• Superficial or deep rhytids/photoaging
• Preneoplastic or neoplastic lesions such as actinic keratoses and lentigines
• Underlying skin disease such as acne
• Pigmentary dyschromias
• Demarcation lines secondary to other resurfacing procedures
■ Any contraindications (Box 19-1)?
Box 19-1 CONTRAINDICATIONS FOR CHEMICAL PEELS
Absolute
• Poor physician-patient relationship
• Lack of psychological stability and mental preparedness
• Unrealistic expectations
• Poor general health and nutritional status
• Isotretinoin therapy within the last 6 months*
• Complete absence of intact pilosebaceous units on the face
• Active infection or open wounds (such as herpes, excoriations, or open acne cysts)
Relative
• Medium-depth or deep resurfacing procedure within the last 3-12 months*
• Recent facial surgery involving extensive undermining, such as a facelift*
• History of abnormal scar formation or delayed wound healing
• History of therapeutic radiation exposure
• History of particular skin diseases (such as rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis, and vitiligo) or active retinoid dermatitis
• Fitzpatrick skin types IV, V, and VI*
*These contraindications are for medium- and deep-depth peels and do not apply to touchups.
■ Comprehensive medical and surgical history and physical examination
• Bleeding complications/risks from prescription and herbal medicine
■ Is the patient taking isotretinoin, birth control pills, or immunosuppressants?
• Is the patient pregnant?
• Patients having a history of cold sores require herpes simplex prophylaxis.
• All patients should receive antiviral prophylaxis regardless of history.
• Does the patient have a history of hypertrophic or keloid scars?
• Does the patient have a history or risk of hepatitis or HIV?
• Does the patient have certain cutaneous diseases in the operative site?
TIP: Patients with rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis, or vitiligo may be at increased risk for postoperative complications, including disease exacerbation, prolonged erythema, contact hypersensitivity, or delayed healing. Patients with rosacea have a vasomotor instability and may develop an exaggerated inflammatory response.
• What skin regimens have been used and what were the results?
• If patient has history of skin rejuvenation, what type of rejuvenation was done, what were results, and did problems occur?
• Identify dyschromias and determine the best depth of peel (Box 19-2).
Box 19-2 PEEL RESULTS FOR DIFFERENT DYSCHROMIAS
| Superficial Peel | Medium-Depth Peel |
| Excellent Results | Excellent Results |
Ephelides | Ephelides |
Epidermal hyperpigmentation | Epidermal melasma |
Epidermal melasma | Epidermal postinflammatory hyperpigmentation |
Lentigines simplex | |
Senile lentigines | |
| Variable Results | Variable Results |
Lentigines simplex | Dermal and mixed melasma |
Mixed (epidermal and dermal) melasma | Dermal and mixed postinflammatory hyperpigmentation |
Mixed postinflammatory hyperpigmentation | Seborrheic keratoses |
Senile lentigines | |
| Poor Results | Poor Results |
Dermal melasma | Nevi |
Dermal postinflammatory hyperpigmentation | Some exophytic seborrheic keratoses |
Junctional nevi | |
Seborrheic keratoses |
• Determine depth of pigmentation using a Wood lamp.
► View patient in darkest room possible.
► Hold lamp 8-12 inches from patient’s face and rotate wrist to change angles.
► Under a Wood lamp, epidermal hyperpigmentation is bright and accentuated. Deep dermal hyperpigmentation is not seen or is less pronounced.
TIP: The worse the patient looks under a Wood lamp, the more superficial the pigmentation.
• Determine and document patient’s skin type (using the Fitzpatrick skin type classification)1 and photoaging grouping (Tables 19-1 and 19-2), degree of actinic damage, sebaceous gland density, dyschromias, suspicious lesions, and scarring.
Table 19-1 Fitzpatrick Skin Type Classification
| Skin Type | Characteristics | Sun Exposure History |
I | Pale white, freckles, blue eyes, blond or red hair | Always burns, never tans |
II | Fair white, blue/green/hazel eyes, blond or red hair | Usually burns, minimally tans |
III | Cream white, any hair or eye color | Sometimes burns, tans uniformly |
IV | Moderate brown (Mediterranean) | Rarely burns, always tans well |
V | Dark brown (Middle Eastern) | Rarely burns, tans easily |
VI | Dark brown to black | Never burns, tans easily |
Table 19-2 Glogau Photoaging Scale
| Description | Features | |
| I (mild) | Wrinkles not present or minimal | Early photoaging No keratoses, pigmentary changes Patient generally wears minimal or no makeup Typical age range: 20s-30s |
| II (moderate) | Wrinkles present only when skin is in motion | Early to moderate photoaging Early actinic keratoses Sallow color Smile lines begin Patient generally wears some makeup Typical age range: Late 30s-40s |
| III (advanced) | Wrinkles present when skin is at rest | Advanced photoaging Dyschromias, telangiectasias Actinic keratoses Persistent wrinkling Patient always wears makeup Typical age range: 50s or older |
| IV (severe) | Only wrinkles | Severe photoaging Yellow-gray skin Dynamic/gravitational wrinkling throughout Actinic keratoses ± skin malignancies No normal skin Patient wears makeup, but coverage is poor (it cakes or cracks) Typical age range: 60s or older |
• Point out any skin excess and gravitational changes that will not be corrected by chemical peels.
■ Standard preoperative photographs for surgical planning (see Chapter 3)
■ Presurgical arrangement and understanding about financial responsibilities for revisions
■ Analysis and operative planning based on patient’s desires, clinical examination, and photographs.
NONFACIAL PEELING
INDICATIONS
■ Back
• To remove sunburn freckles across the shoulders and upper back
• To improve acne scars
• To improve postinflammatory hyperpigmentation from acne
■ Chest
• To improve hyperpigmented macules, usually lentigines or flat seborrheic keratoses and sunburn freckles
• To improve acne scars, especially in areas of hypopigmented scars and hyperpigmented actinic damage
• To improve postinflammatory hyperpigmentation from acne
• To improve fine wrinkling (usually vertical lines over the sternum)
■ Hands and forearms
• To improve hyperpigmented macules (age spots)
• To improve superficial wrinkling
• To improve rough texture
SOME KEY POINTS2
■ It usually takes nonfacial areas 50%-100% longer to heal than the face. Patients need to be sure they have time to undergo this type of therapy before having it done.
■ Dermal peels on the arms, hands, neck, and chest are more prone to scarring or abnormal textural changes. It is safer to perform epidermal peels in these areas. Dermal hyperpigmentation and most types of scars on nonfacial areas should not be treated with chemical peeling, because they will not improve significantly.
■ Most nonfacial peels are done to improve fine wrinkling and blotchy discoloration (including age spots). One intraepidermal peel is usually not sufficient to give these patients their best results. Nonfacial peels are usually repeated several times to achieve the best response.
■ Most nonfacial peels are performed on large areas of skin (a larger surface area than the face). If a peeling agent with potential toxicity is used, there is a greater risk of developing a systemic reaction.
■ The larger the area treated and subsequently wounded, the more difficult it is for patients to care for it, and the greater the chance of a complication, particularly premature peeling or infections.
INFORMED CONSENT3
Recommended items to be included in the informed consent:
■ No warranties, guarantees, or special contracts about the success and longevity of the procedure
■ Review of the healing process and how the patient will look and for how long
■ Possible need for additional surgeries/procedures
■ Complications, especially pigment changes (hyperpigmentation and hypopigmentation), scarring (including keloids, hypertrophic scarring), fever blisters (herpes simplex) activation, infection, milia, and “pink areas” (erythema)
■ Review (with the patient) the things chemical peels can and cannot do (Box 19-3).
Box 19-3 THINGS CHEMICAL PEELS CAN AND CANNOT DO
| Things Chemical Peels CAN Do | Things Chemical Peels CANNOT Do |
Correct sun damage (actinic degeneration) Flatten mild scarring Remove rhytids Improve irregular hyperpigmentation | Decrease pore size—chemical peels might increase pore size Improve skin laxity Improve deep scarring Totally remove hyperpigmentation in dark-skinned whites, Asians, and blacks Remove vascular lesions |
PEEL PREPARATION
■ Chemical peels may be classified as:
• Superficial (epidermal injury)
• Medium-depth (superficial dermal injury to the papillary dermis)
• Deep (mid-dermal injury to the reticular dermis).
■ Degree of injury is dependent on:
• Chemical agent used
• Concentration
• Time of application before neutralization
• Number of coats and the amount of peeling agent placed with each application (i.e., degree of wetness of the applicator)
Fig. 19-1 is a review of skin anatomy. The different chemical peel formulations commonly used are summarized in the section Common Chemical Peel Agents.
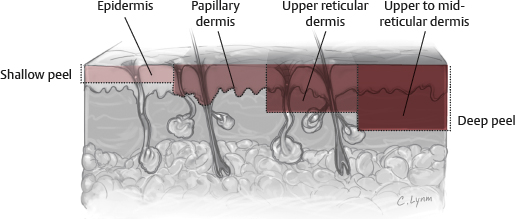
Fig. 19-1 Skin anatomy and chemical peel depth.
COMMON CHEMICAL PEEL AGENTS
GLYCOLIC ACID4
■ The product
• Not light sensitive: Does not need to be stored in a dark bottle
• Very stable (>2 years)
• Deliquescent (absorbs moisture): Must be kept in a tightly capped bottle
■ Features
• Most practitioners use 30%-70% glycolic acid and neutralize the skin with a bicarbonate solution or rinse with water at the onset of erythema.
• Caution must be used, because uneven peeling and dermal wounding can occur.
• White, scattered frosting indicates epidermal necrosis and dermal inflammation.
• Moy et al5 found a protocol of 10%-15% glycolic acid applied twice daily and 50%-70% glycolic peels given weekly for 4 weeks effective in the treatment of fine wrinkles and superficial lesions. Van Scott and Yu,6 using a similar protocol for 10 months, reduced wrinkles in 21 of 27 patients.
• Glycolic peels are less effective for solar keratoses and solar lentigos.
• Piacquadio7 concluded that retinoids, light TCA peels, and glycolic lotion represent a better consumer value than glycolic acid peels.
TIP: Glycolic acid is an alpha-hydroxy acid (AHA) made from sugar cane. Other AHAs include lactic acid (from sour milk), malic acid (from apples), citric acid (various fruits) and tartaric (from grape wine).
JESSNER SOLUTION4
Formulated by Dr. Max Jessner. The combination allows decreasing the concentration and toxicity of each ingredient.
■ The product
• Contains resorcinol, salicylic acid, lactic acid, and ethanol
• Retains strength for up to 2 years if container is opened for only 5 minutes per month
• Light and air sensitive! May develop a salmon-colored tone on exposure to light and air—store in a dark amber bottle with a tight cap
■ Features
• It creates a uniform-depth peel that results in an excellent exfoliation.
• It is useful in treating hyperpigmentation by increasing epidermal turnover and yielding a decrease in the number of melanin-containing keratinocytes.
• Complications are rare because of the limited penetration.
• Use is limited to the face because of the potential for salicylate (tinnitus, headache, nausea) or resorcinol (methemoglobinemia and hypothyroidism with prolonged use) toxicity.
• It is thought to break the intracellular bridges between keratinocytes and has the capacity to remove the epidermis.
• Used alone, it causes superficial epidermal peel.
• Depth is controlled by number of applications.
• No neutralization is needed.
• It can be combined with TCA for a medium peel.
• Application first causes a faint erythema followed by a more pronounced erythema on second application. After further applications, a frost begins to form. Significant exfoliation is seen for 8-10 days when a frost is achieved; however, no weeping or crusting is seen, because it remains an intraepidermal peel.
TRICHLOROACETIC ACID (TCA)
■ The product
■ Not light sensitive
• Refrigeration not needed
• Stable for at least 23 weeks in an opened container
• 20%-100% TCA stored in an unopened TCA-resistant clear plastic container for 2 years—TCA concentration within 3% of the labeled strength
• Colorless and clear
• Free of precipitate
■ Features
• TCA is commonly used in 30%-35% concentration for medium-depth peeling penetrating into the upper reticular dermis.
• The concentration, skin preparation, pretreatment skin type, and method of application contribute to the peel depth obtained.
• An intraepidermal, epidermal, or papillary dermal peel can be successfully obtained with 20% TCA. Superficial papillary dermal necrosis was shown histologically in a porcine model at 24 hours using 20% TCA; however, no change in the number of fibroblasts or elastic fibers was detected at 28 weeks after the peel.8
• Dolezal9 suggested four levels of superficial and intermediate TCA peels.
► Level 0: Has no frost, and the skin looks slick and shiny, which represents removal of the stratum corneum.
► Level 1: Has an irregular, light frost with some erythema; this is an intraepidermal peel that creates 2-4 days of light flaking.
► Level 2: Has a pink-white frost, which suggests a full-thickness epidermal peel, and heals in about 5 days.
► Level 3: Has a solid white frost and is thought to extend into the superficial retinacular dermis. Johnson et al10 described an additional sign of “epidermal sliding” for a papillary dermal peel.
CROTON OIL PEEL
■ The product
• Initially utilized by “lay peelers.” The formula was obtained by Tom Baker in the early 1960s. The original Baker Gordon formula utilized high concentrations of phenol and croton oil (50% phenol, 2.1%-2.4% croton oil). Although excellent results could be obtained, long-term hypopigmentation became a problem and croton oil peeling fell into disfavor.
• Phenol-croton oil peeling regained popularity in the early 2000s due to the work of Hetter11–14 and later Stone and colleagues.15–16 Hetter refuted a number of the concepts espoused by Baker (phenol-croton oil peeling is an “all or none phenomenon,” and decreasing concentrations of phenol led to deeper injury). But most importantly both Hetter and Stone demonstrated by reducing the concentration of phenol and croton oil, complications could be significantly reduced while the results could be maintained.
■ Features
• Stone suggested that the depth of peeling is dependent on the concentration of both the phenol and croton oil, whereas Hetter suggested that croton oil is the critical agent determining peel depth.
• Ozturk et al17 stated that a concentration of 33% phenol and 1.1% croton oil is associated with acceptable side effects in Fitzpatrick I and II skin types, especially in the perioral area.
• Gatti et al18 stated that treatment of the lower lids with phenol 22% and 1.1% croton oil is effective in treating hyperpigmentation and fine lines.
► Standard concentration 88%
► Used alone causes medium-depth peel
► Causes keratin protein coagulation
► Rapidly absorbed through skin, metabolized in the liver, excreted renally
► Can lead to renal failure, hepatotoxicity, directly irritates myocardium causing arrhythmias
► Requires cardiac monitoring and testing of kidney, liver, cardiac function
► Hypopigmentation and scarring significantly minimized by reducing concentrations of phenol and croton oil.
► Peel in subunits, allowing 15-20 minutes per site between units.
PHENOL-CROTON OIL AND TCA PEELS
■ Although traditionally TCA was considered a medium-depth peeling agent and phenol-croton oil a deep peeling agent, this has clearly been disproven by Hetter and Stone. Using modern peeling understanding, both agents can peel in subunits to superficial (epidermal), intermediate (papillary dermal), or deep (mid-reticular dermal) levels depending on:
1. Concentration of agents used
2. Number of applications
3. Wetness of the applicator
■ Most critical to the level of the peel is the degree and nature of the frost obtained.
• Pink-white frost suggests injury to the papillary dermis; dense white frost suggests superficial reticular dermal injury, and gray-white suggests mid-reticular dermal injury.
■ Therefore, TCA and croton oil peels should not be thought of as intermediate or deep peeling agents only, but as agents that can peel to any depth desired. This significantly increases their respective versatility.
SALICYLIC ACID
■ The product
• Made into a paste and spread over the skin using a tongue depressor
• Formula: Salicylic acid powder USP, 50%; methyl salicylate, 16 drops; Aquaphor, 112 g
■ Features
• The incidence of significant complications is low, and it is easy to use.
• Deep penetration is difficult.
• It is effective for the treatment of hyperpigmented age spots on the hands and arms. Patients will need to have their hands/arms wrapped in plastic wrap and gauze for 48 hours.
• In concentrations of 3%-5% it is keratolytic and enhances topical penetration of other agents.
• It has mild potency as a fungicide.
• Symptoms of salicylate toxicity include ringing in the ears, muffled hearing, dizziness, and/or headache several hours after the peel. Increased water intake and removal of the bandage may improve mild salicylism.
• Application of salicylic acid will cause mild stinging for 1-3 minutes followed by superficial anesthesia to light touch. After 5 minutes of air drying, the face should be washed with water.
• Peeling starts around days 3-5 and continues until day 10.
BETA-LIPOHYDROXY ACID19
■ The product
• Eight-carbon fatty chain linked to a benzene ring (derivative of salicylic acid)
• Available in formulations of 5% and 10%
■ Features
• The safety profile is good with less skin irritation, compared with glycolic acid, and neutralization is not required.
• It reduces melanosome clustering and epidermal pigmentation and is used for treatment of photoaged skin and acne.
• It increases the skin’s resistance of UV-induced damage.
• It has antibacterial and antifungal effects.
• The corneosome-corneocyte interface is targeted to cleanly detach individual corneosomes, preventing desquamation in clumps and resulting in skin smoothness.
KEY POINTS FOR ETHNIC SKIN
■ Ethnic skin may respond unpredictably to chemical peels regardless of phenotype.
• Latino and Hispanic patients are prone to an increased incidence of melasma and postinflammatory hyperpigmentation, and chemical peels should only be approached with caution in this patient population. Prolonged pretreatment suppression with 4% hydroguinone is critical.
■ Consider modifying the peel technique: Spot treat lesions instead of treating the entire face.
■ Indications
• Dyschromia
• Acne
• Scarring
• Postinflammatory hyperpigmentation
• Melasma
• Pseudofolliculitis barbae
■ Chemical peel formulations considered safe to use in ethnic skin include:
• Beta-lipohydroxy acid: 5%-10%
• TCA: 10%-20%
• Glycolic acid: 20%-70%
• Salicylic acid: 20%-30%
• Lactic acid
• Jessner solution
PRECONDITIONING THE SKIN: “PRIMING”
■ Preparation of patients may include oral antibiotics and antivirals, facial cleansing, and some preprocedure skin creams. Light peels that only injure the stratum corneum often require no preprocedure prophylaxis, whereas deeper peels may place susceptible patients at higher risk of herpetic outbreaks and should be covered with an appropriate antiviral agent. Skin preparation may include vigorous cleansing with an exfoliant to remove oils and debris.
■ For medium to deep peels: Patients should be instructed to start a vitamin A (retinoic acid 0.1% cream daily for a minimum of 2 weeks before the peel) and glycolic acid skin conditioning program for 6 to 8 weeks before the procedure. Preconditioning the skin causes treated skin to heal faster by 3-4 days by increasing its metabolism—from accelerated cellular division and new collagen formation.20–22
TIP: All-trans-retinoic acid (tretinoin) will speed epidermal healing and enhance the effect of the peel.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




